Abstract
Objectives
The principal aim of our study was to establish concordance between post-mortem CT (PMCT) and forensic standard autopsy (SA) in detecting lesions according to different anatomical regions. A secondary aim was to determine the efficacy of PMCT in showing lethal lesions.
Methods
PMCTs were compared with autopsies in 236 cadavers in different contexts of death. PMCT findings were assessed by two independent radiologists.
Results
Concordance between PMCT and autopsy was almost perfect in showing skull, basal skull and hyoid bone fractures as well as in detecting facial, vertebral or pelvic fractures. Both examinations were discordant in demonstrating some intracranial injuries, vascular or organ wounds (more findings showed by autopsy), as well in showing free air in anatomical cavities (more findings detected by PMCT). Moreover, PMCT was effective in determining lethal lesions in the context of craniofacial trauma or after a gunshot wound. Concordance between the findings of the two radiologists was almost perfect for each type of lesion.
Conclusion
PMCT could be considered as effective as SA in determining the cause of death in certain traumatic events. It was also effective in showing lethal lesions and could be a useful tool in reducing the number of SA.
Key Points
• Post-mortem CT is increasingly performed as an alternative/adjunct to formal autopsy.
• More modern CT systems provide greater anatomical scope.
• PMCT can usually determine the cause of most deaths following trauma.
• Prospective studies are still required to establish an algorithm for forensic CT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Post-mortem CT (PMCT) has been introduced in Denmark [1], the UK [2], the USA [3], Sweden [4], Australia [5] and Switzerland [6]. This procedure is objective, rapid and the resultant data are safely storable for future reference. Major studies reporting the accuracy of PMCT are limited [1–7]. Initial investigations have demonstrated that PMCT can guide forensic autopsy and determine cause of death in many cases. It remains fundamental to determine if CT could be sufficient to detect lethal lesions in some contexts of death, thereby avoiding SA.
At the Rouen University Hospital Department of Forensic Medicine, PMCT was performed before autopsy in order to obtain anatomical–radiological correlations. This evaluation was also justified because recent technical advancements in PMCT have improved the information they can provide to forensic pathologists. The principal aim of the study was to determine the concordance between PMCT and autopsy in detecting traumatic or non-traumatic lesions according to the different anatomical regions. Secondary aims were to determine the efficacy of PMCT in showing lethal lesions proved by autopsy, as well to establish the interobserver agreement between the two radiologists.
Material and methods
Materials
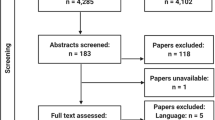
This study was conducted prospectively from January 2006 to August 2011 at Rouen University Hospital, France. During this period, 236 PMCTs were performed before external examination and autopsy (159 male cadavers, 77 female; age range 20 weeks to 78 years; mean age 42 years). All PMCT performed in our department were included. However, the first 66 PMCT (before January 2010) were not performed in consecutive cadavers because CT was not available.
The context of death was a traumatic event (other than gunshot or stab wounds) in 62 cadavers and gunshot wounds, stab wounds, hanging, asphyxia other than hanging, drowning, carbonisation in 26, 17, 11, 11, 22, 21 cadavers, respectively (Table 1). In 66 cadavers, either non-traumatic lesions were observed or no lesions were detected at all.
The mean delay between declaration of death and imaging was 6 ± 3 days, and that between PMCT and autopsy was 18 ± 1 h.
Post-mortem CT
All PMCTs were performed the day before autopsy. The examinations were performed on a 16-detector row system (Light Speed Ultra unit, GE HealthCare, Chalfont St Giles, UK) until December 2009 (92 cases, of which 62 were before autopsy) and since then on a 64-detector row unit (Discovery, GE HealthCare) (174 cases). Examination starts with an anterior–posterior and lateral scout views. Typical parameters are (for the 64-detector row unit) pitch 1.375:1, gantry rotation time 1.0 s, tube voltage 120 kVp, current intensity 200 mA, field of view 50 cm for the entire body including the head. The acquisition time is 3 min, and reconstruction takes about 1 min more. Images are then transferred to a proprietary workstation. Multiplanar software (Reformat, GE HealthCare) is currently being used.
Additional reconstructions can be performed: (a) skull and neck (0.625/0.625 mm) with bone filter (allowing dental CT reconstruction if required), (b) lung (0.625/0.625 mm) with dedicated filter, (c) pelvis–lower limb–feet (slice thickness 1.25 mm, space 1.25 mm, bone filter). For areas of special forensic importance (base skull fractures, teeth, foreign bodies), additional 0.625-mm-thick images can be acquired. During each CT acquisition, approximately 800 native phase images were collected. Multiplanar reconstructions (MPR) were performed in three dimensions (axial, coronal, and sagittal). The reconstructed slice thickness and overlapping sections were adapted to reconstruct each segment in less than 100 images. Axial reconstructions of the skull bone and the lung with adapted windows were routinely performed; other MPR were made in cases of anomalies. Additional reconstructions centred on the brain were often required (slice thickness 2.5 mm and appropriate filter). Lastly, 3D volume rendering technique (VRT) reconstructions were routinely performed for the entire skeleton. For each CT acquisition, the digitally acquired scout radiographs and reconstruction were transferred to a CD-ROM and a check list was completed.
Autopsy
Autopsies were routinely performed by two experienced forensic experts. Anatomical dissection was carried out according to European recommendations (Recommendation no. R(99)3 of the Committee of Ministers to Member States on the harmonisation of medico-legal autopsy rules. Council of Europe, Committee of Ministers). The final report was completed by both forensic experts. The examination of the brain after autopsy was performed by a forensic pathologist after fixation with formalin. No imaging of the isolated, formalin-fixed brain was performed.
Radiological evaluation and data analysis
Post-mortem CT was assessed by a radiologist who was aware of the context of death (e.g. gunshot wound, hanging). A second reading was performed by a second radiologist who was blinded to the results of the previous radiological analysis, but had knowledge of the autopsy findings. Both radiologists had previous experience in reading post-mortem images. Detailed radiological evaluation was known to the two forensic pathologists at autopsy. However, only findings discovered during standard autopsy (SA) without performing additional dissection or particular techniques guided by PMCT (e.g. research of pneumothorax, gaseous embolus) were noticed. We chose to provide the pathologists with detailed radiological evaluations with the aim of increasing autopsy accuracy because if PMCT demonstrated a lesion not routinely searched for by SA additional dissection was performed (but the detected lesion was not considered a finding of the SA). A direct comparison of PMCT and autopsy findings was then performed by both forensic experts after reading the forensic and radiological reports.
Comparison between PMCT and autopsy findings was performed according to anatomical regions of specific lesion sites with the aim of establishing the concordance or discordance between the two examinations in detecting any lesions. SA was not considered the gold standard because PMCT was sometimes able to demonstrate lesions not discovered by autopsy in as much as SA can miss very small lesions and does not always use all specialised manoeuvres (i.e. search for gas embolus, pneumothorax) [7]. For each cadaver, a qualitative evaluation of each lesion was performed: presence or absence of lesions (e.g. fractures, wounds), without specifying their number.
Moreover, PMCT sensitivity in specifying the cause of death was determined: it was established if a lethal lesion discovered by autopsy had been observed on CT. A traumatic lesion was regarded as cause of death only when vital signs were present such as haemorrhagic infiltration, discolouration, soft tissue emphysema, air embolism, fluids or gas in cavities [8]. After autopsy, results of histological analysis were not considered to determine cause of death. When neither autopsy nor PMCT demonstrated any injury and when toxicological analysis showed a lethal dose of a drug, the cause of death was regarded as poisoning.
This study was approved by the public prosecutor. The agreement of the institutional review board of the office of the chief medical examiner was not necessary.
Statistical analysis
Kappa values (with 95 % confidence intervals) were calculated to determine the agreement between PMCT and autopsy in showing the different types of lesions, as well as in specifying the interobserver agreement between the two radiologists. The values were classified as slight (0.01 to 0.20), fair (0.21 to 0.40), moderate (0.41 to 0.60), substantial (0.61 to 0.80) or almost perfect (0.80 to 1.00) [9]. Observations were considered to be concordant when values were substantial or almost perfect.
Results
The first 66 PMCT were not performed in consecutive cadavers unlike the 170 carried out later. In these non-consecutive cadavers, imaging was performed in 24 % of subjects where the context of death was cranial, thoracic or abdominal trauma. When the context of death was gunshot wound, stab wound, hanging, asphyxia other than hanging or drowning, natural death, drowning, burn injury, death by poisoning or sudden infant death syndrome, PMCT was performed in 20 %, 24 %, 18 %, 22 %, 24 %, 14 %, 26 %, 12 % and 23 % of patients, respectively.
Traumatic and non-traumatic lesions
Concordance between PMCT and autopsy was almost perfect in showing skull, basal skull or hyoid bone fractures (Table 2). Concordance between the two examinations was excellent in demonstrating facial, vertebral and pelvic fractures and the number of fractures showed by PMCT was superior to that observed at autopsy. As regards rib fractures, concordance between the two examinations was only substantial and autopsy demonstrated more lesions than PMCT. Discordance was observed in demonstrating intracranial injuries such as subdural haematomas, as well as pulmonary, vascular or abdominal wounds. In these cases, the number of lesions demonstrated by PMCT was inferior to that determined by autopsy. Similarly, discordance was observed between the two examinations in detecting free air in anatomical cavities.
In some cases, PMCT demonstrated findings that would not be shown by autopsy such as a muscular prosthesis inserted in a calf that allowed identification and a fracture of the dens of the axis.
Cause of death
The sensitivity of PMCT in showing lethal lesions demonstrated by autopsy was recorded according to the context of death (Table 3). PMCT was effective in determining lethal lesions detected by autopsy in the context of craniofacial trauma or gunshot wounds but was less accurate after stab wounds, sometimes showing only indirect signs as effusions in anatomical cavities. After death by hanging, PMCT was effective only when a fracture of the hyoid bone was present. In cadavers with asphyxia syndrome not due to hanging or drowning, PMCT was not accurate, because cause of death was determined in only 2/11 cases (foreign bodies that completely blocked off the larynx).
In the context of natural death, PMCT sensitivity was moderate in showing lethal lesions. PMCT had no usefulness in determining the cause of death in the context of drowning, burn injury, poisoning or sudden infant death syndrome. In all drowning subjects, the only non-specific signs were observed by PMCT as ground-glass attenuation within the lungs, fluid in the airways and the paranasal sinus. Sediments in the paranasal sinus (1 subject) and frothy fluid in the airways (2 subjects) were rarely shown. In charred bodies, no specific sign was observed, particularly in the airways, which could suggest the presence of soot deposits in the airways.
Agreement between both radiologists
Conclusions from PMCT were reliable across examiners because concordance between the findings of the two radiologists was almost perfect or substantial in determining each type of lesion (Table 2).
Further studies are needed to establish an algorithm for forensic examinations in order to determine the context of death in which PMCT or autopsy would be sufficient, including the context in which both examinations could be required. In fact, whereas autopsy can show lesions missed by PMCT, it is able to demonstrate lesions that are not observed at autopsy because some anatomical locations are not routinely dissected or specialised manoeuvres are not routinely performed.
Discussion
In our study, an almost perfect correlation was observed between PMCT and autopsy in showing skeletal injuries as well as fluid and gas effusions in anatomical cavities. Moreover, in the context of cranial traumas and gunshot wounds, PMCT was very accurate in detecting lethal lesions observed at autopsy. Lastly, findings of both radiologists were almost perfect for the determination of each type of lesion.
Concordance between PMCT and autopsy in detecting lesions
We have only determined a correlation between the findings of PMCT and autopsy without establishing PMCT sensitivity because SA did not always appear to be a valid reference for testing the performance of the PMCT [7]. Indeed, during autopsy, some injuries can be diagnosed only after specialised manoeuvres or are too small to be observed. In our study, the concordance between PMCT and autopsy was almost perfect for showing skull fractures (Table 2) that were more frequently detected by PMCT than in a previous study [10], probably because the radiologists were aware of the context of death. For the same reason, these radiologists most often discovered basal skull fractures [10] because these injuries were routinely searched for by additional reconstructions in the context of cranial trauma. Concordance between PMCT and autopsy was less perfect than for skull fractures in demonstrating facial, vertebral or pelvic fractures. PMCT more frequently demonstrated these types of fractures than SA because it was performed without routine dissection of the face, spinal column and pelvis [11]. On the other hand, concordance between the two examinations was only substantial in detecting rib fractures, with more lesions demonstrated by autopsy. This finding is contradictory to some previous results [12], but in agreement with another report [13]. Concordance between the two examinations was also almost perfect in showing fracture of the hyoid bone. Moreover, after PMCT, cervical haematomas were detected in two cases of hanging showing that fracture of the hyoid bone occurred before death [14]. However, few cervical haematomas were discovered by PMCT compared with autopsy [15]. Concordance between PMCT and autopsy was barely substantial in demonstrating some intracranial injuries, particularly subdural haematomas, which confirmed that PMCT is less accurate than autopsy [10]. On the other hand, PMCT was concordant with autopsy in demonstrating cerebral oedema as previously reported [10], as well as in showing brain contusions [1], but contrary to previous findings [10] we did identify some brain injuries smaller than 3 mm. Our results must be treated with caution because the number of contusions was low, the brain was sometimes not sliced during autopsy when histological analysis was further performed and some cadavers were putrefied which subsequently altered radiological examination and macroscopic analysis. Indeed, it was widely demonstrated that post-mortem changes, e.g. internal liquefaction, putrefaction, post-mortem clot and sedimentation of blood components, induce artefacts that should be recognised by radiologists [16]. In our subjects, PMCT and autopsy were substantially concordant in demonstrating pulmonary congestion and oedema but discordant in detecting fluids in the airways, because PMCT very frequently demonstrated this non-specific finding that the autopsy did not confirm in most cases. Discordance between the two examinations was also observed in detecting pulmonary [1], vascular or abdominal wounds attesting to the poor accuracy of PMCT in showing vascular and parenchymal lesions [3, 11]. With PMCT, direct identification of aortic or cardiac rupture was often missed, and only indirect signs were observed such as haemothorax and cardiac tamponade [17]. To overcome the obstacle of the lack of circulation, post-mortem angiography is useful in increasing the detection of vascular rupture [18]. In our study, pericardial effusions were more often observed by CT because effusions that were too small because of putrefaction were not noted at autopsy, whereas these data were present on the autopsy check list. Lastly, PMCT and autopsy were discordant in showing gas in anatomical cavities with more findings shown by imaging [19], because gaseous pockets are not routinely searched for during standard autopsy.
Availability of PMCT for showing lethal lesions demonstrated by autopsy
In our study, PMCT was very effective at demonstrating lethal lesions detected by autopsy in the context of craniofacial trauma as previously reported [1, 11, 14]. In thoracic trauma, PMCT was inferior to autopsy in showing pulmonary, vascular or heart wounds. PMCT was effective at detecting lethal gunshot wounds [20], but less effective after stab wounds, because tracks were more difficult to ascertain [14]. In many cases, cause of death was only suspected because of indirect signs as in the case of effusions [21]. When the context of death was hanging, PMCT sensitivity was excellent in showing fractures of the hyoid bone that were detected more frequently than in a previous study [15]. PMCT was useful in establishing diagnosis of natural death only in some cases because this examination has a poor sensitivity in showing parenchymal lesions and does not demonstrate ischaemic cardiac necrosis and premortem thrombosis unlike magnetic nuclear resonance [17]. Most often, only the probable findings were observed [21, 22] and, in most cases, only non-specific findings were shown, such as tracheal and bronchial liquids, pleural effusions, ground-glass attenuation as well as fluids in the paranasal sinus that can also be observed after inhalation or due to decomposition. PMCT was only of slight interest in our subjects after drowning and CT findings of frothy airway fluid suggesting drowning were only observed in two cadavers [23]. Diagnosis of drowning is difficult to establish, even by autopsy, because only non-specific anatomical findings are observed such as oedema fluid in the nostrils, mouth and airways, pulmonary oedema, water in the lumen of the stomach [24] and biological and histological samples are needed to confirm drowning. In charred bodies, no specific signs were found in our subjects and imaging of soot in the airways was never observed [25].
In our study, PMCT was effective at showing lethal lesions demonstrated by autopsy after trauma and gunshot wound. In these cases, except in circumstances of homicide, PMCT with external examination and toxicological samplings would be sufficient and a full autopsy could be avoided. However, the cause of death is not the only issue that concerns the public prosecutor who may also request a macroscopic assessment of organs and histological analysis. Thus, except in cases of homicide, we could possibly envisage situations where a complete autopsy could be replaced by biopsies guided by PMCT [5] or by more limited surgical procedures. Further studies are required in order to establish an algorithm for forensic examinations to compare results of PMCT, standard autopsy, PMCT with standard autopsy and PMCT with more limited surgical procedures (i.e. heart sampling). However, in all cases, external examination and toxicological analysis must be performed.
Our study has some limitations. PMCT was not routinely performed at the beginning of our study because access to CT was limited. Moreover, pathologists were aware of the PMCT findings before the autopsy which allowed them to perform additional dissections guided by CT. However, only lesions detected by SA without additional dissection were considered in this study. Finally, the second radiologist had knowledge of the autopsy findings before image interpretation and was able to perform complementary reconstructions which increased CT performance.
In conclusion, PMCT should be considered a very useful supplementary tool for forensic autopsy because imaging can detect small injuries that may be missed by traditional autopsy. Because concordance between the findings of both radiologists was almost perfect or substantial, particularly in traumatic cases, autopsy could be avoided in these cases, except in cases of homicide. To our knowledge, this study is the first major French series reported in the literature.
References
Poulsen K, Somonsen J (2007) Computed tomography as routine in connection with medico-legal autopsy. Forensic Sci Int 171:190–197
Roberts ISD, Benamore RE, Benbow EW, Lee S, Harris JN, Jackson A, Mallett S, Patankar T, Pebbles C, Roobottom C, Traill Z (2011) Postmortem imaging as an alternative to autopsy in the diagnosis of adult deaths: a validation study. Lancet 22:1–7
Levy G, Goldstein L, Blachar A, Apter S, Barenboim E, Bar-Dayan Y, Shamais A, Atar E (2007) Postmortem computed tomography in victims of military air mishaps: radiological-pathological correlation of CT findings. Isr Med Assoc J 9:699–702
Ljung P, Winskog C, Perssen A, Lundström C, Ynnerman A (2006) Full body virtual autopsies using a state-of-the-art volume rendering pipeline. IEEE Trans Vis Comput Graph 12:869–887
O’Donnell C, Rotman A, Collett S, Woodford N (2007) Current status of routine postmortem CT in Melbourne, Australia. Forensic Int Sci Med Pathol 3:226–232
Thali MJ, Jackowski C, Oesterhelweg L, Ross SG, Dirnhofer R (2007) VIRTOPSY - the Swiss virtual autopsy approach. Leg Me 9:100–104
Scholing M et al (2009) The value of postmortem computed tomography as an alternative for autopsy in trauma victims: a systematic review. Eur Radiol 19:2333–2341
Saukko P, Knight B (2004) The pathophysiology of death. In: Knight’s forensic pathology, 3rd edn. Oxford University Press, New York, pp 52–97
Landis GR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Yen K, Lovblad KO, Scheurer E, Ozdoba C, Thali MJ, Aghayev E, Jackowski C, Anon J, Frickey N, Zwygart K, Weis J, Dirnhofer R (2007) Post-mortem forensic neuroimaging: correlation of MSCT and MRI findings with autopsy results. Forensic Sci Int 173:21–35
Bolliger SA, Thali MJ, Ross S, Buck U, Naether S, Vock P (2010) Postmortem imaging-guided biopsy as an adjuvant to minimally invasive autopsy with CT and postmortem angiography: a feasibility study. AJR Am J Roentgenol 195:1051–1056
Hong TS, Reyes JA, Moineddin R, Chiasson DA, Berdon WE, Babyn PS (2011) Value of postmortem thoracic CT over radiography in imaging of pediatric rib fractures. Pediatr Radiol 41:736–748
Oberladstaetter D, Braun P, Freund MC, Rabl W, Paal P, Baubin M (2012) Autopsy is more sensitive than computed tomography in detection of LUCAS-CPR related non-dislocated chest fractures. Resuscitation 83:89–90
Jeffery AJ (2010) The role of computed tomography in adult postmortem examinations: an overview. Diagn Histopathol 16:546–551
Yen K, Thali MJ, Aghayev E, Jackowski C, Schweitzer W, Boesch C, Vock P, Dirnhofer R, Sonnenschein M (2005) Strangulation signs: initial correlation of MRI, MSCT, and forensic neck findings. J Magn Reson Imaging 22:501–551
Levy AD, Harcke HT, Mallak CT (2010) Postmortem imaging: MDCT features of postmortem change and decomposition. Am Forensic Med Pathol 31:12–17
Jackowski C, Schweitzer W, Thali M, Yen K, Aghayev E, Sonnenschein M, Vock P, Dirnhofer R (2005) Virtopsy: post-mortem imaging of the human heart in situ using MSCT and MRI. Forensic Sci Int 149:11–23
Grabherr S, Doenz F, Steger B, Dirnhoher R, Dominguez A, Sollberger B, Gygax E, Rizzo E, Chevallier C, Meuli R, Mangin P (2012) Multi-phase post-mortem CT angiography: development of a standardized protocol. Int J Legal Med 25:791–802
Weustink AC, Hunink MGM, van Dijke CF, Renken NS, Krestin GP, Oosterhuis JW (2009) Minimally invasive autopsy: an alternative to conventional autopsy? Radiology 250:897–904
Levy G, Abbott RM, Mallak CT, Getz JM, Harcke HT, Champion HR, Pearse LA (2006) Virtual autopsy: preliminary experience in high-velocity gunshot wound victims. Radiology 240:522–528
Takahashi N, Higuchi T, Shiotani M, Hirose Y, Shibuya H, Yamammouchi H, Hashidate H, Funayama K (2012) The effectiveness of postmortem multidetector computed tomography in the detection of fatal findings related to cause of non-traumatic death in the emergency department. Eur Radiol 22:152–160
Wichmann D, Obbelode F, Vogel H, Hoepker WW, Nierhaus A, Braune S, Suater G, Pueschel K, Kluge S (2012) Virtual autopsy as an alternative to traditional medical autopsy in the intensive care unit: a prospective cohort study. Ann Intern Med 156:123–130
Levy AD, Harcke HT, Getz JM, Mallak CT, Curaso JL, Pearse L, Frasier AA, Galvin JR (2007) Virtual autopsy: two- and three-dimensional multidetector CT findings in drowning with autopsy comparison. Radiology 243:62–68
DiMaio VJ, DiMaio D (2001) Death by drowning. In: Forensic pathology, 2nd edn. CRC, New York, pp 416–422
Thali MJ, Yen K, Plattner T, Schweitzer W, Vock P, Ozdoba C, Dirnhofer R (2002) Charred body: virtual autopsy with multi-slice computed tomography and magnetic resonance imaging. J Forensic Sci 47:1326–1331
Acknowledgments
The authors are most grateful to Richard Medeiros, Rouen University Hospital Medical Editor, for his valuable editing of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Le Blanc-Louvry, I., Thureau, S., Duval, C. et al. Post-mortem computed tomography compared to forensic autopsy findings: a French experience. Eur Radiol 23, 1829–1835 (2013). https://doi.org/10.1007/s00330-013-2779-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-013-2779-0