Abstract
Objectives
The aim of this study is to assess the accuracy of postmortem CT (PMCT) in determining the cause of death in children who underwent a forensic autopsy because of a suspected nonnatural death.
Methods
We selected forensic pediatric autopsies at the Netherlands Forensic Institute, whereby the subject underwent PMCT between 1-1-2008 and 31-12-2012. Cause of death was independently scored by a radiologist and a pathologist. Cause of death was classified (1) in categories being natural, unnatural, and unknown; (2) according to the ICD-10; and (3) according to institutional classification.
Results
In the study period, 189 pediatric forensic autopsies were performed. Fifteen were excluded because of putrefaction. Of the remaining 174 autopsies, 98 (56 %) underwent PMCT. PMCT and autopsy identified the same category in 69/98 cases (70 %, kappa 0.49). They identified the same cause of death in 66/98 cases (67 %, kappa 0.5) using ICD-10; in 71/98 (72 %, kappa 0.62) using a forensic classification. PMCT performed better in unnatural deaths (59–67 % agreement) than in natural deaths (0 % agreement). If no cause of death was detected with autopsy, PMCT failed to identify a cause of death in 98 % (39/40).
Conclusions
Pediatric PMCT does identify the majority of unnatural causes of death, but does not identify new diagnoses (true positives) if no cause of death is found during autopsy. Diagnostic accuracy in natural deaths is low.
Key points
• The case mix is an important predictor for the concordance between PMCT and autopsy.
• In case of an unnatural death, 72–-81 % of PMCT results matches autopsy results.
• In case of a natural death, 0 % of PMCT results matches autopsy results.
• If no cause of death is identified with autopsy, 98 % of PMCT results concurs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Postmortem imaging to determine the cause of death is becoming increasingly popular in both a clinical and forensic setting. A reason for this is that autopsy rates are declining and postmortem imaging seems to be an acceptable alternative. Although the number of publications on the subject is rapidly expanding, the diagnostic accuracy of postmortem imaging compared to conventional autopsy has not yet been validated for all settings. In earlier studies, the majority of cases were fetuses and neonates [1, 2] or adults who died of traumatic causes [3–5]. Recently, two major validation studies in clinical/community samples have been published; one in adults [6] and one in fetuses and children [7]. In the study in adults, both postmortem CT (PMCT) and postmortem MRI were performed; the study showed a concordance rate on cause of death (identifying the organ system involved) between postmortem imaging and autopsy of 70 % (n = 127/182). In the study concerning children, only postmortem MRI was performed. This study demonstrated a concordance rate of 50 % in fetuses (n = 137/272) and 69 % in children (n = 85/123), which was much higher if MRI was combined with minimally invasive autopsy (MIA). MIA enhanced the concordance rate to 97 % in fetuses (n = 263/272) and 76 % in children (n = 94/123). Both studies were performed under ideal circumstances, with every effort being made to obtain optimum scanning and reporting conditions. In the study in adults, both PMCT and postmortem MRI were assessed by four general radiologists, two neuroradiologists, and two cardiac radiologists. Several consensus reports were written, resulting in 11 radiology reports per case. In the study in children, MRI was interpreted by four independent specialist pediatric radiologists. As mentioned by the authors, the results might therefore not reflect clinical practice.
Although PMCT resulted in better concordance than postmortem MRI in adults [6], little has been published on the use of PMCT in pediatric deaths. One PMCT study performed in children who died unexpectedly showed a concordance rate between PMCT and autopsy of 89 % (n = 42/47) [8]. In order to determine the value of postmortem imaging, this technique needs to be validated in different settings. The aim of this study is to assess the accuracy of PMCT in determining the cause of death in children who underwent a forensic autopsy because of a suspected nonnatural death.
Materials and methods
Study population
We selected all consecutive pediatric autopsies that were performed at the Netherlands Forensic Institute (NFI, the Hague) in the period 1-1-2008 to 31-12-2012, whereby the subject underwent PMCT. The NFI is the national center for forensic autopsies, and according to Dutch law, all nonnatural deaths in which a crime is suspected have to have an autopsy performed at the NFI. We excluded cases with severe postmortem changes, scoring more than five points on the decomposition staging scale [9]. The study was not subject to institutional review board approval, as postmortem imaging was performed as part of the forensic work-up according to institutional NFI protocol [10].
Postmortem imaging
Total body PMCT was performed shortly before autopsy, using a clinical state-of-the-art scanner (Toshiba Aquilon, Toshiba Medical Systems Europe B.V, Zoetermeer, the Netherlands; Philips Brilliance 64, Philips Healthcare, Best, the Netherlands; or Siemens Sensation 64, Siemens, Erlangen, Germany). In all cases, maximum of 3.0-mm-thin slices, with sagittal and coronal reconstructions, were obtained. Field of view was adjusted to body size of the child. A PACS system (AGFA Impax 6.4, Mortsel, Belgium) was used to review the studies. The NFI does not have CT facilities; scans were therefore performed in the departments of radiology in the Groene Hart Ziekenhuis (Gouda) and the Academic Medical Center (Amsterdam). All PMCT scans were evaluated by a forensic pediatric radiologist (RR) with 10 years of experience in forensic pediatric radiology.
Autopsy
Median time between time of death and autopsy was 1 day, range 0–7 days; in 90 % of the cases, an autopsy was performed within 2 days. Autopsies were performed according to the local protocol of the NFI [10]. The NFI autopsy includes external and internal examination of the body (both macroscopically and microscopically), including the internal organs of the three body cavities and dissection of the skull, neck, and back. Additional investigations such as toxicology, microbiology, anthropology, DNA, and metabolic investigations are performed when indicated, depending on the case at hand. All findings (both normal and abnormal) are reported; the cause, or possible cause, of death is a central aspect in the conclusion of the report. All autopsies were performed by a forensic pediatric pathologist (VS or AM) with respectively 8 and 15 years experience in the pediatric forensic field.
Data evaluation
Both the radiologist (RR) and pathologist (VS) determined the cause of death based on their findings. They had access to limited patient data, namely age, gender, medical problems before death, and scene findings. The radiologist did not inspect the body, nor did he have access to postmortem photos of the victims. Cause of death was classified in three ways: (1) in three main groups comprising natural, unnatural, and no cause of death; (2) according to the ICD-10 [11]; and (3) according to the forensic classification developed by the NFI [10]. For the concordance between radiologist and pathologist, cause of death was scored based on autopsy or PMCT findings only. In other words, a case could only be classified as unnatural cause of death if something abnormal was found during PMCT or autopsy. To describe the baseline characteristics of the group and to compare the scanned versus not-scanned cases, cause of death was scored based on autopsy findings in combination with scene findings. As an example, a cause of death could be unnatural if two children were found dead while the parent was committing suicide. Based on scene findings, this was classified as an unnatural death, although no specific pathology was detected with PMCT or autopsy. To determine the correlation between radiologist and pathologist, only causes of death they were sure of were scored for this study. Concomitant disease was not classified, as these data were obtained in a forensic evaluation and we aimed to score undoubted causes of death. The reference standard was cause of death identified by the pathologist. Both radiologist and pathologist were blinded for the information by the other rater.
Analysis
Data were analyzed using IBM SPSS Statistics 19. Medians with interquartile ranges (IQR) were calculated for numerical variables, as data were not normally distributed. Normality was assessed using the Kolmogorov-Smirnov test. Differences between subgroups were tested with a Mann-Whitney U test for numerical variables and Chi-square for categorical variables. Agreement was expressed as absolute concordance (number of cases correctly identified by radiologist divided by total numbers of autopsies). Furthermore, the kappa coefficient was calculated to describe the agreement between radiologist and pathologist, taking into account the agreement occurring by chance.
Results
Study group
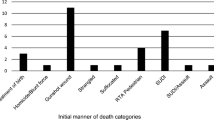
In the 5-year study period, 189 pediatric forensic autopsies were performed at the NFI. Fifteen of these were excluded from this study because of severe putrefaction, these have been described in another paper [12]. Of the 174 autopsies with few postmortem changes, 98 (56 %) underwent PMCT (Fig. 1). The number of PMCTs increased over time, from 34 % in 2008 to 70 % in 2012. In the group with a PMCT scan, median age was 1 year and 1 month, IQR 3 months to 6 years. There were 52 boys (53 %) and 46 girls (47 %).
The case mix of the children who underwent PMCT was typical for the NFI [13]: based on both autopsy and scene findings, 51/98 (52 %) died from unnatural causes; in 35/98 (36 %), no cause of death was determined, i.e., classified as sudden infant death syndrome (SIDS) or sudden unexpected death in infancy (SUDI); and in 12/98 (12 %), a natural cause of death was established. In the children who died of unnatural causes, the cause of death was child abuse in 42/51 (82 %) of the cases; in 9/51 (18 %), the difference between accidental trauma and child abuse could not be determined based on autopsy and scene information. Children who did and did not undergo PMCT differed in age: children who were not scanned were significantly older (median age 2 years and 6 months versus 1 year and 1 month, p = 0.004) (Table 1).
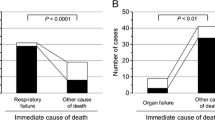
Agreement on cause of death in three main groups
PMCT and autopsy identified the same category in 69/98 cases (70 %) (Table 2). The kappa coefficient was 0.49. Of the 49 children identified from autopsy as an unnatural death, 33 of these (67 %) were identified by PMCT as an unnatural death as well (Online Resource 1, 2); in 16, no cause of death could be identified with PMCT (Fig. 2 and Online Resource 3). Of the 40 children in whom no cause of death was identified with autopsy, one was identified as unnatural and 39 as no cause of death by PMCT (Online Resource 4). Of the nine children identified as natural death by autopsy, all were identified as no cause of death by PMCT (Fig. 3 and Online Resource 5–7). Overall, PMCT was not able to identify the cause of death in 64/98 (65 %) of the cases, 1.6 times more often compared to autopsy. PMCT identified one cause of death where autopsy classified the case as no cause of death. A small subdural hematoma (SDH) over the convexity was seen on PMCT, which was not found during autopsy (Online resource 4).
One-and-a-half-year-old boy, found hanging on a rope positioned around his neck. PMCT showed an intact hyoid–larynx complex (a, b) and except for discrete signs of pulmonary edema (c), no other pathological findings were seen. Intracardiac air in the right atrium and ventricle is noted; this is a normal postmortem finding. Autopsy demonstrated external and internal neck injuries; there was a circular skin abrasion (d) and some hemorrhages in the superficial soft tissues above the sternocleidomastoid muscle (arrow) (e). There were no fractures of the hyoid–larynx complex or the cervical spine. Cause of death was suffocation resulting from trauma on the neck
One-year-and-three-month old boy found dead in an age-appropriate car seat, after a 2-h car trip. PMCT showed a right-sided pleural effusion (asterisk) and a minute amount of air in coronary arteries (arrow) (a). There were no signs of trauma. Autopsy demonstrated a lymphocytic myocarditis, characterized by infiltration of lymphocytes between the cardiomyocytes of the heart, with cardiomyocytolysis (black arrow) (b). Cause of death was cardiac dysfunction based on lymphocytic myocarditis
Agreement on cause of death using ICD-10
Chapters ICD-10
PMCT and autopsy identified the same organ system related to the cause of death in 66/98 cases (67 %) (Table 3). The kappa coefficient was 0.50.
Of the 49 cases identified with autopsy as unnatural death, 31 cases were classified as injury cases; 25/31 (81 %) were classified with PMCT in the same category. Seventeen cases were identified with autopsy as external causes of death; 4/17 (24 %) were identified with PMCT in the same category. There was one case of malnutrition due to neglect, which was classified as endocrine, but was considered an unnatural death by the pathologist. PMCT identified this case as no cause of death.
Based on autopsy findings only, autopsy identified 40 children as unknown cause of death; 2 perinatal deaths and 38 not otherwise specified (NOS). Of these 38 NOS cases, 37 (97 %) were also identified by PMCT as unknown, and one was identified as injury. Both perinatal deaths were identified by PMCT.
The nine children identified as a natural cause of death were classified with autopsy as infectious (n = 1), respiratory (n = 4), and circulatory (n = 4). All of these were identified with PMCT as no cause of death.
Subgroups ICD-10
The pathologist used 22 different ICD-10 subgroups to classify the causes of death. Overall, in 64/98 cases (65 %), PMCT classified in the same ICD-10 subgroup (Table 4). The kappa coefficient for the subgroups was 0.59.
In 26/49 (53 %) of the unnatural causes of death, PMCT identified the same subgroup. In 38/40 (95 %) of the unknown causes of death, PMCT identified the same subgroup. In 0/9 (0 %) of the natural causes of death, PMCT identified the same subgroup.
Agreement on cause of death using NFI classification
The pathologist used 11 different codes from the forensic classification. In 71/98 (72 %), PMCT identified the same forensic classification (Table 5). The kappa coefficient was 0.62.
In 32/49 (65 %) of the unnatural causes of death, PMCT identified the same diagnosis. In 39/40 (98 %) of the unknown causes of death, PMCT identified the same diagnosis. In 0/9 (0 %) of the natural causes of death, PMCT identified the same diagnosis.
Discussion
We determined the concordance between PMCT and autopsy in cause of death in children. To our knowledge, this is the first PMCT study performed in children in a forensic setting.
The case mix of the patients seems to be an important predictor for the concordance between PMCT and autopsy. In unnatural deaths, concordance between PMCT and autopsy was 67 %. A systematic review of this topic in adults showed a concordance in unnatural deaths between 46 and 100 % [14]. In natural deaths, PMCT did not identify any cause of death in our study. Another study found a concordance rate of 88 % for PMCT vs. autopsy (38/43) for natural pediatric deaths [8]. A pediatric MRI study, describing 88 % natural and 12 % unnatural deaths, found a concordance rate of 69 % for MRI vs. autopsy (85/123) [7]. We have no explanation for our poor results on natural deaths. Concordance rate on cases where autopsy did not identify a cause of death was 98 %, which is comparable with other publications [6–8].
False negatives
In the cases identified with autopsy as unnatural death (n = 49), the number of false negatives was 39 % (16/49). Unnatural deaths most commonly missed with PMCT were injuries caused by hanging, strangulation or suffocation (n = 7) (Fig. 2), injuries caused by smoke and fire (n = 5) (Fig. 3), and head (n = 3) and abdominal injuries (n = 3).
In the cases identified with autopsy as natural death (n = 9), all PMCT reports were false negatives. These were all infectious diseases: myocarditis (n = 4) (Fig. 3 and Online Resource 5) pneumonia (n = 3) (Online Resource 6 and 7), bronchiolitis (n = 1) and miliairy TB (n = 1). However, other pediatric studies identified infectious diseases correctly: in the study by Proisy et al., PMCT identified 79 % (11/14) natural causes of death, including pneumonia (n = 7), pneumonia and gastroenteritis (n = 1), pancarditis (n = 1), metabolic disease (n = 1), and bowel volvulus (n = 1) [8]. The only false-negative causes of death were three cases of pneumonia. This low number of false negatives is surprising given that postmortem diagnosis of pulmonary disease is complex, since postmortem consolidation and livor mortis interfere with assessment of the lungs. Furthermore, radiological characteristics of pancarditis and metabolic disease are not described in the article, but in general, these are not demonstrated with CT. An explanation for the different results between their study and this one is the fact that we only scored causes of death if the radiologist was absolutely sure that these abnormalities had caused the death. Major or minor abnormalities were sometimes detected but not scored if it was not sure that these findings would have caused the death. We chose these strict criteria because all PMCTs were performed in a forensic setting; in court, a doubtful diagnosis is not acceptable. In the MRI study, 32/132 (26 %) of the MRI reports were false negatives [7]. Diagnoses most commonly missed were sepsis (n = 24) and placental abnormalities (n = 3).
False positives
Of all cases where autopsy did not identify a cause of death (n = 40), PMCT identified a small SDH in one case (1 %). As it is unlikely that an SDH would be missed during a forensic autopsy, this was regarded as a false positive finding. Based on this one extra case, it seems unlikely that PMCT in children will identify many diagnoses that will be missed during autopsy. PMCT identified two cases of pneumonia (2/47 or 4 %) regarded to be false positives in another study [8]. In the MRI study, two false-positive diagnoses (2 %) were identified: ischemic brain injury and drowning [7].
Limitations
A limitation of our study is that not all autopsy cases underwent PMCT scanning, resulting in the inclusion of 59 % of the autopsies. The reason for this is that the NFI does not own its own CT scanner and practicalities can impede routine transportation of the body. In children under the age of 4 years, a skeletal survey is always performed to identify occult fractures. These cases are transported to a hospital where they also undergo PMCT. Another reason is that the use of PMCT is a relatively new development and it takes time to implement new protocols. We do not expect that the selection of patients influenced our results, as distribution of causes of death was identical in the PMCT and the non-PMCT group.
Future perspective
Several adaptations to postmortem imaging are currently being developed. In adults, the results of postmortem angiography are promising [15–17]. As ischemic heart disease is uncommon in children, this will probably be of limited value in a pediatric setting. Postmortem ventilation, however, might improve the diagnostic value of postmortem imaging in children. Applying pressure to the lungs reduces livores, and small lung pathologies become more visible [18]. Minimally invasive autopsy increases the concordance rate between postmortem MRI and autopsy from 69 to 76 % in children and shows even better results in fetuses [7, 19]. The combination of PMCT and minimally invasive autopsy, or both PMCT and MRI with minimally invasive autopsy, is promising in adults [20, 21], but has not yet been validated in children. In 2011, the first case was published in which a cause of death established by PMCT, in combination with postmortem MRI and tissue biopsy, was accepted by the Swiss Department of Public Prosecution, without confirmation by a forensic autopsy [22]. In this case, a pedestrian crossing the street had been hit by a car. On postmortem imaging, extensive blunt trauma was demonstrated; among others, a vertebral fracture piercing the aorta and causing extensive internal hemorrhage. In many countries, e.g., the Netherlands, replacement of autopsy by postmortem imaging is currently not accepted in Court yet, as only validated and widely accepted methods can be submitted as evidence.
In conclusion, PMCT in children does identify the majority of unnatural causes of death correctly (67 %); it does not give new insight into the cause of death if this is unexplained according to the pathologist. Diagnostic accuracy in natural deaths in this study is low compared to other publications. At present, PMCT cannot replace conventional autopsy in children, but in combination with minimally invasive autopsy, it might be suitable for determining those cases that require conventional autopsy.
Abbreviations
- ICD-10:
-
International Classification of Diseases, version 2010
- NFI:
-
Netherlands Forensic Institute
- PMCT:
-
Postmortem CT
- SDH:
-
Subdural hematoma
References
Alderliesten ME, Peringa J, van der Hulst V, Blaauwgeers HL, van Lith JM (2003) Perinatal mortality: clinical value of postmortem magnetic resonance imaging compared with autopsy in routine obstetric practice. BJOG 110:378–382
Cohen MC, Paley MN, Griffiths PD, Whitby EH (2008) Less invasive autopsy: benefits and limitations of the use of magnetic resonance imaging in the perinatal postmortem. Pediatr Dev Pathol 11:1–9
Aghayev E, Christe A, Sonnenschein M et al (2008) Postmortem imaging of blunt chest trauma using CT and MRI: comparison with autopsy. J Thorac Imaging 23:20–27
Anon J, Remonda L, Spreng A et al (2008) Traumatic extra-axial hemorrhage: correlation of postmortem MSCT, MRI, and forensic-pathological findings. J Magn Reson Imaging 28:823–836
Christe A, Ross S, Oesterhelweg L et al (2009) Abdominal trauma—sensitivity and specificity of postmortem noncontrast imaging findings compared with autopsy findings. J Trauma 66:1302–1307
Roberts IS, Benamore RE, Benbow EW et al (2012) Post-mortem imaging as an alternative to autopsy in the diagnosis of adult deaths: a validation study. Lancet 379:136–142
Thayyil S, Sebire NJ, Chitty LS et al (2013) Post-mortem MRI versus conventional autopsy in fetuses and children: a prospective validation study. Lancet 382:223–233
Proisy M, Marchand AJ, Loget P et al (2013) Whole-body post-mortem computed tomography compared with autopsy in the investigation of unexpected death in infants and children. Eur Radiol 23:1711–1719
Clark MA, Worell MB, Pless JE (1997) Postmortem changes in soft tissues. In: Haglund WD, Sorg MH (eds) Forensic Taphonomy. The postmortem fate of human remains. CRC Press LLC, Boca, pp 161–162
Soerdjbalie-Maikoe V, Maes A (2010) Forensisch post mortem onderzoek bij minderjarigen. Theoretische en praktische aanbevelingen voor artsen en arts-pathologen. Nederlands Forensic Institute, The Hague
ICD-10 (2010) International statistical classification of diseases and related health problems, 2013th edn. World Health Organization, Geneva
Sieswerda-Hoogendoorn T, Soerdjbalie-Maikoe V, Maes A, van Rijn RR (2013) The value of post-mortem CT in neonaticide in case of severe decomposition: Description of 12 cases. Forensic Sci Int 233:298–303
Soerdjbalie-Maikoe V, Bilo RA, van den Akker E, Maes A (2010) Unnatural death due to child abuse—forensic autopsies 1996–2009. Ned Tijdschr Geneeskd 154:A2285
Scholing M, Saltzherr TP, Fung Kon Jin PH et al (2009) The value of postmortem computed tomography as an alternative for autopsy in trauma victims: a systematic review. Eur Radiol 19:2333–2341
Michaud K, Grabherr S, Doenz F, Mangin P (2012) Evaluation of postmortem MDCT and MDCT-angiography for the investigation of sudden cardiac death related to atherosclerotic coronary artery disease. Int J Cardiovasc Imaging 28:1807–1822
Christine C, Francesco D, Paul V et al (2013) Postmortem computed tomography angiography vs. conventional autopsy: advantages and inconveniences of each method. Int J Legal Med 127:981–989
Ross SG, Thali MJ, Bolliger S, Germerott T, Ruder TD, Flach PM (2012) Sudden death after chest pain: feasibility of virtual autopsy with postmortem CT angiography and biopsy. Radiology 264:250–259
Germerott T, Flach PM, Preiss US, Ross SG, Thali MJ (2012) Postmortem ventilation: a new method for improved detection of pulmonary pathologies in forensic imaging. Leg Med (Tokyo) 14:223–228
Sebire NJ, Weber MA, Thayyil S, Mushtaq I, Taylor A, Chitty LS (2012) Minimally invasive perinatal autopsies using magnetic resonance imaging and endoscopic postmortem examination ("keyhole autopsy"): feasibility and initial experience. J Matern Fetal Neonatal Med 25:513–518
Weustink AC, Hunink MG, van Dijke CF, Renken NS, Krestin GP, Oosterhuis JW (2009) Minimally invasive autopsy: an alternative to conventional autopsy? Radiology 250:897–904
Bolliger SA, Filograna L, Spendlove D, Thali MJ, Dirnhofer S, Ross S (2010) Postmortem imaging-guided biopsy as an adjuvant to minimally invasive autopsy with CT and postmortem angiography: a feasibility study. AJR Am J Roentgenol 195:1051–1056
Ruder TD, Hatch GM, Thali MJ, Fischer N (2011) One small scan for radiology, one giant leap for forensic medicine—post-mortem imaging replaces forensic autopsy in a case of traumatic aortic laceration. Leg Med (Tokyo) 13:41–43
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Online Resource 1
Nine-year old girl found in bed, with a lot of blood nearby the body. The left side of the neck of the child was deeply cut, which was seen with both PMCT (A) and autopsy (B). The trachea was intact and the cause of death was exsanguination.(JPEG 172 kb)
B
(JPEG 114 kb)
Online Resource 2
Three-month-old girl, previously healthy, who according to caregivers suddenly collapsed and needed cardiopulmonary resuscitation. She was admitted to a pediatric intensive care unit, where she died on the day of the admission. PMCT scan shows a subdural hematoma along the falx cerebri (arrows) (A). The lack of gray-white matter differentiation is a normal postmortem finding. Chest CT of the same patient shows multiple healing rib fractures, 2nd to 6th, along the left lateral side of the chest (arrow) (B). At autopsy, a subdural hematoma, subarachnoidal hematoma and contusion at the left frontal side of the cerebrum (no picture taken). There were healing rib fractures along the left lateral side, of the second to the sixth ribs (C). Underlying bone diseases were excluded microscopically. Based on the acute neurological deterioration and the older rib fractures, it was concluded that there were at least two (abusive) incidents separated in time. (JPEG 46 kb)
B
(JPEG 35 kb)
C
(JPEG 111 kb)
Online Resource 3
Eleven-year-old girl found in a house, after a domestic fire. PMCT showed no signs of intracranial trauma (A), normal pulmonary postmortem findings, without signs of edema (B), and normal intra-abdominal organs (C). At autopsy the brain was slightly edematous; the weight was 1,280 g (compared to a reference standard of 1,150 g) and flattening of the gyri and sulci was seen (D). At microscopy edema was confirmed (E). In the lungs edema (black arrow), congestion (red arrow) and postmortem gas formation (white arrow) were seen (F). There were no signs of external trauma. Cause of death was carbon monoxide intoxication, based on the combination of thermal damage to the airways and a carboxyhemoglobin level of 32 % as measured in heart blood. (JPEG 32 kb)
B
(JPEG 33 kb)
C
(JPEG 33 kb)
D
(JPEG 78 kb)
E
(JPEG 99 kb)
F
(JPEG 97 kb)
Online Resource 4
Six-month-old girl, found between the couch and the radiator. Her head was positioned downwards. According to clinical history the caregiver had been fallen asleep with the baby on the couch. On PMCT a thin layered subdural hematoma (arrow) was diagnosed (A). At autopsy, several bruises on the head were found. Furthermore, there was swelling of the brain; the dura was stretched and tense, the brain was bulging through the first incision in the dura; the gyri were pale and flattened (B,C). No definite cause of death was established. Autopsy did not confirm the radiological diagnosis of subdural hematoma. The radiological finding can be explained as a beam hardening artifact and constitutes a false positive finding. (JPEG 114 kb)
B
(JPEG 130 kb)
C
(JPEG 130 kb)
Online Resource 5
Two-month-old boy found dead in prone position in his crib. PMCT showed no abnormalities, other than normal postmortem changes, such as a minor amount of postmortem gas formation in the right atrium and ventricle and left ventricle (A). At autopsy a bilateral pneumonia, with bronchial and alveolar leukocyte infiltrates, as well as a lymphocytic myocarditis, with lymphocyte-rich inflammatory infiltrate (black arrow) in combination with focal areas of cardiomyocytolysis with hypereosinofilia of the cardiomyocyte (white arrow) (B), were found. Microbiological throat swabs tested positive for Rhinovirus. Cause of death was tissue damage due to pulmonary and cardiac inflammations. (JPEG 79 kb)
B
(JPEG 104 kb)
Online Resource 6
Three-month-old boy found in a critical state in a baby chair at home. He was admitted to a pediatric intensive care unit, where on neuroimaging severe brain hypoxia was diagnosed. The patient died one week after admission, after medical support was withdrawn because of a poor neurological prognosis. PMCT showed infiltrative pulmonary lesions, differential diagnostically interpreted as edema or inflammation (A). Autopsy demonstrated severe pulmonary edema (black arrow) and bilateral bronchopneumonia with infiltration of neutrophilic granulocytes in alveoli and in bronchus lumen (white arrows) (B). In the brain hypoxic encephalopathy was detected. Microbial specimens were negative for viruses and bacteria. Cause of death was multiorgan failure. (JPEG 80 kb)
B
(JPEG 114 kb)
Online Resource 7
Three-year-old girl found dead in her bed. PMCT showed diffuse patchy areas of ground glass (A). At autopsy bilateral pulmonary edema (black arrow) and pneumonia was observed, with neutrophile granulocytes in the alveoli (white arrow) (B). Microbiological specimen of the lung tissue was positive for B-hemolytic streptococci and in the throat specimen RS-virus was collected. Cause of death was organ dysfunction, especially of the lungs, on the basis of severe pneumonia. (JPEG 90 kb)
B
(JPEG 214 kb)
Rights and permissions
About this article
Cite this article
Sieswerda-Hoogendoorn, T., Soerdjbalie-Maikoe, V., de Bakker, H. et al. Postmortem CT compared to autopsy in children; concordance in a forensic setting. Int J Legal Med 128, 957–965 (2014). https://doi.org/10.1007/s00414-014-0964-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-014-0964-6