Abstract
Purpose
Postmortem computed tomography angiography (PMCTA) was introduced into forensic investigations a few years ago. It provides reliable images that can be consulted at any time. Conventional autopsy remains the reference standard for defining the cause of death, but provides only limited possibility of a second examination. This study compares these two procedures and discusses findings that can be detected exclusively using each method.
Materials and methods
This retrospective study compared radiological reports from PMCTA to reports from conventional autopsy for 50 forensic autopsy cases. Reported findings from autopsy and PMCTA were extracted and compared to each other. PMCTA was performed using a modified heart–lung machine and the oily contrast agent Angiofil® (Fumedica AG, Muri, Switzerland).
Results
PMCTA and conventional autopsy would have drawn similar conclusions regarding causes of death. Nearly 60 % of all findings were visualized with both techniques. PMCTA demonstrates a higher sensitivity for identifying skeletal and vascular lesions. However, vascular occlusions due to postmortem blood clots could be falsely assumed to be vascular lesions. In contrast, conventional autopsy does not detect all bone fractures or the exact source of bleeding. Conventional autopsy provides important information about organ morphology and remains the only way to diagnose a vital vascular occlusion with certitude.
Conclusion
Overall, PMCTA and conventional autopsy provide comparable findings. However, each technique presents advantages and disadvantages for detecting specific findings. To correctly interpret findings and clearly define the indications for PMCTA, these differences must be understood.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The use of multi-detector computed tomography (MDCT) in postmortem investigations has become routine in many centers of legal medicine [1–6]. MDCT is a rapid and easy way to look inside the body and document findings. It offers the opportunity to consult data at any time, even after cremation or burial of the body. Furthermore, the handling of an MDCT unit is relatively easy, and its maintenance costs are affordable for certain institutes of legal medicine. The diagnostic value of MDCT compared to conventional autopsy has been addressed in multiple publications [7, 8].
Although native or unenhanced MDCT (without the injection of contrast agent) can show major vascular lesions such as aortic rupture [9], its most important limitation is its low ability to visualize the vascular system and soft tissue. By injecting contrast agent into the vessels, different parts of the vascular system are rendered visible [10–13]. Recent advances have made it possible to visualize the entire vascular system in a minimally invasive way [14, 15]. The performance of postmortem computed tomography angiography (PMCTA) appears to have important advantages, especially in detecting sources of hemorrhage [16, 17]. In the early twenty-first century, postmortem angiography was performed with little success due to the imaging and perfusion techniques [18, 19]. In 2008, Grabherr at al. introduced the use of a modified heart–lung machine to establish postmortem circulation, in turn allowing the injection of a contrast agent and constant perfusion of a body [20]. This technique has been further developed and standardized. Nowadays, it consists of the execution of at least one native computed tomography scan and three angiographic phases (arterial, venous, and dynamic). This multi-phase PMCTA (MPMCTA) [21] has been introduced as a routine investigation method at the University Centre of Legal Medicine in Lausanne. The combination of MPMCTA with conventional autopsy appears to increase the results of postmortem investigations, as has been stated regarding the examination of the coronary arteries [22].
However, MPMCTA is still a new technique. In contrast, conventional autopsy consists of a systematic approach that has been known and used for centuries—one reason why it is recognized as the optimal method with which to detect findings that indicate an individual’s cause of death. To define the limits, advantages, and overall diagnostic value of MPMCTA, it is necessary to compare the performance of this new method to the well-known technique of conventional autopsy. To our knowledge, this is the first such study.
This study will evaluate the diagnostic value of MPMCTA compared with native MDCT and conventional autopsy, and describe findings that can be detected exclusively by each method to define method-specific limitations and advantages.
Materials and methods
Subjects
A total of 50 human corpses with postmortem intervals ranging from a few hours to several days were included retrospectively in the study. The first nine bodies were donated by anatomical institutes, and a summary of the medical history of the diseased was made available. The other 41 cadavers underwent a forensic autopsy in our institute between September 2008 and February 2010. A consecutive sample method with no specific exclusion criteria was used to include autopsy cases. No choice was made concerning the indication for the medico-legal autopsy. Therefore, causes of death included trauma (e.g., stab wounds or traffic accidents), intoxication (e.g., drug or carbon monoxide intoxication), and natural death (e.g., heart attack or cancer-related complications). In each case, a radiological investigation including native CT scan and postmortem CT angiography was performed before the conventional autopsy. This study was approved by the local justice department and the ethics committee.
Radiological examination
Before starting any invasive incisions, an external examination of the body was performed by the forensic pathologist in charge of the case, and a native CT scan was done by the forensic radiographer of the institute. MDCT scans were performed using an eight-row CT unit (CT LightSpeed 8; GE Healthcare, Milwaukee, WI, USA) with the following scan parameters: field of view (FOV), 50 cm; slice thickness, 2.5 mm; interval of reconstruction, 2 mm; 120 kV; 280 mA (modulated); and noise index, 15. The scan was performed following the standard protocol of the institute, from the cerebral vertex to the pubic symphysis. Standard lung and bone filter reconstructions were acquired, and bone-reformatted images of the spine were extracted.
After the collection of postmortem liquid samples under CT guidance for toxicological analysis and the analysis of clinical biomarkers [21, 23], cannulation of the femoral vessels of one side was performed using 16F diameter cannulas for arteries and 18F cannulas for veins (MAQUET GmbH & Co. KG, Rastatt, Germany). MPMCTA was performed according to the standardized protocol proposed by Grabherr et al. [21], using a contrast agent mixture composed of 6 % of the oily liquid Angiofil® (Fumedica AG, Muri, Switzerland) and paraffin oil (paraffinum liquidum) with a Virtangio® perfusion device (Fumedica). For the arterial phase of MPMCTA, 1,200 ml of contrast-agent mixture has been injected into the femoral artery using a flow rate of 800 ml/min. Once this volume was injected, data acquisition of the arterial phase was completed using the following scan parameters: field of view, 50 cm; slice thickness, 1.25 mm; interval of reconstruction, 0.6 mm; 120 kV; 280 mA (modulated); and noise index, 15.
For the venous phase, 1,800 ml of contrast-agent mixture has been injected at a flow rate of 800 ml/min. Data acquisition was then obtained using the following scan parameters: field of view, 50 cm; slice thickness, 2.5 mm; interval of reconstruction, 1.2 mm; 120 kV; 280 mA (modulated); and noise index, 15. In order to perform the dynamic phase of MPMCTA, further 500 ml of contrast-agent mixture were injected at a flow rate of 200 ml/min. The data acquisition of this phase was performed during the ongoing injection in order to mimic in vivo conditions. For this acquisition, the same scan parameters were used as in the venous phase of angiography.
Radiological interpretation
A complete radiological report, including native CT scan and CT angiography, was written jointly by two board certified radiologists (one specialized in vascular radiology and one specialized in neuroradiology) and one board certified forensic pathologist specialized in forensic radiology. These specialists did get major information about the case such as age of the deceased, circumstances of death or discovery of the body, short medical history if available, information obtained by witnesses, and most important findings of the external examination (same information as the forensic pathologist had prior to autopsy).
Findings that were identified and reported in the autopsy report but not in the radiological report were then cross-checked by one radiologist to define whether the finding was imperceptible or simply not reported during the first lecture.
Conventional autopsy
Autopsies were performed by the forensic pathologists in charge of the case (one board-certified forensic pathologist and one forensic pathologist-in-training). These experts were informed about the most important radiological findings prior to the autopsy, enabling them to adequately adapt their autopsy technique. The autopsy complied with local standards (examination of the cranial, thoracic, and abdominal cavities) and was in accordance with European standards [24]. A complete autopsy report was edited by the two forensic pathologists.
Data extraction
To compare the two procedures (radiological examination and autopsy), only macroscopic autopsy findings (excluding those from external examination, histology, and toxicology) were taken into account and extracted from the autopsy reports.
For each case, all reported signs were extracted from both radiological and autopsy reports by an independent observer. This process made it possible to recognize findings that were identified and reported by both methods, as well as those that were only mentioned by a single method.
All findings were also categorized by the type of tissue in which they were observed. Therefore, we distinguished between vascular (e.g. leak, rupture, and occlusion), bone (e.g., fracture, arthrosis, and defect), soft tissue (e.g., hematoma…), and parenchymal (e.g., lung or liver nodules, and lacerations) findings.
To define the importance of each finding to the solution of the respective case, two board-certified forensic pathologists independently classified each finding, without knowing if it was extracted from autopsy or radiological report, on a three-step Likert scale: “essential”, “useful”, and “not important”. Experts were asked to "subjectively evaluate the importance of each finding in defining the cause of death". For example, in one case "Fracture of the 4th, 5th and 6th rib, and fracture of the sternum" was judged as "useful findings" only as these fractures were due to unsuccessful cardiopulmonary resuscitation that took place after death had occurred whereas in a cases of thoracic trauma, such fractures would be judged as “essential findings”. To give another example, the presence of coronary sclerosis would be esteemed as essential finding in a case of sudden cardiac disease whereas it would only be classified as “useful finding” in a case of trauma. Typical “not important findings” were the description of degenerative changes of the spine or the presence of small gallstones. When experts disagreed, an intermediate category was generated. Therefore, in total, there were five ordinal values corresponding to “Essential finding” (important to solve the case), “Very useful finding” (helped to solve the case), “Useful finding” (good to know), “Less important finding” (may be mentioned), and “Not important finding” (not useful to mention).
Causes of death were defined from the overall conclusion, which includes all examinations. Cause of death was then categorized as due to polytrauma, other violent death, sudden cardiac death, or other natural death.
Statistical analysis
Kappa statistics were used to assess the reliability of pathologists’ judgments when defining the relevance of each sign used to determine the cause of death. Next, we used the chi-squared test to test the significance level of observed differences between groups that had been classified by relevance of signs, nature of tissue, and cause of death. The significance level was set at 0.05, and P values did not take into consideration the lack of independence between signs from the same case. Results were confirmed using a generalized estimate equation that controlled for clustering effects. All statistics were performed by a certified statistician, using STATA 12.0 (StataCorp LP, College Station, TX, USA).
Results
Details of the 50 cases assessed are summarized in Table 1. From these 50 cases, a total of 582 findings were reported.
On a three-step Likert scale, overall agreement between the two assessors regarding the relevance of findings to the conclusion of the cause of death was 61.5 %. Two hundred eighteen of the discrepancies (97.3 %) concerned neighboring categories, while the six remaining findings were classified with a discrepancy of two categories. Therefore, even when Cohen’s kappa was low (k = 0.34; 95 % CI = 0.28, 0.41), the assessment was shown to be reliable when the ordinal value of the scale was taken into consideration (ICC2,3 = 0.573; 95 % CI = 0.481, 0.647).
Of the 463 findings reported at autopsy, 340 were initially reported by the radiologists (73.4 %; 95 % CI = 69.2, 77.4). Five radiological findings out of 459 (1.1 %; 95 % CI = 0.4, 2.5) were “missed” during the first lecture and identified during the second reading. Apparently, the ability to detect findings from the autopsy was not related to the cause of death (χ 2 = 1.73; df = 3; P = 0.630), but was mostly related to the nature of the lesion itself (χ 2 = 35.4; df = 4; P < 0.001). The proportion of findings detected by CT angiography was highest (91.3 %) for findings estimated as essential to defining the cause of death. This trend was independent of the type of tissue studied and the cause of death (Table 2).
Compared to autopsy or CT, MPMCTA was most efficient in detecting essential findings (Table 3). MPMCTA was highly efficient in detecting vascular signs (97.1 %) and bone findings (98.6 %, with bone filter reconstructions). However, it demonstrated some limitations regarding the detection of parenchymal findings (79.1 %), while autopsy demonstrated major limitations in detecting bone findings (58.9 %). These two methods were complementary, as 97.7 % of findings in parenchyma were detected by autopsy.
Useless findings for defining the cause of death were reported in both radiological and autopsy reports (Table 4), and varied from 14.7 % of reported findings for MPMCTA to 17.9 % for native CT scan.
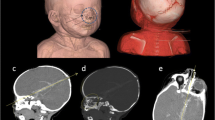
Figure 1 illustrates the comparative abilities of imaging and autopsy to detect findings. Thirty of the 73 essential bone signs were detected by imaging alone, while nine of the 43 essential parenchymal findings were detected by autopsy alone. Thirty of the 38 findings that were judged of no importance were of parenchymal origin.
As the radiological investigation showed clear advantages especially concerning bone findings, we investigated these findings in more details (Table 5). One hundred twenty-three fractures were observed on 22 cases. The number of fractures per case ranged from one to 33 fractures (median = 2). Thirty-nine fractures (31.7 %) were not reported during the autopsy. Missed fractures most often concerned the scapula (3/3; 100 %), the pelvis (5/7; 71.4 %), the skull (17/36; 47.2 %), and the spine (13/30; 43.3 %), and least of all the ribs, sternum and collar bone (1/40; 2.5 %), the lower limb (0/3; 0 %), and the hyoid bone (0/3; 0 %).
Discussion
The present study evaluated the diagnostic value of MPMCTA, particularly its additional value compared with native CT and advantages and limitations compared with conventional autopsy. We compared findings extracted from radiological reports with those extracted from conventional autopsy reports without taking into consideration the results of histology, toxicology, or additional examinations because the study’s aim was to compare the results of autopsy and imaging, and not those of the entire medico-legal investigation to imaging alone.
To determine the overall value of MPMCTA, medico-legal cases were selected according to the availability of technical personnel during the initial implementation of this new technique, rather than in response to specific indications. Therefore, MPMCTA was applied to some cases for which this type of investigation would not have been indicated in routine practice. This consequence can be assimilated as a limitation of the study. However, different types of medico-legal cases are examined. We therefore limited bias concerning the application of this technique to only one kind of case. In addition, this procedure permitted to determine in which cases the performance of MPMCTA is of use, and therefore to define indications for its application.
To examine the impact of MPMCTA, we categorized different findings according to their importance for solving respective medico-legal cases. Although the two board-certified forensic pathologists who performed this grading have graduated from different European medico-legal schools, their estimations were similar regarding the importance of each finding.
As suspected at the beginning of our study, these results demonstrate that MPMCTA is highly efficient in the detection of vascular findings, particularly regarding hemorrhage sources (Table 3). However, some vascular findings were only detected by conventional autopsy. Such findings were bleedings into the vascular wall or ruptured atherosclerotic plaques that were too small to be detected by CT because they were essentially located in the coronary vessels. A similar observation has already been described by Michaud et al., who investigated the use of MPMCTA to examine coronary arteries [22].
The most important weakness of MPMCTA was its inability to visualize parenchymal findings. Although the performance of an MPMCTA can significantly improve the detection of parenchymal findings compared with native MDCT (from 65 % to 80.9 %), it still remains less sensitive than conventional autopsy. This difference can be easily explained by the fact that, even with the injection of contrast agent, contrast of the parenchyma is not high enough to diagnose lesions of inner organs. The implementation of MRI has already been proposed to overcome this disadvantage of forensic imaging, and initial studies have had promising results [25–27]. However, gaining access to an MRI unit may be even more difficult for forensic institutions than the performance of an MPMCTA.
Concerning the detection of bone findings, the radiological examination appears to clearly overcome conventional autopsy (Table 2). As shown by our results and in Table 5, standard autopsy can miss fractures in different regions of the body, especially in those which are difficult to access (scapula, spine, pelvis, and skull). Concerning the skull, missed fractures were mostly located in the facial bones which are not investigated routinely by a standard conventional autopsy. By using an appropriated filter of reconstruction, bone findings can be obtained by performing either native CT scan or MPMCTA.
One surprising result of this study was that MPMCTA appears to have greater sensitivity regarding soft tissue findings, such as small hemorrhages in subcutaneous fatty tissue or muscular tissue. This fact may be explained by the high sensitivity of contrast agents to detect the smallest extravasations (e.g., hematomas) but also by the fact that we have compared radiological data to findings from standard conventional autopsy, including opening three body cavities and examining soft tissue in the thorax and abdomen, but not including the dissection of soft tissue of the back. While the complete and detailed dissection of subcutaneous and muscular tissue of the back requires a special indication in conventional autopsy, the soft tissue of the back is always visualized during a standard CT acquisition, which includes the head, thorax, and abdomen. Therefore, MPMCTA may detect small hemorrhages in the muscle and subcutaneous tissue that would not necessarily be searched for during a conventional autopsy. This possibility may indicate that MPMCTA could also be used as a screen to decide whether dissection of the back is necessary.
Native CT scan and MPMCTA provided nearly the same percentage of non-useful findings (Table 4). The mean number of findings reported as non-useful for conclusions of sudden cardiac death and other violent death is slightly higher for imaging than for autopsy, possibly because radiologists are used to a very detailed description of pathological changes that may play a role in clinical investigations, but not in forensic ones. A typical example is the description of degenerative lesions of the vertebral spine, which are mostly present in elderly subjects. As a matter of fact, elderly subjects are mostly victims of sudden cardiac death, and therefore the description of such “useless findings” may be observed more often in this group. Cases of other violent death were typically cases of intoxication. These also, showed more preexisting pathological changes that were described by radiologists without influencing the cause of death.
According to the results of our study, the indication to perform MPMCTA depends on the findings that are expected. MPMCTA is indicated if lesions are suspected in the vascular system according to the circumstances of death and the medical anamnesis (e.g., cases of polytrauma or sudden cardiac death). Cases in which a hemorrhage is suspected, or in which the vascular system has been modified by a surgical intervention (e.g., after coronary bypass), comprise a very special group of cases in which a detailed examination of the vascular anatomy is of importance. The performance of MPMCTA does not make sense in cases in which no vascular lesions are expected (e.g., cases of intoxication, drowning, or hanging). A vascular lesion should be suspected as a result of the reported data concerning the case, as well as after viewing the data from a native CT scan.
In our institute, the decision to perform MPMCTA is made by the forensic pathologist in charge of the case, who has all information necessary to know the circumstances of death and who will view radiological images of the native MDCT before starting the autopsy. This new technique can be implemented easily, particularly in institutes with access to a CT unit. Performance of a complete MPMCTA takes 1 to 1.5 h (depending on the MDCT unit used), including sample collections performed prior to the injection of the contrast agent. Thus, the entire postmortem investigation would be prolonged by up to 1.5 h, a change that appears to be possible, especially considering the advantages that can be obtained by using this technique. In our institute, the entire radiological examination is performed by forensic radiographers [26], which have been added to the forensic team. The multi-phase exploration can increase on one hand the quality of the obtained images as it allows a nearly complete filling of the vessels of the head, the thorax, and the abdomen and, on the other hand, it ameliorates also the radiological interpretation as it allows to verify findings by comparing different angiographic phases as described by Grabherr et al. [21]. However, the performance of the technique and the radiological interpretation of the images require specialized personnel.
If we consider all findings regardless of tissue type and importance, MPMCTA and conventional autopsy demonstrate nearly the same sensitivity concerning the detection of important findings. MPMCTA can increase the sensitivity of native CT scan from 65 % to 80.9 %, while conventional autopsy detects 83.1 % of all findings (Table 3). The result concerning essential findings is more surprising: autopsy reported 77.2 % and MPMCTA reported 93.3 % of all findings. For this reason, we esteem MPMCTA as a very powerful and useful tool that should be implemented as part of the routine medico-legal examination, if possible.
References
Dirnhofer R, Jackowski C, Vock P et al (2006) VIRTOPSY: minimally invasive, imaging-guided virtual autopsy. Radiographics 26(5):1305–1333, Review
Thali M, Dirnhofer R, Vock P (eds) (2009) The virtopsy approach: 3D optical and radiological scanning and reconstruction in forensic medicine. CRC, New York
Weustink AC, Hunink MGM, van Dijke CF et al (2009) Minimally invasive autopsy: an alternative to conventional autopsy? Radiology 250(3):897–904
Jeffery AJ (2010) The role of computed tomography in adult postmortem examinations: an overview. Diagn Histopathol 16(12):546–551
O’Donnell C (2010) An image of sudden death: utility of routine postmortem computed tomography scanning in medico-legal autopsy practice. Diagn Histopathol 16(12):552–555
Poulsen K, Simonsen J (2007) Computed tomography as a routine in connection with medico-legal autopsies. Forensic Sci Int 171(2–3):190–7
Jacobsen C, Lynnerup N (2010) Craniocerebral trauma-congruence between postmortem computed tomography diagnoses and autopsy results: a 2-year retrospective study. Forensic Sci Int 194(1–3):9–14
Roberts IS, Benamore RE, Benbow EW et al (2012) Postmortem imaging as an alternative to autopsy in the diagnosis of adult deaths: a validation study. Lancet 379(9811):136–42
Aghayev E, Sonnenschein M, Jackowski C et al (2006) Postmortem radiology of fatal hemorrhage: measurements of cross-sectional areas of major blood vessels and volumes of aorta and spleen on MDCT and volumes of heart chambers on MRI. AJR 187(1):209–215
Kennedy D, Laing C, Tseng L et al (2010) Detection of active gastrointestinal hemorrhage with CT angiography: a 4(1/2)-year retrospective review. J Vasc Interv Radiol 21(6):848–855
Karhunen PJ, Servo A (1993) Sudden fatal or non-operable bleeding from ruptured intracranial aneurysm: evaluation by post-mortem angiography with vulcanising contrast medium. Int J Legal Med 106(2):55–59
Roberts I, Benamore R, Peebles C et al (2011) Diagnosis of coronary artery disease using minimally invasive autopsy: evaluation of a novel method of post-mortem coronary CT angiography. Clin Radiol 66(7):645–650, Technical report
Saunders S, Morgan B, Raj V et al (2011) Targeted post-mortem computed tomography cardiac angiography: proof of concept. Int J Legal Med 125(4):609–616
Jackowski C, Thali M, Sonnenschein M et al (2005) Virtopsy: postmortem minimally invasive angiography using cross section techniques—implementation and preliminary results. J Forensic Sci 50(5):1175–1186
Grabherr S, Djonov V, Friess A et al (2006) Postmortem angiography after vascular perfusion with diesel oil and a lipophilic contrast agent. AJR 187(5):W515–W523
Kominato Y, Fujikura T, Hata Y et al (2006) A case of postoperative hemorrhage after a hysterectomy in which a bleeding point of the left uterine artery was identified by postmortem angiography. Legal Med 6(3):187–189
Ruder T, Ketterer T, Preiss U et al (2011) Suicidal knife wound to the heart: challenges in reconstructing wound channels with postmortem CT and CT-angiography. Legal Medicine 13(2):91–94
Grabherr S, Djonov V, Yen K et al (2007) Postmortem angiography: review of former and current methods. AJR 188(3):832–838
Saunders S, Morgan B, Raj V, Rutty G (2010) Post-mortem computed tomography angiography: past, present and future. Forensic Sci Med Pathol 7(3):271–277
Grabherr S, Gygax E, Sollberger B et al (2008) Two-step post-mortem angiography with a modified heart–lung machine: preliminary results. AJR 190(2):345–351
Grabherr S, Doenz F, Steger B et al (2011) Multi-phase post-mortem CT angiography: development of a standardized protocol. Int J Legal Med 125(6):791–802
Michaud K, Grabherr S, Doenz F, Mangin P (2012) Evaluation of postmortem MDCT and MDCT-angiography for the investigation of sudden cardiac death related to atherosclerotic coronary artery disease. Int J Cardiovasc Imaging 28(7):1807–1822
Schneider B, Chevallier C, Dominguez A (2011) The forensic radiographer: a new member in the medicolegal team. Am J Forensic Med Pathol 33(1):30–36
Brinkmann B (1999) Harmonisation of medico-legal autopsy rules. Int J Legal Med 113(1):1–14
Jackowski C, Warntjes MJ, Berge J et al (2011) Magnetic resonance imaging goes postmortem: noninvasive detection and assessment of myocardial infarction by postmortem MRI. Eur Radiol 21(1):70–8
Yen K, Thali M, Aghayev E et al (2005) Strangulation signs: initial correlation of MRI, MSCT and forensic neck findings. J Magn Reson Imaging 22(4):501–510
Bouchireb K, Teychene AM, Rigal O et al (2010) Post-mortem MRI reveals CPT2 deficiency after sudden infant death. Eur J Pediatr 169(12):1561–1563
Acknowledgments
This study was financially supported by the Promotion Agency for Innovation of the Swiss Confederation (KTI Nr.10221.1 PFIW-IW) and the Leenards Foundation, Lausanne, Switzerland.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Christine, C., Francesco, D., Paul, V. et al. Postmortem computed tomography angiography vs. conventional autopsy: advantages and inconveniences of each method. Int J Legal Med 127, 981–989 (2013). https://doi.org/10.1007/s00414-012-0814-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-012-0814-3