Abstract
Purpose
Chronic cough is a common problem in various populations. The present study assessed the impact of cough and unmet needs in Korean patients with chronic cough.
Methods
This cross-sectional multi-center study enrolled adult patients newly referred to clinic for assessment of chronic cough. A second group of patients with unexplained chronic cough following detailed assessment were recruited for comparison. Patients completed self-reported questionnaires, including cough characteristics, impact of cough on daily life, and unmet needs.
Results
A total of 447 subjects were recruited from six referral clinics, including 408 with chronic cough and 39 with unexplained chronic cough. Almost all patients reported that cough impacted their daily lives. Psychosocial impacts were more evident in unexplained cough patients compared to newly referred patients. Approximately 75% of newly referred patients had previously sought medical care for cough on multiple occasions, but the effectiveness of treatment was limited (70.3%) or absent (17.3%). The most frequent unmet need was the ineffectiveness of treatment (49.3%), followed by unclear diagnosis (30.1%). The majority of participants ( > 80%) expressed the need for further information on accessing cough specialists and disease management. The main problem faced by unexplained cough patients was poor cough control despite treatment (64%).
Conclusions
Chronic cough has a substantial impact on daily life and is worst in those whose cough remains unexplained following assessment. Ineffectiveness of treatment and unclear diagnosis were major unmet needs. Medical information about chronic cough was also lacking. Improvements in the management of chronic cough patients in Korea are necessary.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Chronic cough is a prevalent condition in general populations worldwide [1]. It is a multi-factorial syndrome presenting as cough hypersensitivity [2], which is frequently comorbid with asthma, rhinitis/sinusitis, or gastroesophageal reflux disease (GERD) [3, 4]. Anatomic diagnostic protocol to treat these peripheral conditions in cough reflex pathways is considered generally successful [3, 4]. However, 10–40% of patients remained refractory or unexplained despite considerable diagnostic and therapeutic efforts [5], suggesting the needs to improve our management pathways.
Chronic cough is associated with significant impairment in quality of life, including physical, psychological, or social aspects [6,7,8]. A recent internet-based survey of European countries examined patients’ perspectives on the impact of cough and their unmet needs [9]. It recruited 1120 patients and found the negative impact of cough and limited effectiveness of current treatments across Europe [9]. However, the disease epidemiology, healthcare accessibility, and medical issues may vary among regions and populations. To our knowledge, the patients’ perspectives have not been studied in Korean patients. Based on the European survey protocol [9], we performed a multi-center study to identify the disease impact and unmet needs in Korean patients seeking medical care for chronic cough. We extended this study to include a comparison with patients with unexplained chronic cough to further address their unmet clinical needs as they form a significant workload in specialist clinics.
Materials and Methods
Study Population
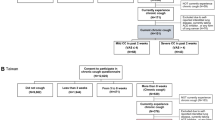
This prospective, multi-center study included adult patients visiting six large regional referral hospitals for chronic cough (defined as cough persisting longer than 8 weeks) [10] between February 2016 and November 2018. Patients were divided into two groups, one with chronic cough, consisting of patients newly referred for chronic cough (as their chief complaint), irrespective of underlying conditions and the other with unexplained chronic cough, consisting of patients with chronic cough of unknown etiology despite thorough investigation and therapeutic trials at the participating institutions [10]. The chronic cough group consisted of patients referred from primary or secondary care physicians, recruited to address overall unmet needs in seeking specialist care for cough. The unexplained chronic cough group was additionally recruited to address the specific disease experience in this treatment-refractory group. There was no overlap between two groups. All participants were consecutively recruited. The study protocols were approved by the Institutional Ethics Review Boards of all participating institutions.
Questionnaire Surveys
Structured questionnaires included demographic characteristics (age, sex, and smoking status), cough status, and unmet needs for chronic cough. The questionnaires for the chronic cough group, based on the European Lung Foundation study protocol [9], consisted of five categories: “About your cough (cough characteristics),” “How are you affected by cough? (impact of cough),” “Diagnosis of cough,” “Treatment of cough,” and “Support for patients with cough.” Surveys were administered prior to patients’ initial outpatient visits to the participating institution.
The questionnaires for the unexplained chronic cough group were modified versions of the questionnaires administered to patients with chronic cough [9], as well as including open-ended questions on unmet needs while receiving tertiary care.
Translation into the Korean version followed previous methodology [11]. Briefly, forward-back translation methodology was used by two bilingual professionals. They were asked to keep conceptual equivalence rather than linguistic uniformity. To check its comprehensibility and validate its cross-cultural adaptation, a pilot study was performed in ten subjects. The Korean version of the questionnaire is available upon request to the authors.
Statistical Analysis
Continuous variables were presented as mean ± standard deviation (SD). Categorical variables were expressed as number and frequency. Between-group differences were assessed using t-tests, Mann–Whitney U-tests, or chi-squared tests, as appropriate. Two-sided p values < 0.05 were considered statistically significant. All analyses were performed using Stata 15.1 software (Stata Corp, College Station, Texas, USA).
Results
Baseline Characteristics
A total of 447 subjects, including 408 with newly referred chronic cough and 39 with unexplained chronic cough, were recruited from the six participating institutions. A comparison of baseline characteristics in the two groups showed that patients with unexplained chronic cough were significantly older (62.4 ± 13.4 vs. 54.4 ± 15.9 years; p = 0.003), had a higher percentage of women (82.1% vs. 65.7%; p = 0.036), and had significantly longer duration of cough (p < 0.001) than patients with chronic cough (Table 1).
Impact of Chronic Cough
The effects of cough on activities of daily life, patients’ families and friends, and individuals with depression were analyzed (Fig. 1). Virtually all patients with chronic cough and unexplained chronic cough reported that cough impaired their daily life, either frequently (61.2% and 64.0%, respectively) or sometimes (37.9% and 36.0%, respectively). Both patient groups reported that cough disturbed their relationships with families and friends and led to depression or feeling fed up, but these psychosocial impacts of cough were more evident in the patients with unexplained chronic cough (Fig. 1).
Management and Treatment Experience in Patients with Chronic Cough
About 75% of patients in the chronic cough group reported that they had previously visited two or more clinics for cough. About 80% of patients had previously received one or more diagnoses for chronic cough, with rhinitis/rhinosinusitis (23.3%), asthma (22.6%), and bronchitis (20.4%) being the three most common conditions. Most patients reported that previous treatments for cough had limited (70.3%) or no (17.3%) effectiveness (Fig. 2). About two-thirds had tried over-the-counter (OTC) medicines to relieve cough, with most finding that these OTC drugs had limited (55.6%) or no (15.8%) effectiveness. Only 27.1% of respondents believed that their doctors had dealt with their cough thoroughly.
Unmet Needs in the Chronic Cough Group
The most common unmet need in the chronic cough group was the lack of effectiveness of treatment (49.3%), followed by unclear diagnosis (30.1%), medical costs (6.2%), and adverse effects of treatment (3.5%) (Fig. 3). Most patients reported difficulties in locating cough specialists (48.2%) or clinics (38.2%). Patients in this group wanted further information on cough treatment and prevention (55.1%), cough assessment (36.7%), and cough specialists (8.2%). Most patients (89.1%) reported that they were willing to attend a specialist cough clinic if available.
Unmet Needs in the Unexplained Chronic Cough Group
An open-ended questionnaire assessing unmet needs while receiving tertiary care was administered to the 39 patients with unexplained chronic cough. Two common items were generated: poor control of cough despite treatments (64.0%) and incurable coughing (36.0%). The majority (83.8%) reported a lack of information about their disease and wanted further information, including cough treatment (n = 7), prevention (n = 4), cure (n = 4), self-management (n = 2), general knowledge (n = 2), diagnosis (n = 2), causes (n = 2), and supplementary foods (n = 1).
Discussion
The present study assessed the impact of cough and unmet needs in Korean adult patients with chronic cough. Chronic cough was frequently associated with impairments in daily activities, impaired personal relationships with family and friends, and emotional reactions, such as feeling fed up or depressed. Despite management efforts, most patients found that previous treatments and OTC medications provided little or no effectiveness. Lack of treatment effects and unclear diagnosis were the two major unmet needs. Patients with unexplained cough were more likely to be female gender, older, and have a longer duration of cough compared to newly referred patients. The main problems faced by unexplained cough patients were poor cough control despite treatment (64%) and incurable coughing (36.0%). The majority of participants, including the patients already attending tertiary clinics, expressed the need for further information on accessing cough specialists and disease management.
These findings on the impact of cough in Korean patients are consistent with those of studies in the US and Europe [6, 7, 9], highlighting the unique characteristics of chronic cough. Cough can significantly impair wide aspects of daily life [7]. However, chronic cough may particularly result in social isolation, probably more so than other disease conditions. In the study by French et al. [7], the reasons a large proportion of cough patients sought medical care were related to the social domain, such as “others think something is wrong with me” (53%), “self-consciousness” (46%), “difficulty speaking on the telephone” (39%), “spouse cannot tolerate cough” (30%), or “stopped going to the movies” (16%) [7]. Similarly, most patients in the present study found that their cough disturbed family or friends, with the proportion being higher in patients with unexplained than with chronic cough.
One of the major unmet needs in our patients with chronic cough were “lack of treatment effects.” Although about 80% of study participants had previously received one or more diagnoses for chronic cough, they were still seeking medical care for persistent cough. Only 12.4% reported that their previous treatments were effective; however, as this study did not assess the details of previous treatments, it is difficult to determine whether these high failure rates indicate that currently available anti-tussive drugs were ineffective or whether anatomic diagnoses were insufficient. Meanwhile, about two-thirds of the patients had previously tried OTC medications for cough, with 71.4% reporting little or no effectiveness. The absence of effectiveness of OTC medications was rather expected, because their evidence is poor by modern standards including robust outcome measurement [12]. In addition, our patients with unexplained chronic cough attending tertiary clinics also pointed out “poor cough control despite treatments” (64%) and “incurable coughing” (36%) as their unmet needs. Randomized placebo-controlled trials have tested the efficacy of opioids [13] (codeine in Korea) or neuromodulators such as gabapentin [14] in patients with chronic refractory cough. However, their treatment response rates are only around 30–50%. These findings indicate an urgent need for more effective medications for cough control in patients with chronic cough.
The second most common unmet need was “unclear diagnosis,” reported by 30.1% in the chronic cough group. As this study did not obtain detailed information on previous diagnostic trials, it is difficult to determine whether this high rate is associated with diagnostic failure. Identifying underlying pathology is a key to manage chronic cough patients primarily; however, 10–40% of patients do not easily fit into any disease category, despite diagnostic and therapeutic trials, thus termed as chronic idiopathic, unexplained, or refractory cough [5]. There has been a prevalent perception among physicians that cough is always due to something else [15]; however, it is increasingly recognized that persistent hypersensitivity in the cough reflex pathways is the common mechanism underlying chronic cough [2, 16, 17]. Considering that persistent cough is the main reason for these patients to seek medical care, it is necessary that physicians will pay more attention to their cough problems and be active for cough control modalities. In our survey, only 27.1% felt that their doctors had dealt with their cough thoroughly.
Our study also found that there is a significant lack of medical information for chronic cough. Eighty-six percent of chronic cough patients have difficulty locating cough specialist clinics. Most study participants, including patients already attending tertiary clinics, reported their needs for further medical information on chronic cough. These findings indicate the need for improvement in the medical care for chronic cough in Korea.
In this study, we did not include a comparator group with other common respiratory disease conditions, such as patients with asthma or chronic obstructive pulmonary disease (COPD). We believe that such comparison would highlight distinct aspects of chronic cough in terms of the disease impact. In a previous study by Polley et al. [18], patients with chronic cough had more psychological issues than those with bronchiectasis but less functional impairment than those with COPD.
This study had several limitations. First, the survey questionnaires were not developed de novo for Korean patients but were adopted from protocols used in a recent European survey [9]. However, it was our intention to compare common items in the two populations. Second, we used only a few simple questions to assess the impact of cough, to make the survey protocol brief. Utilization of validated questionnaires for health-related or cough-specific quality of life would provide more precise information on the impact of cough. Third, patients were recruited from six large regional referral centers. In particular, about 75% of patients in the chronic cough group reported that they had previously visited two or more clinics for cough. Thus, the applicability of these results to primary care or general populations is unclear. The perspectives addressed here would reflect those of more symptomatic or less treatment-responsive patients. Fourth, the number of patients with unexplained chronic cough was relatively small (n = 39), and thus definitive comparisons were difficult to make. A large difference in the number of participants between two groups was related to our consecutive recruitment, and we suppose it reflects a small proportion of unexplained cough patients per overall chronic cough population. The ratio of these patients to those in the chronic cough group (9.6%; 39/408) was in line with the prevalence of chronic refractory cough patients in other countries (10–40%) [5]. The predominance of middle-aged women in our population was also consistent with previous reports [2]. Finally, we did not perform subgroup analyses of several cough phenotypes, such as asthmatic cough and reflux cough. Therefore, the relationship between phenotype and disease experience remains unclear.
In conclusion, the present study assessed the impact of cough and unmet needs in Korean patients with chronic cough. The impact of chronic cough was substantial, including psychosocial problems. Lack of treatment effects and unclear diagnosis were major unmet clinical needs. Information about cough specialists and disease management was also lacking. These findings indicate the necessity to improve levels of care and management of chronic cough patients in Korea.
References
Song WJ, Chang YS, Faruqi S, Kim JY, Kang MG, Kim S et al (2015) The global epidemiology of chronic cough in adults: a systematic review and meta-analysis. Eur Respir J 45:1479–1481
Morice AH, Millqvist E, Belvisi MG, Bieksiene K, Birring SS, Chung KF et al (2014) Expert opinion on the cough hypersensitivity syndrome in respiratory medicine. Eur Respir J 44:1132–1148
Morice AH, Fontana GA, Sovijarvi AR, Pistolesi M, Chung KF, Widdicombe J et al (2004) The diagnosis and management of chronic cough. Eur Respir J 24:481–492
Irwin RS, Baumann MH, Bolser DC, Boulet LP, Braman SS, Brightling CE et al (2006) Diagnosis and management of cough executive summary: accp evidence-based clinical practice guidelines. Chest 129:1S–23S
Mcgarvey L (2013) The difficult-to-treat, therapy-resistant cough: why are current cough treatments not working and what can we do? Pulm Pharmacol Ther 26:528–531
Birring SS, Prudon B, Carr AJ, Singh SJ, Morgan MD, Pavord ID (2003) Development of a symptom specific health status measure for patients with chronic cough: Leicester Cough Questionnaire (LCQ). Thorax 58:339–343
French CL, Irwin RS, Curley FJ, Krikorian CJ (1998) Impact of chronic cough on quality of life. Arch Intern Med 158:1657–1661
Song WJ, Morice AH, Kim MH, Lee SE, Jo EJ, Lee SM et al (2013) Cough in the elderly population: relationships with multiple comorbidity. PLoS ONE 8:E78081
Chamberlain SA, Garrod R, Douiri A, Masefield S, Powell P, Bucher C et al (2015) The impact of chronic cough: a cross-sectional European Survey. Lung 193:401–408
Song DJ, Song WJ, Kwon JW, Kim GW, Kim MA, Kim MY et al (2018) KAAACI evidence-based clinical practice guidelines for chronic cough in adults and children in Korea. Allergy Asthma Immunol Res 10:591–613
Song W-J, Lee S-H, Kang M-G, Kim J-Y, Kim M-Y, Jo E-J et al (2015) Validation of the korean version of the European Community Respiratory Health Survey Screening Questionnaire for use in epidemiologic studies for adult asthma. Asia Pac Allergy 5:25–31
Morice AH (2015) Over-the-counter cough medicines: new approaches. Pulm Pharmacol Ther 35:149–151
Morice AH, Menon MS, Mulrennan SA, Everett CF, Wright C, Jackson J et al (2007) Opiate therapy in chronic cough. Am J Respir Crit Care Med 175:312–315
Ryan NM, Birring SS, Gibson PG (2012) Gabapentin for refractory chronic cough: a randomised, double-blind, placebo-controlled trial. Lancet 380:1583–1589
Faruqi S, Murdoch RD, Allum F, Morice AH (2014) On the definition of chronic cough and current treatment pathways: an International Qualitative Study. Cough 10:5
Chung KF, Mcgarvey L, Mazzone SB (2013) Chronic cough as a neuropathic disorder. Lancet Respir Med 1:414–422
Song WJ, Morice AH (2017) Cough hypersensitivity syndrome: a few more steps forward. Allergy Asthma Immunol Res 9:394–402
Polley L, Yaman N, Heaney L, Cardwell C, Murtagh E, Ramsey J et al (2008) Impact of cough across different chronic respiratory diseases: comparison of two cough-specific health-related quality of life questionnaires. Chest 134:295–302
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declared that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kang, SY., Won, HK., Lee, S.M. et al. Impact of Cough and Unmet Needs in Chronic Cough: A Survey of Patients in Korea. Lung 197, 635–639 (2019). https://doi.org/10.1007/s00408-019-00258-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-019-00258-9