Abstract
Purpose
Studies that investigate the impact of chronic cough have largely focused on patients attending secondary care. Our aim was to investigate the opinions of the wider general population across Europe.
Methods
An internet survey was made available in 12 languages on the European Lung Foundation website, between January 2012 and April 2013.
Results
Of 1120 respondents from 29 different European countries, 67 % were female, mean age 51 years (SD 15), median cough duration 2–5 years. The majority of respondents reported cough impacted their quality of life, mood and ability to undertake activities. Despite 72 % of respondents having visited their doctor ≥3 times, only 53 % had received a diagnosis. Asthma was the most common diagnosis (23 %). Most respondents reported limited or no effectiveness of medications. 88 % of respondents reported that they would like more information to be available on chronic cough.
Conclusions
Chronic cough has a negative impact on quality of life. Further work is needed to raise awareness, promote management strategies, develop effective treatments and consider the educational and support needs of patients with chronic cough.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of chronic cough has been estimated as affecting 11–13 % of the population [1–4]. Chronic cough is associated with significant physical and psychological morbidity [5, 6]. Adverse physical symptoms associated with cough include syncope, incontinence, chest pain, headaches and sore throat. Depression, anxiety and social embarrassment are also common [5, 7, 8]. The impact of chronic cough has largely been investigated in patients attending specialist cough clinics [5, 6, 9]. Few studies have investigated the impact of chronic cough in patients based in the community. The aim of this study, in collaboration with the European Lung Foundation (ELF), was to investigate the impact of chronic cough from the patients’ perspective in a wide range of European countries. An internet-based survey was developed to investigate the impact, medical consultations, diagnoses, treatments and needs of patients with chronic cough.
Methods
Subjects
Adults with chronic cough (duration >8 weeks) of any cause were recruited using an internet-based survey. Exclusion criteria were acute and sub-acute cough, age <18 years and non-European country of residence. A patient information sheet was provided online on the ELF website. Participants who selected to complete the online survey were considered to have given implied consent. Secondary anonymised data from the survey were analysed.
Survey Development
Phase 1: Item Generation
A preliminary survey (21 items) was developed following a review of the chronic cough health-related quality-of-life (QoL) literature and published surveys of chronic cough. The survey was also reviewed and discussed within the European Respiratory Society (ERS) Chronic cough Taskforce (15 respiratory physicians from nine countries), a multi-disciplinary team (respiratory physician and physiotherapists, Kings College Hospital) and the ELF. The survey contained both open-ended and closed questions with response scales.
Phase 2: Survey Refinement
The survey was adapted for use on the internet and reduced to 17 items in response to feedback received during the item generation phase. The items were grouped into five categories: “About your cough”, “How are you affected by your cough?”, “Diagnosis of your cough”, “Treatment of your cough” and “Support for patients with cough” (Online Appendix A).
Phase 3: Translation Of Survey
The survey was translated by Web-Translations (Leeds, UK). Forward-back translation methodology was used by native speakers to ensure accuracy. The back-translated survey was checked by the original author (SSB) for accuracy, and the differences were reconciled during a harmonisation process. The survey was translated into 12 languages: English, German, French, Spanish, Greek, Romanian, Lithuanian, Swedish, Italian, Bulgarian, Polish and Russian.
Internet Survey
The survey was launched by the ELF on their website www.european-lung-foundation.org (website has now changed to www.europeanlung.org) using a Survey Monkey survey package. Google AdWords was used to advertise the survey on Google searches. This used keywords or search terms entered into a Google search website to return the cough survey in the Google results page and advertisement sidebar. The keywords set for this survey were “chronic cough”, “cough survey”, “a cough that won’t go away” and “can lung disease make you cough”. These key words were identified by the ELF, following review of the literature and online resources for cough. Keywords were translated and applied for each survey language. The survey was promoted by the ELF by developing advertisement posters in all survey languages with dissemination to all ERS members (>10,000) and ELF patient organisation network (>160 organisations). The posters were available on the ELF website to download. The survey was also promoted in the ELF monthly newsletter and via social media (Twitter and Facebook).
Analysis
Count data were expressed as frequencies and percentages of the total number of participants responding to each question. The data were analysed as a whole sample and then as sub-groups according to the country of residence (countries with >50 responders) and gender. Categorical data for “the impact of cough” questions (questions 5–8, Online Appendix A) were summarised as binary variables to enable calculation of the proportions of participants with the symptom. Open questions (questions 2, 16, 19 and 20; Online Appendix A) were analysed by frequency content analysis. Preliminary categories were further refined to generate consolidated themes. The data generated by questions relating to further information and support were merged for analysis (questions 19 and 20).
Results
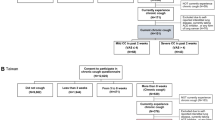
The survey was available between January 2012 and April 2013. 1968 participants responded and completed the survey; 1120 met the inclusion criteria. The reasons for excluding participants are stated in Fig. 1. Sixty-seven percent of respondents were female, the mean age of respondents was 51 years (SD 15, range 18–87) and 83 % were non-smokers (participant demographics are presented in Table 1). The respondents resided in 29 European countries (Fig. 2). The countries with the five highest response rates were United Kingdom (UK) (n = 136, 20 %), Germany (n = 114, 18 %), France (n = 76, 11 %), Italy (n = 70, 10 %) and Poland (n = 67, 10 %).
Diagnosis
Median duration of cough was between 2 and 5 years. There were two peaks of cough duration; twenty-two percent, reported an early chronic cough (3–6 months duration) and a similar number, twenty percent reported cough duration of 10 or more years (Fig. 3). Fifty-three percent (n = 562) of respondents reported that they had been given a diagnosis for their cough (Fig. 4). Seven percent of respondents who had been given a diagnosis had been given two or more diagnoses. Asthma was the most common diagnosis reported (23 %; Fig. 4).
Cough diagnoses of survey respondents. Data presented as number of survey respondents. GORD Gastro-oesophageal reflux, PND post-nasal drip, COPD chronic obstructive respiratory disease, ACE-I angiotensin-converting-enzyme inhibitor, ILD interstitial lung disease, Other includes non-disclosed diagnoses of cough, PCD primary cillary dyskinesia. First, second and third diagnoses were defined as the first, second and third diagnoses listed by survey respondents in response to Survey Question 10
Impact of Chronic Cough
Ninety-six percent (n = 1055) of responders reported that their cough affected their QoL. Eighty-one percent (n = 890) reported that their cough affected the activities they liked to do. Ninety-one percent (n = 1000) reported feeling fed up and depressed because of their cough and 94 % (n = 1030) reported that their cough disturbed or worried their family and friends. The impact of cough was consistent across the top five countries of residence for the respondents (Table 2).
There were significant gender differences in the limitation of activities due to cough; a significantly higher proportion of women (87 %; confidence interval (CI) 84–90 %) than men (77 %; 95 CI 72–82 %) reported limitations (difference in proportion 10 %; CI 4–16 %). More women (94 %; CI 92–96 %) than men (90 %; CI 85–93 %) reported feeling fed up or depressed due to their cough (difference in proportion 5 %; 95 CI 0–9 %). No significant differences in population proportions were found between gender for impact on QoL or on family and friends.
Management and Treatment of Chronic Cough
The majority of respondents had seen a doctor about their cough (Table 1). Seventy-two percent of respondents had seen a doctor ≥3 times in relation to their cough. Thirteen percent reported that they had attended a specialist cough clinic. Only 30 % of respondents felt their doctor had dealt with their cough thoroughly. Respondents were asked in an open-ended question why they had first consulted their doctor. This question generated seven themes: the characteristics of the cough (n = 422), physical symptoms associated with cough (n = 380), possible viral infection symptoms (n = 140), psychological symptoms associated with cough (n = 88), to consult a doctor about existing respiratory or other health condition (n = 80), social symptoms associated with cough (n = 76) and for diagnosis/assessment and treatment for the cough (n = 31), (Online Appendix B). Some examples of quotations from respondents are listed in Online Appendix C.
Most respondents reported limited (57 %) or no (36 %) effectiveness of medications they had tried for cough. Only 7 % reported that medications they had tried for their cough were effective. Medications found helpful for their cough were reported by 222 responders (Question 16—open-ended question; see Table 3). Sixty-nine percent of respondents reported that over-the-counter medications were not effective.
Information and Support
Eighty-eight percent of respondents reported that they would like more information on chronic cough to be available and 78 % reported that they would like to receive more information about the ERS/ELF Chronic cough Task Force. The open-ended questions concerning further information and support needs of the respondents generated 20 themes (Table 4). The two most common themes were the need for further patient information relating to the treatment and on causes of cough. Examples of quotations from respondents requesting further information and support are listed in Online Appendix D.
Discussion
This community-based survey investigated the impact of chronic cough in a large number of participants living in 29 European countries. The demographics of respondents to this survey were consistent with previous studies of chronic cough that report a middle aged, female predominance [10–13]. There was an adverse impact of cough on health-related QoL in most respondents, which was consistent across the top five response countries. The impact on activities was more significant in females compared to males. Most respondents reported that their doctor had not ‘dealt with their cough thoroughly’ and that medications were largely ineffective.
This survey has highlighted the significant adverse impact of chronic cough to the individual. The respondents had consulted their physician for a wide range of reasons, such as the severity of cough, adverse physical and psychological symptoms associated with cough and the social impact. The effect on health-related QoL was consistent with previous studies conducted in specialist Cough Clinics by French et al. [9] and Birring et al. [6]. In contrast to French et al. [14], a gender difference was not found in the impact on health-related QoL. This may be because we did not use validated questionnaires such as the cough-specific QoL questionnaire (CQLQ) [15] and the Leicester cough questionnaire (LCQ) [6] to assess health-related QoL. Most respondents also reported feeling ‘fed up or depressed’ because of their cough. This finding is consistent with those of Dicipingaitis et al. [8] and McGarvey et al. [7], who also reported significant depressive symptomatology in up to 50 % of participants. The prevalence of depressive symptoms in our study was greater than this (91 %), though again this was not measured by validated questionnaires; hence the severity of these reported symptoms in our respondents is unknown.
Only 53 % of the survey respondents had been given a suggested diagnosis for their cough. This was despite the respondents having consulted their doctor on multiple occasions. However, it is possible that some respondents were still undergoing investigations for the cause of their cough and only 13 % of our participants had been assessed in specialist cough clinics. These factors may have contributed to the high prevalence of unexplained chronic cough. Only 30 % of respondents felt that their doctor had dealt with their cough thoroughly. When a diagnosis was suggested, the most common cause was asthma (23 %). Gastro-oesophageal reflux disease and upper airway cough syndrome (post-nasal drip) were also common causes, consistent with previous studies of cough that investigated subjects with the Anatomic Diagnostic Protocol as recommended by chronic cough guidelines [12, 16–18]. As expected, some respondents reported multiple causes of cough.
Our study findings suggest that there is room for improvement in the management of patients with chronic cough. One approach is to increase awareness of this condition and improve the implementation of chronic cough management guidelines in both primary and secondary care. Another approach could be to improve patient access to specialist cough clinics, by increasing the number of such clinics. A key finding reported by respondents was that their medications, including over-the-counter medications, were ineffective. The reasons why other prescribed and over-the counter medications were ineffective are unclear, and was beyond the scope of this study. Inadequate assessment of patients, dose/duration and non-compliance of medications and misdiagnosis could all be potential explanations [16, 17]. The reasons for treatment failure warrant further investigation.
A novel internet-based survey was used in this study to investigate the impact of chronic cough. This method was simple to set up, low-cost and one that provided data output in an electronic format that was ready to analyse. It also facilitated the recruitment of participants from across Europe. The use of the internet did not inhibit elderly participants; the age range of our study was 18–87 years. Few surveys have specifically assessed the impact of chronic cough in detail. Everett et al. [19] surveyed 373 subjects with chronic cough in the community based in the UK that responded initially to a radio broadcast. Everett et al. [19] also found that chronic cough was associated with a significant adverse impact on physical, psychological and social wellbeing of subjects. The strength of our study in contrast to Everett et al. [19] was a larger sample size of participants with chronic cough, recruitment from 29 European countries and the additional capture of qualitative data (for example, participants’ views on information and support for cough). Fujimara et al. [20] surveyed 232 participants with chronic cough registered with a research company via e-mail. The recruitment of volunteers from a research company database is likely to have introduced a selection bias. Seventy-four percent of participants were male, which is in sharp contrast to most studies of chronic cough, which report a female predominance. Forty-four percent of participants had not consulted their doctor regarding their cough, and 75 % were satisfied with over-the-counter cough medications. This reflects the high number of participants with acute and sub-acute cough in their study. Cough, however, was associated with significant psychosocial impact on the subject, and females were more affected than males. Ford et al. [2] identified 481 participants with chronic cough in a survey of a community based in Yorkshire, UK. The cough was considered severe in approximately half of these subjects based on the disruption to activities of daily living. However, this study did not report the psychosocial impact, access to specialist care or treatments used for cough. Adams et al. [21] identified 611 participants with chronic cough in a survey of a community based in Adelaide, Australia. Chronic dry cough was more common in participants who were male, current smokers and elderly. Cough was associated with significant psychological morbidity and impairment in health-related QoL, but this study also did not investigate the access to specialist care, treatments and information/support for participants.
There are a number of limitations with this study. Validated health-related QoL, activity or depression questionnaires were not used. We used a small selection of questions derived from the literature review of health-related QoL literature and multi-disciplinary discussion. This was to keep the survey brief, and therefore encourage completion by respondents. A significant number of respondents were excluded as they did not answer any of the cough-related questions. This may have been minimised using a shorter questionnaire. The diagnoses and medications were not verified by checking medical records, as this was not feasible in this study. The use of the internet to recruit participants seeking medical advice may have led to bias, although the wide age range of our participants and a clinical phenotype consistent with previous studies of chronic cough suggests that this bias may not have been as much as expected [10–13]. Studies of the general population, perhaps by telephone, would minimise selection bias but are likely to be costly and unfeasible. The recruitment of participants is likely to have been greater if we had used a commercial Google search strategy, for example a featured advertisement, rather than the Google AdWords account. The use of other search engines and strategies may have increased recruitment of subjects. Our data does, however, suggest that the internet has the potential to recruit a large number of participants for survey-based research. Our survey focused on exploring the impact of chronic cough; however, acute cough is also known to cause a significant impact on quality of life [22]. Future studies might explore usefully the impact of acute cough across Europe and serve to allow comparison with the findings of this present study.
In conclusion, chronic cough was associated with a significant impact on their daily activities and health-related QoL in this European study. Cough was undiagnosed in 47 % of respondents. The majority of respondents said that they would like further information, support and access to specialist cough clinics. This suggests that much more work needs to be done to promote awareness of this condition, implement clinical guidelines and improve access to specialist care. This is best achieved in collaboration with patient and healthcare professional societies, such as the ELF and the ERS.
References
Montnémery P et al (1998) Prevalence of obstructive lung diseases and respiratory symptoms in southern Sweden. Respir Med 92(12):1337–1345
Ford AC et al (2006) Cough in the community: a cross sectional survey and the relationship to gastrointestinal symptoms. Thorax 61(11):975–979
Cullinan P (1992) Persistent cough and sputum: prevalence and clinical characteristics in south east England. Respir Med 86(2):143–149
Lundbäck B et al (1991) Obstructive lung disease in northern Sweden: respiratory symptoms assessed in a postal survey. Eur Respir J 4(3):257–266
Brignall K, Jayaraman B, Birring SS (2008) Quality of life and psychosocial aspects of cough. Lung 186(Suppl 1):S55–S58
Birring SS et al (2003) Development of a symptom specific health status measure for patients with chronic cough: Leicester Cough Questionnaire (LCQ). Thorax 58(4):339–343
McGarvey L et al (2006) Prevalence of psychomorbidity among patients with chronic cough. Cough 2(1):4
Dicpinigaitis PV, Tso R, Banauch G (2006) Prevalence of depressive symptoms among patients with chronic cough. Chest 130(6):1839–1843
French CL et al (1998) Impact of chronic cough on quality of life. Arch Intern Med 158(15):1657–1661
Birring SS et al (2003) Respiratory symptoms in patients with treated hypothyroidism and inflammatory bowel disease. Thorax 58(6):533–536
Morice A et al (2014) Greater worldwide preponderence of chronic cough in women: a manifestation of enhanced somatosensory response? Eur Respir J 44(5):1149–1155
Morice AH et al (2006) Recommendations for the management of cough in adults. Thorax 61(Suppl 1):i1–i24
Morice AH (2002) Epidemiology of cough. Pulm Pharmacol Ther 15(3):253–259
French CT, Fletcher KE, Irwin RS (2004) Gender differences in health-related quality of life in patients complaining of chronic cough. Chest 125(2):482–488
French CT et al (2002) Evaluation of a cough-specific quality-of-life questionnaire. Chest 121(4):1123–1131
Irwin RS, Madison JM (2000) Anatomical diagnostic protocol in evaluating chronic cough with specific reference to gastroesophageal reflux disease. Am J Med 108(Suppl 4a):126S–130S
Morice AH et al (2004) The diagnosis and management of chronic cough. Eur Respir J 24(3):481–492
Irwin R et al (2006) Diagnosis and management of cough executive summary: ACCP evidence-based clinical practice guidelines. Chest 129(1 Suppl):1S–23S
Everett CF et al (2007) Chronic persistent cough in the community: a questionnaire survey. Cough 3:5
Fujimura M (2012) Frequency of persistent cough and trends in seeking medical care and treatment-results of an internet survey. Allergol Int 61(4):573–581
Adams RJ et al (2009) Associations of physical and mental health problems with chronic cough in a representative population cohort. Cough 5:10
Yousaf N et al (2011) The assessment of quality of life in acute cough with the Leicester Cough Questionnaire (LCQ-acute). Cough 7(1):4
Acknowledgments
We would like to thank our colleagues at the ERS Chronic Cough Taskforce for their valuable feedback during the development of the survey, ERS Chronic Taskforce members: Maria Belvisi, Kristina Bieksiene, Kian Fan Chung, Peter Dicpingaitis, Robert W. Dal Negro, Ahmad Kantar, Lorcan P. McGarvey, Eva Millqvist, Raimundas Sakalauskas, Jaclyn A. Smith. We also would like to thank all the respondents to the survey.
Conflict of interest
Authors Chamberlain, Garrod, Douiri, Bücher, Masefield, Powell, Birring declare that they have no conflict of interest. Author Pandyan has received research grants from the National Institute of Health Research and Pneumacare, he also received educational support from Allergan Limited, Biometrics Limited and GlaxoSmithKline. Author AM has received research grants from Boehringer Ingelheim, Cheisi Pharma, Novartis Pharmaceuticals, Orion Pharma UK, Procter & Gamble Health Sciences, Pfizer, Pharmaxis, Profile Pharma, MPEX Pharmaceuticals, PPD Development, Almirall, Seekacure, Philips Home Healthcare Solutions, Glenmark, Harrison Clinical Research, Janssen, Gilead, Bayer, Astrazeneca, Genentech, Bionoria, PRA International, GlaxoSmithKline, Allianz Global, Guangzhou Institute of Respiratory Disease, Cardiff Chest Federation, British Pharmacological Society, Italian Society of Respiratory Medicine, Drug Information Association, SRxA USA, Association of Inhalation Toxicologists, Ardmore Healthcare Limited, Actelion, Hellenic Society of Respiratory and Occupational Chest Diseases, Primary Care respiratory Society UK, TREAT Education USA, National Health and Lung Institute.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chamberlain, S.A.F., Garrod, R., Douiri, A. et al. The Impact of Chronic Cough: A Cross-Sectional European Survey. Lung 193, 401–408 (2015). https://doi.org/10.1007/s00408-015-9701-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-015-9701-2