Abstract
Tracheobronchopathia osteochondroplastica (TO) is a rare disorder of the large airways characterized by the development of submucosal cartilaginous and bony nodules. The nodules involve the anterior and lateral walls and typically spare the posterior membranous wall. The clinical presentation of TO is variable and ranges from incidental diagnosis in asymptomatic patients during workup or management for unrelated medical problems, to devastating disease with central airway obstruction. Bronchoscopy remains the gold standard for diagnosing this condition. Radiographic studies play an important role in suggesting the diagnosis of TO and in the follow-up of this condition. The treatment of TO is usually symptomatic. with emphasis on the management and prevention of recurrent respiratory infections. Bronchoscopic or surgical treatment is usually reserved for symptomatic patients with severe airway narrowing and airflow obstruction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
The report by Darjani et al. [1] describes their experience with tracheobronchopathia osteochondroplastica (TO). They treated ten symptomatic patients with this rare disorder over a period of 6 years in an interventional pulmonary unit affiliated with a referral center for respiratory disorders. Their report adds to the growing body of literature related to this rare airway disorder. The article by Darjani et al. raises interesting questions and intriguing observations about the incidence, clinical presentation, and diagnosis of this rare condition. It also improves our knowledge about associated medical conditions and potential treatment options for symptomatic patients with severe disease and airway obstruction. The following sections present a literature review of this rare condition and discuss the pertinent issues related to Darjani et al.’s [1] report.
Introduction
TO is a rare disorder of the large airways characterized by the development of submucosal cartilaginous and bony nodules. The nodules involve the anterior and lateral walls and typically spare the posterior membranous wall because of the absence of cartilage in this region of the airway. Laryngeal involvement has also been described. Calcification and ossification of the nodules are common, with protrusion of the nodules into the airway lumen [2]. The bony nodules may contain functional bone marrow. Squamous metaplasia and inflammatory changes of the mucosa can alter the efficiency of clearing respiratory secretions and lead to recurrent pulmonary infections [3]. Large and confluent nodules can cause variable degrees of symptomatic airway obstruction.
Incidence
TO was originally described by Rokitansky, Luschka, and Wilks in the mid-19th century [4, 5]. Less than 400 cases were subsequently reported in the literature (to our review). The two largest series involved 30 and 41 cases of TO, respectively [6, 7]. While this rare disorder was originally described at autopsy, the development of bronchoscopy and airway imaging techniques improved its detection and follow-up. Increasingly, cases are reported after bronchoscopic examination and evaluation by thoracic computed tomography (CT scan) for various pulmonary symptoms. The overall incidence of this condition remains unknown. However, reports, including the article by Darjani et al. [1], shed more light on this issue. While the incidence of TO has been reported to be in the range of 2-3 per 1000 autopsies [8–10], this would be expected to vary significantly depending on each specific study population’s characteristics and symptoms. Diagnosis by imaging or bronchoscopy would also be expected to affect the reported incidence of TO, as bronchoscopy is probably more sensitive and specific. This is clearly illustrated in a recent report by Decalmer et al. [11] where TO was reported in a group of patients referred for unexplained chronic persistent cough unresponsive to treatment. Seven cases of TO were diagnosed in that report [11] among 125 patients (where 82 patients had bronchoscopy performed for the sole indication of chronic cough). Primer [12] reported four cases incidentally found during 550 bronchoscopies. The incidence of TO in the report by Darjani et al. [1] (0.11%) is similar to other bronchoscopy reports in the literature.
Clinical Presentation
The clinical presentation of TO is variable and ranges from incidental diagnosis in asymptomatic patients during workup or management for unrelated medical problems [7, 13, 14] to devastating disease with central airway obstruction [15]. It has been suggested that only half of the people with TO will be diagnosed in their lifetime [16], but this number will likely increase as more complex diagnostic radiographic studies and bronchoscopies are performed for various medical problems.
Chronic cough appears to be the most common clinical presentation in symptomatic patients [7, 14]. Other symptoms include hemoptysis, chronic sputum production, wheezing, hoarseness and dyspnea (Table 1). Recurrent respiratory infections and related symptoms caused by interrupted mucociliary clearance are also common. The clinical presentation is therefore nonspecific, which leads to significant delays in establishing the diagnosis of this rare condition. In some case series, symptoms were present for years or even decades before definitive diagnosis [7, 17]. The diagnosis is usually established in the fourth through the seventh decade without gender predominance [6, 7, 18]. The diagnosis has rarely been reported in children, including reports of 12- and 9-year-old patients [6, 19]. In the Darjani et al. [1] report, the mean age at the time of diagnosis is 51 years and the youngest patient was 16 years old. Dyspnea on exertion and chronic cough were the most frequent presenting symptoms in their series, reflecting the severity of the disease at the time of diagnosis.
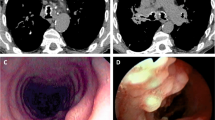
Bronchoscopy
Because the clinical presentation of TO is nonspecific, the diagnosis is usually made during bronchoscopy or by computed tomography and can be confirmed by bronchoscopic biopsies. Bronchoscopy remains the gold standard for the diagnosis of this condition. Hard sessile nodules arising from the anterior and lateral walls of the airway, typically sparing the posterior membrane, give a classic appearance that can be easily recognized (Fig. 1). However, extension of the nodules to the posterior tracheal wall was reported at bronchoscopy in 15% of patients in the largest available series [7]. The nodules are typically small (1–10 mm in diameter) and can be diffuse, scattered, or confluent. Large confluent nodules can protrude into the airway lumen and cause significant airway obstruction. The proximal and midtrachea are commonly involved, with less involvement of the mainstem bronchi, lobar, and segmental airways, respectively. Subglottic space and laryngeal involvement are less common but can be found on close examination in some patients [7, 14, 20].
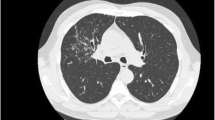
Radiographic Studies
Radiographic studies play an important role in suggesting the diagnosis of TO and in the follow-up of this condition. However, subtle radiographic findings can be overlooked, especially in mild cases. While the regular chest radiograph frequently is normal, it can show irregularity, narrowing, scalloping, or calcification of the trachea and mainstem bronchi, especially with overpenetrated studies. Complications of TO, including pneumonia, atelectasis, and bronchiectasis, may be the only findings seen on the chest radiographs [21]. This lack of sensitivity and specificity of the chest radiographs is illustrated in the report by Darjani et al. [1] as four of ten patients had normal chest radiographs and none had changes in the trachea or mainstem bronchi that were specific for TO. The CT scan is generally more sensitive and specific. It can show the typical features of TO with multiple calcified or noncalcified nodules that protrude into the airway lumen (Fig. 2). Involvement of the posterior wall of the trachea or mainstem bronchi should raise the suspicion for other conditions, including relapsing polychondritis, sarcoidosis, amyloidosis, and papillomatosis [22, 23]. Calcification associated with TO should be differentiated from diffuse tracheobronchial calcification seen with advanced age or other conditions such as tuberculosis, carcinoma, Wegener’s granulomatosis, and fibroma, among others [18, 24]. In the largest available series, CT scans detected dense submucosal nodules and calcifications in 74 and 61% of the cases, respectively [7]. CT scans showed suggestive findings in nine of ten patients in Darjani et al.’s report [1]. Bronchoscopic confirmation should be considered in symptomatic patients when this diagnosis is suspected by clinical presentation and suggestive radiographic studies.
Pulmonary Function Tests
Pulmonary function tests (PFT) are frequently normal, as mild luminal narrowing of the airway does not cause significant airflow obstruction. In symptomatic patients, however, airflow obstruction can be found with reduction in the FEV1 and FEV1/FVC, as the large central airways can be severely narrowed. The pattern seen on a flow volume loop in patients with severe TO associated with large airway obstruction can be differentiated from that seen with chronic obstructive pulmonary disease (COPD) due to cigarette smoking (Fig. 3). TO patients with significant large airway obstruction can have inspiratory and/or expiratory airflow limitation on flow volume loops [7, 17, 25], depending on the location and severity of the airflow-limiting endobronchial disease. Such patterns on the flow volume loop, along with other PFT indices, radiographic studies, and careful bronchoscopic evaluation, can help predict potential response to bronchoscopic or surgical interventions in symptomatic patients with severe TO and air flow obstruction. This is important because patients with TO can have underlying severe COPD which can be primarily responsible for their pulmonary symptoms and limitations. Restrictive physiology is less common and is usually associated with secondary atelectasis or other underlying restrictive lung disease. In Darjani et al.’s report [1], eight of ten patients had significant impairment in spirometric testing at the time of diagnosis.
Flow volume loops: different patterns that can be seen in upper airway obstruction related to severe TO. This ranges from normal flow volume loop (a) to severe fixed obstruction during inspiration and expiration (b). Variable airflow obstruction during inspiration (c) or expiration (d) can be seen depending on the level and degree of the endobronchial obstructing disease. Classic COPD pattern on flow-volume loop (e) can be seen in patients with TO and underlying COPD
Bronchoscopic Biopsies
The submucosal bony and cartilaginous nodules can be continuous with the perichondrium of the central airway rings and can demonstrate calcification or hematopoeitic bone marrow [7, 10]. Mucosal squamous metaplasia is also common. Flexible bronchoscopic biopsies could be difficult due to the hard nature of the nodules [26]. This is illustrated by a diagnostic yield of 55% after the initial biopsy by flexible bronchoscopy and 70% after repeated biopsies in the largest available series [7]. Table 2 and Figure 4 summarize the histopathologic findings in TO. Histopathologic confirmation of the diagnosis is reasonable, but the typical appearance during bronchoscopy and the benign nature of this condition has led some authors to question the need for this confirmation [2, 26]. While this conservative approach seems reasonable for asymptomatic patients with an incidental diagnosis, we agree with Darjani et al. [1] and others [27, 28] that histopathologic confirmation, coupled with bacteriologic assessment, is reasonable in the majority of cases. This is because of the rare nature of TO, the lack of familiarity of most bronchoscopists with this condition, and the need to rule out other differential diagnoses and evaluate for other associated conditions. This recommendation is especially relevant to symptomatic patients who might require more invasive therapeutic interventions.
Possible Etiologies
The etiology of TO remains largely unknown. Several theories about its pathogenesis and associated conditions have been reported [29]. Virchow (in 1863) originally proposed that in this condition, ecchondrosis and exostosis arise from the cartilaginous rings and this is followed by subsequent ossification. Aschoff and later Dalgaard [30, 31] suggested metaplasia of the elastic connective tissue as one possible mechanism. Bone morphogenetic protein-2 (BMP-2) may have an important role in nodule formation and act synergistically with transforming growth factor β1 (TGF-β1) to promote an inductive cascade of TO nodules in the tracheal submucosa [32]. This generally supports both the ecchondrosis/exostosis and metaplasia theories of TO formation [7]. Nodules continuous with the perichondrium of the airway cartilaginous rings and other free lesions (not related to the airway cartilaginous rings) have been reported [32, 33]. The effect of chronic irritation and cough on the development and progression of TO remain unclear. Squamous metaplasia is a common finding in TO, but this could be secondary to the chronic and irritant nature of this condition. Primary squamous metaplasia, followed by cartilage and bone metaplasia, was also suggested as a potential mechanism [7, 34]. The possibility that TO is an end-stage of airway amyloidosis has also been suggested [29, 35, 36]. This theory is not supported by the available literature and the association between both conditions is uncommon. An association between TO and atrophic rhinitis (ozena) has also been reported [6, 7, 34, 37]. Squamous metaplasia of the nasal and large airway mucosa can be a feature of both conditions and was seen in two of ten patients in the report by Darjani et al. [1]. Klebsiella ozaenae was reported in 20% of patients with TO in the largest reported series [7]. However, a direct role for this bacteria in the pathogenesis of TO has not been established. The majority of patients with ozena do not have the features of TO. Other associations, including familial occurrence, malignancy, typical and atypical mycobacterial infections, and autoimmune disease, have been sporadic and probably coincidental.
Treatment
The treatment of TO is usually symptomatic and nonspecific. It is not possible at this point to prevent the development and progression of this disease or remove all the airway lesions using any available treatment or intervention. Fortunately, this disease is rare; most of the cases are asymptomatic (discovered incidentally during bronchoscopy, imaging studies, or postmortem), and the progression of TO is usually minimal and slow. In the largest published series [7], 45% of the patients who were diagnosed with TO and were followed for a mean of 7 years showed progression. This progression was minimal in the majority and was significant in only 17% of patients. The treatment approach for symptomatic patients is primarily geared toward managing potentially recurrent pulmonary infections, improving clearance of secretions, using bronchodilators and inhaled corticosteroids, and treating associated pulmonary conditions that include COPD, asthma, and bronchiectasis. Specific treatment of the airway lesions is usually reserved for symptomatic patients with severe airway narrowing and airflow obstruction. This is illustrated in the largest published series, with only 1 of 41 patients requiring bronchoscopic laser therapy and 1 of 41 patients requiring tracheostomy [7]. Proposed specific palliative treatments in severe cases with symptomatic airway obstruction include bronchoscopic laser therapy with mechanical removal using the biopsy forceps or the bevel of the rigid bronchoscope [14, 27, 38], thoracic surgical interventions [15, 39, 40], and radiation therapy [41, 42]. The hard nature of the nodular protrusions limits the bronchoscopic therapeutic options for TO, while the diffuse and multilevel involvement of the airway limits the surgical approaches. Radiation therapy cannot be recommended based on the few reported cases.
The report by Darjani et al. [1] represents the largest series of bronchoscopic management for this large airway disorder in which laser photovaporization therapy is used in ten symptomatic patients. This was combined with mechanical debulking using the tip of the rigid bronchoscope (coring) and the flexible biopsy forceps in eight patients with confluent and diffuse disease. Two symptomatic patients with normal baseline FEV1 and scattered disease were managed with bronchoscopic laser therapy alone. All of their patients were symptomatic, with dyspnea on exertion as the most common symptom (9/10 patients). Airflow obstruction was seen in eight of the ten patients. They reported significant improvement in symptoms and lung function in four of ten patients after 8–30 months of follow-up. The two patients with normal FEV1 at baseline showed post-treatment improvement in symptoms after 6 and 36 months of follow-up, respectively. Three of the ten patients did not have symptomatic or spirometric improvements after 18, 22, and 36 months of follow-up, respectively. One of their ten patients died after 6 years of follow-up. She had recurrent bronchoscopic interventions and stent placement for her original disease and subsequent airway stenosis.
The symptomatic and spirometric improvement in four of their ten patients with impaired baseline FEV1 is expected, as three of the four did not have a history of smoking, leading to the conclusion that most their spirometric impairment and symptoms at baseline were probably related to the underlying TO. In fact, three of the four had normalization of the FEV1 after treatment. On the other hand, all three patients who did not improve after treatment had a history of smoking and baseline severe impairment in the FEV1, leading us to conclude that a significant proportion of their symptoms and obstructive airway disease was related to underlying COPD. It is in patients similar to this latter group that further physiologic evaluation, including flow volume loops, other PFT indices, and complex radiographic and bronchoscopic evaluation, could help predict a significant contribution of large airway obstruction to symptoms and, hence, predict response to bronchoscopic interventions. A similar approach was recently proposed for treatment of large airway obstruction related to malignancy [43] (recognizing the different nature of airway obstruction associated with TO). Finally, the symptomatic response that was reported in the two patients with baseline cough and dyspnea who had scattered disease and normal baseline FEV1 is intriguing. Turbulent airflow and impaired mucociliary clearance were implicated in cough and other symptoms related to TO [3, 17]. It would be plausible if bronchoscopic intervention improves such factors. However, this remains speculation and is not supported by sufficient evidence at this point.
Summary
In conclusion, TO is a rare disease of the large airways, which is more frequently reported now as a result of the increasing number of bronchoscopies and radiographic studies performed for evaluation of pulmonary disorders. The majority of cases are discovered incidentally and are not suspected prior to bronchoscopy or radiographic studies. Severe symptomatic disease with central airway obstruction requiring specific intervention appears to be exceptionally rare. The report by Darjani et al. [1] reflects their experience with a selected patient population that was referred to an interventional pulmonary unit at a tertiary center. Ten symptomatic patients with TO were treated with bronchoscopic laser photovaporization and mechanical debridement. Their report illustrates several interesting features and areas of discussion about this condition. The treatment of TO remains largely conservative and symptomatic, with bronchoscopic interventions reserved for selective symptomatic patients with severe disease and significant large airway obstruction. More data about treatment outcomes and longer-term follow-up will be necessary before recommending bronchoscopic interventions or other techniques for less severe disease. This report illustrates the need to develop physiologic, radiographic, and bronchoscopic criteria that could predict response to treatment of large airway obstruction. Registries like GERM “OP” [7] and reports similar to that of Darjani et al. [1] will further help us understand TO and other rare pulmonary disorders.
References
Darjani JHR, Radpey B, Kharabian S, Masjedi MR (2008) Tracheobronchopathia osteochondroplastica: presentation of ten cases and review of the literature. Lung 186
Prakash UB (2002) Tracheobronchopathia osteochondroplastica. Semin Respir Crit Care Med 23:167–175
Chen AY, Donovan DT (1997) Impaired ciliary clearance from tracheopathia osteoplastica of the upper respiratory tract. Otolaryngol Head Neck Surg 117:S102–S104
Wilks S (1857) Ossific deposits on larynx, trachea, and bronchi. Trans Pathol Soc Lond 8:88
Meyer CN, Dossing M, Broholm H (1997) Tracheobronchopathia osteochondroplastica. Respir Med 91:499–502
Harma RA, Suurkari S (1977) Tracheopathia chondro-osteoplastica. A clinical study of thirty cases. Acta Otolaryngol 84:118–123
Leske V, Lazor R, Coetmeur D, Crestani B, Chatte G, Cordier JF (2001) Tracheobronchopathia osteochondroplastica: a study of 41 patients. Medicine (Baltimore) 80:378–390
Ragaini DL, Piccol DP (1957) Trachea-bronchopathia chondro-osteoplastica. Riv Anat Put 13(188–208):289–338
Pounder DJ, Pieterse AS (1982) Tracheopathia osteoplastica: report of four cases. Pathology 14:429–433
Pounder DJ, Pieterse AS (1982) Tracheopathia osteoplastica: a study of the minimal lesion. J Pathol 138:235–239
Decalmer S, Woodcock A, Greaves M, Howe M, Smith J (2007) Airway abnormalities at flexible bronchoscopy in patients with chronic cough. Eur Respir J 30:1138–1142
Primer G (1979) Tracheobronchopathia osteochondroplastica. Prax Klin Pneumol 33:1060–1063
Thomas D, Stonell C, Hasan K (2001) Tracheobronchopathia osteoplastica: incidental finding at tracheal intubation. Br J Anaesth 87:515–517
Nienhuis DM, Prakash UB, Edell ES (1990) Tracheobronchopathia osteochondroplastica. Ann Otol Rhinol Laryngol 99:689–694
Khan AM, Shim C, Simmons N, Chung V, Alterman DD, Haramati LB, Berman AR (2006) Tracheobronchopathia osteochondroplastica: a rare cause of tracheal stenosis—“TPO stenosis”. J Thorac Cardiovasc Surg 132:714–716
Secrest PG, Kendig TA, Beland AJ (1964) Tracheobronchopathia osteochondroplastica. Am J Med 36:815–818
Lundgren R, Stjernberg NL (1981) Tracheobronchopathia osteochondroplastica. A clinical bronchoscopic and spirometric study. Chest 80:706–709
Lazor R, Cordier JF (2004) Tracheobronchopathia osteochondroplastica. Orphanet encyclopedia. Available at http://www.orpha.net/data/patho/GB/UK-TO.pdf. Accessed 22 Aug 2008
Simsek PO, Ozcelik U, Demirkazik F, Unal OF, Orhan D, Aslan AT, Dogru D (2006) Tracheobronchopathia osteochondroplastica in a 9-year-old girl. Pediatr Pulmonol 41:95–97
Paaske PB, Tang E (1985) Tracheopathia osteoplastica in the larynx. J Laryngol Otol 99:305–310
Zack JR, Rozenshtein A (2002) Tracheobronchopathia osteochondroplastica: report of three cases. J Comput Assist Tomogr 26:33–36
White BD, Kong A, Khoo E, Southcott AM (2005) Computed tomography diagnosis of tracheobronchopathia osteochondroplastica. Australas Radiol 49:319–321
Marom EM, Goodman PC, McAdams HP (2001) Diffuse abnormalities of the trachea and main bronchi. AJR Am J Roentgenol 176:713–717
Lloyd DC, Taylor PM (1990) Calcification of the intrathoracic trachea demonstrated by computed tomography. Br J Radiol 63:31–32
van Nierop MA, Wagenaar SS, van den Bosch JM, Westermann CJ (1983) Tracheobronchopathia osteochondroplastica. Report of four cases. Eur J Respir Dis 64:129–133
Prakash UB (2001) What is Tracheo(broncho)pathia Osteo(chondro)plastica? J Bronchol 8:75–77
Bioque JC, Feu N, Rubio JM, Martin MA, Garcia FL, Bravo JM, Bravo F, Alvarez A, Villar C, Munoz L (2001) Tracheobronchopathia osteochondroplastica: clinical study and follow-up in nine cases. J Bronchol 8:78–83
Perez-Rodriguez E, Nunez N, Alvarado C, Golpe A, Casanova C, Zapatero J, Fogué L (1990) Diagnosis of tracheopathia osteochondroplastica. Chest 97:763
Sakula A (1968) Tracheobronchopathia osteoplastica: its relationship to primary tracheobronchial amyloidosis. Thorax 23:105–110
Aschoff L (1910) Uber tracheopathia osteoplastica. Verch Dtsch Path Ges 14:125–127
Dalgaard JB (1947) Tracheopathia osteoplastica. Acta Pathol Microbiol Scand 24:118–134
Tajima K, Yamakawa M, Katagiri T, Sasaki H (1997) Immunohistochemical detection of bone morphogenetic protein-2 and transforming growth factor beta-1 in tracheopathia osteochondroplastica. Virchows Arch 431:359–363
Way SP (1967) Tracheopathia osteoplastica. J Clin Pathol 20:814–820
Rose Y, Roucou Y, Roujeau J, Fromentin JC (1974) Metaplasie ossifiante de la muqueuse tracheo-bronchique et ozene. Rev Fr Mal Respir 2:637–645
Jones AW, Chatterji AN (1977) Primary tracheobronchial amyloidosis with tracheobronchopathia osteoplastica. Br J Dis Chest 71:268–272
Alroy GG, Lichtig C, Kaftori JK (1972) Tracheobronchopathia osteoplastica: end stage of primary lung amyloidosis? Chest 61:465–468
Jepsen O, Sorensen H (1960) Tracheopathia osteoplastica and ozaena. Acta Otolaryngol 51:79–83
Gleich LL, Rebeiz EE, Pankratov MM, Shapshay SM (1995) The holmium: YAG laser-assisted otolaryngologic procedures. Arch Otolaryngol Head Neck Surg 121:1162–1166
Grillo HC, Wright CD (2005) Airway obstruction owing to tracheopathia osteoplastica: treatment by linear tracheoplasty. Ann Thorac Surg 79:1676–1681
Kutlu CA, Yeginsu A, Ozalp T, Baran R (2002) Modified slide tracheoplasty for the management of tracheobroncopathia osteochondroplastica. Eur J Cardiothorac Surg 21:140–142
Clerf LH (1944) Tracheopathia osteoplastica. Ann Otol Rhinol Laryngol 53:839–844
Howland WJ Jr, Good CA (1958) The radiographic features of tracheopathia osteoplastica. Radiology 71:847–850
Miyazawa T, Miyazu Y, Iwamoto Y, Ishida A, Kanoh K, Sumiyoshi H, Doi M, Kurimoto N (2004) Stenting at the flow-limiting segment in tracheobronchial stenosis due to lung cancer. Am J Respir Crit Care Med 169:1096–1102
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Abu-Hijleh, M., Lee, D. & Braman, S.S. Tracheobronchopathia Osteochondroplastica: A Rare Large Airway Disorder. Lung 186, 353–359 (2008). https://doi.org/10.1007/s00408-008-9113-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-008-9113-7