Abstract
Objective
The aim of this analysis was to evaluate the prognostic significance of inflammatory biomarkers (NLR, dNLR, PLR and LMR) in NPC patients.
Methods
This was a retrospective analysis of 111 NPC patients from January 2013 and December 2016. Receiver-operating characteristic (ROC) curve was plotted to determine the cut-off values of these inflammatory biomarkers. Univariate analysis and multivariate Cox regression model were used to evaluate the association between these parameters and progression-free survival (PFS) and overall survival (OS).
Results
The optimal critical value of NLR was 2.02, by which cases were divided into high NLR group (NLR ≥ 2.02) and low NLR group (NLR < 2.02). The elevated NLR was significantly associated with decreased OS (P = 0.009) and remained significant in multivariate analysis (HR 8.48, 95% CI 1.69–42.46, P = 0.009).
Conclusions
The before treatment NLR may be an independent prognostic biomarker for OS in patients with NPC. NLR, dNLR and PLR might be a useful complement to TNM staging in the prognosis evaluation of NPC patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nasopharyngeal carcinoma (NPC) is one of the most common head and neck cancers in Southern China with unique ethnic and geographic distributions [1, 2]. Patients with undifferentiated NPC accounts for 90% of cases in endemic regions [3]. Radiotherapy is the primary care for early-stage disease, while concurrent chemoradiotherapy is the standard treatment for advanced NPC [4]. Like other solid tumors, the prognosis of NPC mainly depends on TNM staging system [5]. Although the TNM stage is a very important and widely accepted as a predictor for prognosis, which currently possess some limitations as it does not reflect tumor heterogeneity. Patients with the same TNM and receiving similar treatment strategies exhibit different clinical behaviors and outcomes [6]. Therefore, we need to find out a new way to complement NPC prognosis.
Previous data had shown that inflammation plays a critical role in the metastasis and progression of cancer by facilitating angiogenesis and inhibiting apoptosis [7].Some inflammatory biomarkers, such as NLR (neutrophil-to-lymphocyte ratio), dNLR (derived neutrophil-to-lymphocyte ratio), PLR (platelet-to-lymphocyte ratio), LMR (lymphocyte-to-monocyte ratio), have been found to be related to the prognosis of various cancers, such as laryngeal carcinoma, colorectal cancer, non-small cell lung cancer, gastric cancer [8,9,10,11]. The elevated systemic inflammation response is associated with a poor survival [12]. However, few studies regarding these biomarkers in patients with NPC are available. Therefore, the aim of this analysis was to investigate the prognostic role of the inflammatory biomarkers (NLR, dNLR, PLR and LMR) in NPC.
Materials and methods
Patients
All patients were diagnosed with NPC between January 2013 and December 2016 at our hospital. The patients with early-stage (T1–2N0) diseases were treated with radiotherapy only. The cases with advanced-stage disease were treated with concurrent chemoradiotherapy. Inclusion criteria were as follows: (1) histologically confirmed with NPC; (2) pathological type with low differentiation squamous cancer; (3) complete clinical information and laboratory data; (4) no history of other malignancy; (5) no infection or inflammatory condition. Exclusion criteria were as follows: (1) invalid or incomplete clinical data; (2) unwilling attend to follow-up or lost contact during research period; (3) previously treated in an external hospital; (4) active concomitant infection and acute attack of chronic inflammatory disease. The diagnosis of NPC was made depended on histological evidence and clinical stage according to the 8th edition of the American Joint Committee on Cancer (AJCC) staging system. All clinicopathological data utilized in the present study were retrospectively obtained from each patient’s medical records. Written consent was obtained in all the participants.
Follow-up
Each patient received regular follow-up regularly until June 2020 or until death (every 3 months for the first 2 years, every 6 months in years 3–5 and annually thereafter). Follow-up visit included clinical examination, radiological assessment and electronic nasopharyngoscope. The time of progression-free survival (PFS) and overall survival (OS) were calculated from date of histological diagnosis to the date of disease progressed, death or last follow-up respectively, whichever came first. The median follow-up time was 59 months.
Blood samples
The before treatment blood samples were obtained before first treatment, and which were blinded to the clinical materials. The blood samples are routine examinations before treatment. The NLR, dNLR, PLR and LMR were constructed as follows: NLR = neutrophils count to lymphocytes count, dNLR = neutrophils count to (white cell count—neutrophils count), PLR = platelet count to lymphocytes count, and LMR = platelet count to monocyte count. Patients without information on blood samples and patients with baseline leukocyte counts > 10 × 10^9/L were excluded, as this might portend infection or hematologic conditions.
Statistical analysis
Statistical analysis was carried out by SPSS 23.0 (IBM SPSS, Chicago, IL, USA). Receiver-operating curve (ROC) analysis was applied to determine the area under the curve (AUC) and ideal cut-off values of NLR, dNLR, PLR and LMR. Survival curves were performed by Kaplan–Meier survival analysis. The significance of each clinicopathological parameter (age, gender, disease stage) and inflammatory response index (NLR, dNLR and PLR) with PFS and OS were analyzed using the log-rank test. Multivariate Cox regression model was performed to determine the effect of variables achieving significant level of P < 0.05. Ninety-five percent confidence intervals (95% CI) of hazard risk (HR) were used as common measures to assess relative risk. P < 0.05 was considered to indicate a statistically significant difference.
Results
Association of clinicopathological characteristics with PFS and OS in patients with NPC
A total of 111 patients were eligible for this analysis. Clinicopathological characteristics are presented in Table 1. Briefly, the cohort included 77 male and 34 female patients with a median age of 63 years (range 12–74 years). The demographic form of patients' characteristics is shown in Fig. 1. The median PFS and OS times were 44 months (range 3–90 months) and 53 months (range 5–90 months), respectively. Of the 111 patients, 59 (53.15%) developed tumor progression and 50 (45.05%) died within the follow-up period. The 1-year, 3-year and 5-year overall survival rate were 92.79%, 82.88% and 57.5% for the whole cohort, respectively. We found a significant correlation between age and PFS (P = 0.025). Meanwhile, age, gender and distant metastasis or not also found to significantly affected the OS time (P = 0.012, P = 0.045 and P = 0.034, respectively).
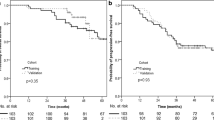
The optimal cut-off values for NLR, dNLR and PLR
The ROC curves, using death as an end-point for NLR, dNLR and PLR are shown in Fig. 2. The areas under curve (AUC) for NLR, dNLR, PLR and LMR were 0.647, 0.635, 0.570 and 0.415 respectively. Because of AUC of LMR less than 0.5, we do not think LMR has application value. The ideal cut-off values based on OS were 2.02 for NLR (86.0% sensitivity and 44.3% specificity), 1.60 for dNLR (82.0% sensitivity and 42.6% specificity) and 266.65 for PLR (72.0% sensitivity and 88.5% specificity) by ROC curve analysis. Patients were divided into two groups based on the ideal cut-off values, with a high group ≥ the optimal cut-off values and a low group < the optimal cut-off values. The association of two groups with OS in patients with NPC is presented in Table 2. The mortality in the low group of NLR was 20.6% and in the high group of NLR was 55.8% (P = 0.009, Fig. 3). The mortality in the low group of dNLR was 25.7% and in the high group of dNLR was 53.9% (P = 0.035, Fig. 3). The mortality in the low group of PLR was 40.0% and in the high group of NLR was 66.7% (P = 0.047, Fig. 3).
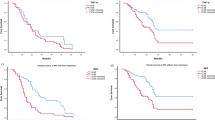
Likewise, using the progression of disease as end-point for NLR, dNLR and PLR, the ROC curves are shown in Fig. 4. The areas under curve (AUC) for NLR, dNLR, and PLR were 0.627, 0.623, and 0.573 respectively. The ideal cut-off values based on PFS were 2.02 for NLR (81.4% sensitivity and 44.2% specificity), 1.34 for dNLR (91.5% sensitivity and 30.8% specificity) and 151.89 for PLR (55.9% sensitivity and 59.6% specificity) by ROC curve analysis. The tumor progressed in 11 (32.4%) out of 34 patients with NLR < 2.02 and in 48 (62.3%) out of 77 patients with NLR ≥ 2.02 (P = 0.013, Fig. 5), 5 (23.8%) out of 21 patients with dNLR < 1.34 and in 54 (60%) out of 90 patients with dNLR ≥ 1.34 (P = 0.013, Fig. 5), and 25 (44.6%) out of 56 patients with PLR < 151.89 and in 34 (61.8%) out of 55 patients with PLR ≥ 151.89 (P = 0.132, Fig. 5), respectively. In the present study, the NLR and dNLR were associated with PFS, whereas PLR was not associated with PFS (Table3).
According to multivariate analysis, age, gender, distant metastasis or not and NLR were independent prognostic factors for OS (P = 0.025, P = 0.012 P = 0.007 and P = 0.009, respectively; Table 4). It was showed that high NLR, high age, male and distant metastasis were associated with worse OS. On univariate analyses, high age was associated with worse PFS (P = 0.025, Table5).
Discussion
Currently, studies have shown that the invasion ability of malignant tumors is not only related to the essential characteristics of tumor cells, but also depends on the inflammatory microenvironment. The specific mechanism may be as follows: inflammatory mediators and cytokines secreted by inflammatory cells can stimulate the body to produce a series of stress responses, leading to excessive accumulation of inflammatory cells, resulting in negative biological effects of cell oxidative damage, and affecting the body's microenvironment, which eventually leads to the transformation of normal cells to tumor cells, and enhances the ability of tumor growth, invasion and metastasis [13, 14]. The inflammatory microenvironment is mainly composed of inflammatory cells, and neutrophils, lymphocytes, platelets and monocytes in the peripheral blood are easily obtained.
Neutrophils are generally considered to have antibacterial functions. However, more and more studies have proved that tumor-associated neutrophils (TAN) play an important role in cancer biology. TAN can be divided into N1 (anti-tumor type) and N2 (tumor-promoting type) according to different activation pathways [15]. TAN is of N2 type in the presence of transforming growth factor β(TGF-β). N2TAN can secrete angiogenic factors, chemokines, cytokines and reactive oxygen species, which promote tumor development. Lymphocytes are an important cell component of the body's immune response process. During the malignant growth of tumors, its main function is to inhibit the development of tumors through immune surveillance. Ts cells and NK cells induce cancer cell apoptosis and inhibit tumor growth by secreting interferon-γ (IFN-γ) [16, 17]. Th17 cells secrete a high level of cytokines, including IFN-γ, and tumor necrosis factor (TNF), which mediate the antitumor effects [18]. Platelets store various angiogenesis regulators, such as VEGF, platelet-derived growth factor, and fibroblast growth factor. Most of these angiogenesis regulators have been proved to be direct or indirectly participate in the angiogenesis of tumor cell growth. Hyperplatelet is considered to be an important factor affecting the prognosis of cancer patients. Tumor-associated macrophages (TAM) exist in the tumor microenvironment, which can promote angiogenesis and immunosuppression, enhance tumor progression and growth [19].
NLR, dNLR, PLR and LMR as the ratio of absolute counts between two types of inflammatory cells.
Jin et al. found that NLR before treatment is considered to be an independent predictor of survival in patients with metastatic nasopharyngeal carcinoma [20]. In this study, elevated NLR was significantly associated with poor PFS and OS of the NPC patients. In addition, NLR was the independent prognostic factor for OS of NPC patients. The result was consistent with the finding of existing research [21, 22]. Moreover, we found that the dNLR was significantly associated with poor PFS and OS of the NPC patients, which were rarely found in other studies. This was our new discovery. The relatively high PLR was associated with poor OS of the NPC patients. However, PLR was not the independent prognostic factor in this study. The result was consistent with the finding of Lu et al. [23]. There was no significant correlation between LMR level and prognosis in NPC patients. At present, there are very few studies on the prognosis of NPC patients with before treatment LMR. This study has some limitations. First, this paper is based on a single-center retrospective research with only a small number of patients enrolled. For the furthermore endeavor, we would conduct a multi-center large-scale prospective research to further verify the correlations between inflammation and the prognosis of NPC patients. Second, from clinical judgment, there are many pathological types of nasopharyngeal carcinoma. This paper only focused on the most popular pathological type—low differentiation squamous cancer, which led to a limitation in the number of patients enrolled. In the future, we will expand more pathological types and explore the correlations between different pathological types and prognosis of NPC patients. Finally, we did not collect blood samples from patients after treatment, which made it very hard to observe the changes on inflammatory indicators of all the NPC patients after treatment. Therefore, in future series of researches, we will pay attention to the dynamic changes of inflammatory indicators in relevant patients between before treatment and post-treatment, so as to further clarify the relationship between inflammatory response indicators and the prognosis of patients with nasopharyngeal carcinoma.
In summary, NLR, dNLR and PLR, as indicators of systemic inflammatory response, have certain significance in the prognostic evaluation of patients with nasopharyngeal carcinoma. At the same time, due to easy access, low cost, and easy acceptance by patients, the inflammatory indicators may be useful complements to the prognosis evaluation of NPC patients.
Conclusion
In the current study, we found that the before treatment NLR was independent prognostic factor for OS in NPC patients. The elevated NLR, dNLR and PLR were linked to poor prognosis in NPC patient. NLR, dNLR and PLR might be a useful complement to TNM staging in the prognosis evaluation of NPC patients. At present, it is still necessary to find the best cut-off value of the inflammatory response indicators for evaluating the prognosis of NPC patients in my country through domestic multi-center and large-sample research, and to clarify its diagnosis, curative effect evaluation and prognosis judgment for NPC patients through prospective studies.
References
Wei KR, Zheng RS, Zhang SW et al (2017) Nasopharyngeal carcinoma incidence and mortality in China, 2013. Chin J Cancer. https://doi.org/10.1186/s40880-017-0257-9
Poh SS, Chua MLK, Wee JTS (2016) Carcinogenesis of nasopharyngeal carcinoma: an alternate hypothetical mechanism. Chin J Cancer 35:9
Wee J (2012) Nasopharyngeal cancer: a promising future. Lancet Oncology 13(2):116–118
Blanchard P, Lee A, Marguet S et al (2015) Chemotherapy and radiotherapy in nasopharyngeal carcinoma: an update of the MAC-NPC meta-analysis. Lancet Oncol 16(6):645–655
Rui S, Hui-Zhi Q, Hai-Qiang M et al (2013) Prognostic value and differences of the sixth and seventh editions of the UICC/AJCC staging systems in nasopharyngeal carcinoma. J Cancer Res Clin Oncol 139(2):307–314
Au JSK, Law CK, Foo W et al (2003) In-depth evaluation of the AJCC/UICC 1997 staging system of nasopharyngeal carcinoma: Prognostic homogeneity and proposed refinements. Int J Radiat Oncol Biol Phys 56(2):413–426
Grivennikov SI, Greten FR, Karin M (2010) Immunity, Inflammation, and Cancer. Cell 140(6):883–899
Song S, Chen H, Dong W et al (2019) The prognostic value of preoperative derived neutrophil-to-lymphocyte ratio in patients undergoing total laryngectomy with laryngeal carcinoma. Acta Oto Laryngologica 139(3):294–298
Azab B, Mohammad F et al (2014) The value of the before treatment neutrophil lymphocyte ratio vs. platelet lymphocyte ratio in predicting the long-term survival in colorectal cancer. CBM. https://doi.org/10.3233/CBM-140416
Lin GN, Peng JW, Xiao JJ et al (2014) Prognostic impact of circulating monocytes and lymphocyte-to-monocyte ratio on previously untreated metastatic non-small cell lung cancer patients receiving platinum-based doublet. Med Oncol 31(7):1–6
Jiang N, Deng JY, Liu Y et al (2014) The role of preoperative neutrophil–lymphocyte and platelet–lymphocyte ratio in patients after radical resection for gastric cancer. Biomarkers 19(6):444–451
Roxburgh CSD, Mcmillan DC (2014) Cancer and systemic inflammation: treat the tumour and treat the host. Br J Cancer 110(6):1409–1412
Azab B, Bhatt VR, Phookan J, Murukutla S et al (2012) Usefulness of the neutrophil-to-lymphocyte ratio in predicting short-and long-term mortality in breast patients. Ann Surg Oncol 19(1):217–224
Pichler M, Stoeckigt C, Chromecki TF et al (2013) Validation of the before treatment neutrophil-lymphocyte ratio as prognostic factor regarding cancer-specific, metastasis-free, and overall survival in a European cohort of patients with renal cell carcinoma. JCO 31(6_suppl):410
Fridlender ZG, Sun J, Kim S et al (2009) Polarization of tumor-associated neutrophil phenotype by TGF-beta: “N1” versus “N2” TAN. Cancer Cell 16(3):183–194
Smith HA, Kang Y (2013) The metastasis-promoting roles of tumor-associated immune cells. J Mol Med 91(4):411–429
Dunn GP, Old LJ, Schreiber RD (2004) The three Es of cancer immunoediting. Annu Rev Immunol 22(22):329–360
Kryczek I, Banerjee M, Cheng P et al (2009) Phenotype, distribution, generation, and functional and clinical relevance of Th17 cells in the human tumor environments. Blood 114(6):1141–1149
Varki A (2007) Trousseau’s syndrome: multiple definitions and multiple mechanisms. Blood 110:1723–1729
Jin Y, Ye X, He C, Zhang B, Zhang Y (2015) before treatment neutrophil-to-lymphocyte ratio as predictor of survival for patients with metastatic nasopharyngeal carcinoma. Head Neck 37(1):69–75
An X, Ding PR, Wang FH, Jiang WQ, Li YH (2011) Elevated neutrophil to lymphocyte ratio predicts poor prognosis in nasopharyngeal carcinoma. Tumour Biol 32(2):317–324
Takenaka Y, Kitamura T, Oya R et al (2017) Prognostic role of neutrophil–lymphocyte ratio in nasopharyngeal carcinoma: a meta-analysis. PLoS ONE 12(7):e0181478
Lu A, Li H, Zheng Y et al (2017) Prognostic significance of neutrophil to lymphocyte ratio, lymphocyte to monocyte ratio, and platelet to lymphocyte ratio in patients with nasopharyngeal carcinoma. Biomed Res Int 2017:3047802
Funding
This study was supported by the National Natural Science Foundation of China (Nos. 81670928), Nanjing Medical Science and technique Development Foundation (QRX17051), and the Project of Invigorating Health Care through Science, Technology and Education (ZDXKB2016015).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Not applicable.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Song, S., Chen, H., Dou, X. et al. The prognostic value of before treatment neutrophil-to-lymphocyte ratio in nasopharyngeal carcinoma. Eur Arch Otorhinolaryngol 279, 2485–2492 (2022). https://doi.org/10.1007/s00405-021-07070-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-07070-3