Abstract
Elevated neutrophil to lymphocyte ratio (NLR) has been reported to be associated with worse survival in many malignancies, whereas its role in nasopharyngeal carcinoma (NPC) remains unclear. We retrospectively reviewed 363 consecutively, newly diagnosed, non-disseminated, and biopsy-proven NPC patients. Disease-specific survival (DSS), distant metastasis-free survival (DMFS), and locoregional recurrence-free survival (LRFS) rates were compared according to NLR level. Multivariate analysis was performed to assess the prognostic value of NLR. The 5-year DSS, DMFS, and LRFS rates for patients with elevated or non-elevated NLR (> or ≤3.73) were 59.6% vs. 76.6% (p = 0.03), 69.7% vs. 86.6% (p = 0.002), and 78.5% vs. 87.3% (p = 0.105), respectively. For patients with locoregionally advanced disease, NLR was not only an independent prognostic factor, but also a predictor of response to chemoradiotherapy. The 5-year DSS, DMFS, and LRFS rates for patients with elevated or non-elevated NLR were 47.2% vs. 73.7% (p < 0.001), 59.2% vs. 85.1% (p < 0.001), and 72.3% vs. 84.6% (p = 0.041), respectively. Compared with radiation alone, chemoradiotherapy significantly improved DSS and LRFS for patients with non-elevated NLR, but not for those with elevated NLR. Pre-treatment NLR is a strong prognostic factor for NPC patients. For patients with locoregionally advanced disease, NLR might also be a useful indicator for selection of treatment strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nasopharyngeal carcinoma (NPC) is one of the most common malignancies in southern China, especially in the region of Guangdong Province, where the incidence is 30 to 80 of 100,000 people per year [1]. Although NPC is sensitive to radiotherapy (RT), the long-term survival remains poor due to high incidence of distant metastasis and (or) local recurrences. Currently, the prognosis for NPC patients mainly relies on clinical staging. However, patients with the same clinical stage often present different clinical outcomes, indicating that the clinical staging is insufficient for precisely predicting prognosis of NPC. Various prognostic factors for NPC have been identified and evaluated retrospectively, most of these factors were identified by immunohistochemical staining of tumor tissue, such as apoptosis-related protein survivin and livin [2], angiogenetic factor vascular endothelial growth factor [3], and so on. However, few of these markers are currently in clinical application. It is therefore critical to explore valuable factors to predict outcome for NPC patients.
Recent studies have shown that systemic inflammatory response could promote tumor metastasis and progression by inhibition of apoptosis, promotion of angiogenesis, and damage of DNA [4]. Neutrophil to lymphocyte ratio (NLR), one of the inflammatory marker, has been shown to be associated with progression and metastasis of many kinds of malignancies, including colorectal cancer [5–7], gastric cancer [8], non-small cell lung cancer [9], ovarian cancer [10], intrahepatic cholangiocarcinoma [11], hepatocellular carcinoma [12, 13], and pancreatic cancer [14]. However, there is no report about the possible role of NLR in NPC patients. We therefore conducted this retrospective study to investigate whether NLR could serve as a prognostic factor in NPC patients.
Material and methods
Study population
A total of 381 consecutive newly diagnosed, histologically proven, and non- disseminated NPC patients were hospitalized and treated at the Sun Yat-sen University Cancer Center (Guangzhou, China) between November 2001 and July 2002. Of these patients, 18 were subsequently eliminated from the study, including ten patients who presented recurrence disease and had received RT therapy before, five patients who had residual disease after RT, and three patients who developed metastasis during the treatment. Thus, 363 patients were included in the analysis. There were 274 (75.5%) male patients and 89 (24.5%) female patients. The median age was 47 years (range, 12–76 years). The routine workup was done before the initiation of treatment, which included a complete physical examination, hematologic and biochemistry profiles, endoscopic examination of the nasopharynx, computed tomography (CT) or magnetic resonance imaging (MRI) scan of the nasopharynx and neck, chest plain film or CT scan, and abdominal sonography or CT scan. According to the 1997 AJCC staging system [15], 14 patients (3.9%) were classified as stage I, 81 patients (22.3%) as stage II, 165 patients (45.4%) as stage III, and 103 patients (28.4%) as stage IVA (M0) disease. Informed consent has been obtained, and procedures followed were in accordance with the institutional ethical standards of the responsible committee on human experimentation.
The NLR was calculated from the differential count by dividing the absolute neutrophil count by the absolute lymphocyte count. All patients had no coexistent hematologic disorders or known active infection before treatment, ensuring that the white cell count was representative of normal baseline value.
Treatment and follow-up
All patients were treated with standard curative RT with or without chemotherapy. The median radiation dose was 70 Gy (range, 60–80 Gy) to the nasopharyngeal region and 60 Gy (range, 40–72 Gy) to the initially involved cervical node. For 268 locoregionally advanced stage III and IVA patients, 133 patients (49.6%) were treated with RT alone and 135 (50.4%) patients were treated with cisplatin and/or 5-FU-based neoadjuvant (28 patients) and/or concurrent chemotherapy (107 patients). Thirty-three (24.4%) patients received one cycle of chemotherapy, 88 (65.2%) patients received two cycles of chemotherapy, and 14 (10.4%) patients received three cycles of chemotherapy.
Patients were followed up at least every 3 months during the first 2 years; thereafter, patients were followed up every 5 months until death or until July 2009. The median follow-up period for the whole group was 62 months (range, 2–92 months). The following endpoints were assessed: disease-specific survival (DSS); distant metastasis-free survival (DMFS), and locoregional recurrence-free survival (LRFS). Local recurrence was established by fiberoptic endoscopy and biopsy and/or MRI. Distant metastases were diagnosed based on clinical symptoms, physical examination, and imaging methods including chest plain film or CT scan, bone scan, and abdominal sonography or CT scan. Whenever possible, salvage treatments were given to patients after documented recurrence. The treatment employed included reirradiation, chemotherapy, and surgery.
Statistical analysis
Statistical analysis was performed by using SPSS statistical software (SPSS Inc, Chicago, IL, USA, version 12.0 for Windows). Receiver operating characteristic (ROC) curve analysis was performed to select the most appropriate cut-off point of NLR to stratify patients at a high risk of malignancy-related death. At each value, the sensitivity and specificity was plotted, thus generating an ROC curve. The score closest to the point with both maximum sensitivity and specificity (i.e., the point [0.0, 1.0] on the curve) was selected as the cut-off value. Chi-square tests were used to analyze differences among groups of patients with elevated or non-elevated NLR. The DSS, DMFS, and LRFS rates were calculated by the Kaplan–Meier method, and survivals were compared by using the log-rank test. Multivariate analyses with the Cox proportional hazards model were used to test independent prognostic impact of NLR. P values of less than 0.05 were considered statistically significant.
Results
Recurrence and survival analysis
By July 2009, 49 patients (13.5%) developed locoregional recurrences, 72 patients (19.8%) developed distant metastases, and five patients (1.4%) developed both distant metastases and local–regional recurrences. Overall, the 5-year failure-free survival (FFS) rate was71.6%. The 5-year LRFS and DMFS rates were 87.4% and 82.5%, respectively. One hundred and one patients (27.8%) died of all causes, among which 96 (95.0%) died of recurrence disease. The 5-year DSS rate was 72.2%.
Determinants of NLR status
The mean NLR level was 3.07 ± 1.65 (range, 0.72–11.0). An NLR value of 3.73 resulted in the most appropriate sensitivity of 0.66 and specificity of 0.55 for DSS. Using 3.73 as the cut-off point, we identified 92 patients (25.3%) as elevated NLR. None of the demographic and clinical characteristics, including age, gender, performance status (PS), T stage, N stage, and treatment modality, or serum lactate dehydrogenase (LDH) level was associated with elevated NLR.
NLR predicted survival for NPC patients
Various potential prognostic factors and NLR status were univariately analyzed by the log-rank test (Table 1). T status, N status, and NLR status were predictors of malignancy-related death. N status and NLR status were predictors of distant metastasis. T status and gender were predictors of local disease recurrence. Multivariate analysis showed that NLR status was an independent predictor of both malignancy-related death and distant metastasis. Other independent factors were advanced T and N status (predicted malignancy-related death), advanced N status (predicted distant metastasis) and advanced T status (predicted local disease recurrence) (Table 2).
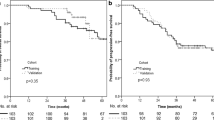
Kaplan–Meier analysis showed that patients with an elevated pre-treatment NLR had a significant shorter DSS and higher distant metastatic rate than those with non-elevated NLR. The 5-year DSS rate was 59.6% in the elevated NLR group and 76.6% in the non-elevated NLR group (p = 0.03). Five-year DMFS rate in the elevated NLR group and low NLR group were 69.7% and 86.6%, respectively (p = 0.002). There was a trend of lower LRFS rate in patients with elevated NLR than in those with non-elevated NLR (78.5% vs. 87.3%, p = 0.105) (Table 1 and Fig. 1).
NLR predicted response to chemoradiotherapy (CRT) for patients with locoregionally advanced stage
For 268 patients who had locoregionally advanced disease (stage III/IVA), 5-year DSS, FFS, DMFS, and LRFS rates were 66.7%, 66.0%, 78.6%, and 81.3%, respectively. Seventy out of 268 patients showed elevated NLR level (>3.73), whereas 198 patients showed non-elevated NLR level (≤3.73). The 5-year DSS, DMFS, and LRFS rates between elevated NLR group and non-elevated NLR groups were 47.2% vs. 73.7% (p < 0.001), 59.2% vs. 85.1% (p < 0.001), and 72.3% vs. 84.6% (p = 0.041), respectively (Fig. 2). For patients treated with RT alone (133 patients), the 5-year DSS rates between elevated NLR group and non-elevated NLR groups were 51.9% vs. 69.1 (p = 0.014), while for patients treated with CRT (135 patients), the 5-year DSS rates between elevated NLR group and non-elevated NLR groups were 46.2% vs. 77.3% (p < 0.001). (Fig. 3)
The efficacy of different treatment modality was also investigated. Among 198 patients with non-elevated NLR, 94 patients were treated by RT alone and 104 patients were treated by CRT. The events of patients dying from disease, developing distant metastasis, and developing local recurrence in RT alone group were 30, 22, and 17 cases, compared to 22, 19, and 14 cases in CRT group, respectively. The 5-year DSS, LRFS, and DMFS rates in RT alone and CRT group were 69.5% vs. 77.3% (p = 0.049), 78.4% vs. 89.8% (p = 0.021), and 84.9% vs. 85.2% (p = 0.588), respectively. Among 70 patients with elevated NLR, 39 patients were treated by RT alone and 31 patients were treated by CRT. The events of patients dying from disease, developing distant metastasis and local recurrence in RT alone group were 18, 16, and eight cases, compared to 17, 11, and eight cases in CRT group, respectively. The 5-year DSS, DMFS, and LRFS rates in the RT alone and CRT group were 51.9% vs. 46.2% (p = 0.691), 56.3% vs. 62.9% (p = 0.474), and 71.8% vs. 69.0% (p = 0.438), respectively. (Fig. 4).
Discussion
In the current study, we demonstrated for the first time that pre-treatment NLR status was a strong prognostic factor for NPC patients. Patients with elevated NLR showed significantly worse DSS and DMFS, compared with patients with non-elevated NLR. Patients with elevated NLR also showed a tendency toward increased locoregional recurrence risk, although the difference was not statistically significant. For patients with locoregionally advanced stage disease in the same treatment modality, NLR remained a significant prognostic factor. On multivariate analysis, after adjusting T classification and N classification, NLR remained an independent prognostic factor for DSS and DMFS.
The association between elevated NLR and poor oncologic outcome is not clearly defined to date. Several possible mechanisms may explain it. First, the host’s immune response to tumor is lymphocyte dependent. Early studies have shown an abundant infiltration of nonmalignant lymphocytes in the primary tumor of NPC [16, 17], which is linked with favorable prognosis [18]. Meanwhile, elevated peripheral blood lymphocyte counts have also been linked with improved survival in breast cancer patients undergoing curative resection, which is attributed to the pivotal role of lymphocytes in cytotoxic cell death and cytokines production that inhibit proliferation and metastatic activity of tumor cells [19]. Second, neutrophils are reported to be the primary source of circulating angiogenesis-regulating chemokines (e.g., CXCL8), growth factors (e.g., vascular endothelial growth factor), and proteases (e.g., tissue inhibitors of metalloproteinase) which are major contributors to tumor related angiogenesis [13, 20, 21]. Therefore, NLR can be considered as the balance between pro-tumor inflammatory status and anti-tumor immune status. Patients with elevated NLR have a relative lymphocytopenia and neutrophilic leukocytosis, which denotes that the balance is tipped in favor of pro-tumor inflammatory and is associated with poor oncologic outcome.
Currently, for patients with locally advanced disease, a number of randomized clinical trials have shown that concurrent chemoradiotherapy (CCRT) either with or without adjuvant chemotherapy could improve both overall and progression free survival [22–24]. However, not all the patients could benefit from CCRT. Lin et al. [25] reported that CCRT was superior to RT alone for low-risk patients but inadequate for high-risk patients according to their risk grouping system. Therefore, it is critical to identify patients who may benefit from more aggressive treatment modalities. According to our study, for patients with non-elevated NLR, CCRT is significantly better than RT alone in terms of OS and LRFS, while for patients with elevated NLR, CCRT failed to show significant survival benefits compared to RT alone. These findings suggest that NLR might be considered to be used as an indicator for decision making in the treatment of locoregionally advanced NPC patients.
NLR is an inexpensive, reproducible, and widely available blood test and adds no additional cost to routine pretreatment workup. This is especially relevant because NPC is endemic to many developing countries in which the healthcare budget is a major constraint. However, the interpretation of our results was hampered by the retrospective nature of the study. Various biases exist in the present study, such as among patient treated with CRT, only 79% of patients received CCRT and 24% of patients received only one cycle of chemotherapy. Therefore, further prospective study is warranted.
In summary, in the current study, we indicate that pre-treatment NLR level is a significant prognostic factor in patients with NPC. Furthermore, pre-treatment NLR level might be a useful indicator for decision making in the management of locoregionally advanced NPC.
References
Muir C, Waterhouse J, Mack T. Cancer incidence in five continents. IARC Sci Publ. 1987;5:1–970.
Xiang Y, Yao H, Wang S, Hong M, He J, Cao S, et al. Prognostic value of survivin and livin in nasopharyngeal carcinoma. Laryngoscope. 2006;116:126–30.
Segawa Y, Oda Y, Yamamoto H, Shiratsuchi H, Hirakawa N, Komune S, et al. Close correlation between CXCR4 and VEGF expression and their prognostic implications in nasopharyngeal carcinoma. Oncol Rep. 2009;21:1197–202.
McMillan DC. Systemic inflammation, nutritional status and survival in patients with cancer. Curr Opin Clin Nutr Metab Care. 2009;12:223–6.
Halazun KJ, Aldoori A, Malik HZ, Al-Mukhtar A, Prasad KR, Toogood GJ, et al. Elevated preoperative neutrophil to lymphocyte ratio predicts survival following hepatic resection for colorectal liver metastases. Eur J Surg Oncol. 2008;34:55–60.
Kishi Y, Kopetz S, Chun YS, Palavecino M, Abdalla EK, Vauthey JN. Blood neutrophil-to-lymphocyte ratio predicts survival in patients with colorectal liver metastases treated with systemic chemotherapy. Ann Surg Oncol. 2009;16:614–22.
Ding PR, An X, Zhang RX, Fang YJ, Li LR, Chen G, Wu XJ, Lu ZH, Lin JZ, Kong LH, Wan DS, Pan ZZ. Elevated preoperative neutrophil to lymphocyte ratio predicts risk of recurrence following curative resection for stage iia colon cancer. Int J Colorectal Dis. 2010 (in press)
Yamanaka T, Matsumoto S, Teramukai S, Ishiwata R, Nagai Y, Fukushima M. The baseline ratio of neutrophils to lymphocytes is associated with patient prognosis in advanced gastric cancer. Oncology. 2007;73:215–20.
Sarraf KM, Belcher E, Raevsky E, Nicholson AG, Goldstraw P, Lim E. Neutrophil/lymphocyte ratio and its association with survival after complete resection in non-small cell lung cancer. J Thorac Cardiovasc Surg. 2009;137:425–8.
Cho H, Hur HW, Kim SW, Kim SH, Kim JH, Kim YT, et al. Pre-treatment neutrophil to lymphocyte ratio is elevated in epithelial ovarian cancer and predicts survival after treatment. Cancer Immunol Immunother. 2009;58:15–23.
Gomez D, Morris-Stiff G, Toogood GJ, Lodge JP, Prasad KR. Impact of systemic inflammation on outcome following resection for intrahepatic cholangiocarcinoma. J Surg Oncol. 2008;97:513–8.
Gomez D, Farid S, Malik HZ, Young AL, Toogood GJ, Lodge JP, et al. Preoperative neutrophil-to-lymphocyte ratio as a prognostic predictor after curative resection for hepatocellular carcinoma. World J Surg. 2008;32:1757–62.
Halazun KJ, Hardy MA, Rana AA, Woodland DCT, Luyten EJ, Mahadev S, et al. Negative impact of neutrophil-lymphocyte ratio on outcome after liver transplantation for hepatocellular carcinoma. Ann Surg. 2009;250:141–51.
An X, Ding PR, Li YH, Wang FH, Shi YX, Wang ZQ, et al. Elevated neutrophil to lymphocyte ratio predicts survival in advanced pancreatic cancer. Biomarkers. 2010;15:516–22.
American Joint Committee on Cancer. Manual for staging of cancer. 5th ed. Philadelphia: Lippincott; 1997.
Ferradini L, Miescher S, Stoeck M, Busson P, Barras C, Cerf-Bensussan N, et al. Cytotoxic potential despite impaired activation pathways in t lymphocytes infiltrating nasopharyngeal carcinoma. Int J Cancer. 1991;47:362–70.
Hang ZB, Wei YQ, Wang YP, Xu NR. Direct ultrastructural evidence of lymphocyte-mediated cancer cell lysis in the microenvironment of Chinese nasopharyngeal carcinoma. Hum Pathol. 1991;22:320–5.
Kojya S, Itokazu T, Noda Y, Ezaki M, Tomita Y, Ohsawa M, et al. Site-specific localization of Epstein-Barr virus in pharyngeal carcinomas. Jpn J Cancer Res. 1998;89:510–5.
Ownby HE, Roi LD, Isenberg RR, Brennan MJ. Peripheral lymphocyte and eosinophil counts as indicators of prognosis in primary breast cancer. Cancer. 1983;52:126–30.
Tanigawa N, Amaya H, Matsumura M, Shimomatsuya T. Correlation between expression of vascular endothelial growth factor and tumor vascularity, and patient outcome in human gastric carcinoma. J Clin Oncol. 1997;15:826–32.
Kusumanto YH, Dam WA, Hospers GA, Meijer C, Mulder NH. Platelets and granulocytes, in particular the neutrophils, form important compartments for circulating vascular endothelial growth factor. Angiogenesis. 2003;6:283–7.
Lin JC, Jan JS, Hsu CY, Liang WM, Jiang RS, Wang WY. Phase III study of concurrent chemoradiotherapy versus radiotherapy alone for advanced nasopharyngeal carcinoma: positive effect on overall and progression-free survival. J Clin Oncol. 2003;21:631–7.
Kwong DL, Sham JS, Au GK, Chua DT, Kwong PW, Cheng AC, et al. Concurrent and adjuvant chemotherapy for nasopharyngeal carcinoma: a factorial study. J Clin Oncol. 2004;22:2643–53.
Al-Sarraf M, LeBlanc M, Giri PG, Fu KK, Cooper J, Vuong T, et al. Chemoradiotherapy versus radiotherapy in patients with advanced nasopharyngeal cancer: phase III randomized intergroup study 0099. J Clin Oncol. 1998;16:1310–7.
Lin JC, Liang WM, Jan JS, Jiang RS, Lin AC. Another way to estimate outcome of advanced nasopharyngeal carcinoma—is concurrent chemoradiotherapy adequate? Int J Radiat Oncol Biol Phys. 2004;60:156–64.
Authors’ disclosures of potential conflicts of interest
The authors report no declarations of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Xin An and Pei-Rong Ding contributed equally to this work.
Rights and permissions
About this article
Cite this article
An, X., Ding, PR., Wang, FH. et al. Elevated neutrophil to lymphocyte ratio predicts poor prognosis in nasopharyngeal carcinoma. Tumor Biol. 32, 317–324 (2011). https://doi.org/10.1007/s13277-010-0124-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-010-0124-7