Abstract
Background
Cochlear nerve deficiency is one of the known causes of congenital sensorineural hearing loss. Management of hearing loss in children with cochlear nerve deficiency poses a multidimensional challenge. The absent or hypoplastic cochlear nerve may prevent electrical stimulation from reaching the brainstem and the auditory cortex. A deficient cochlear nerve can be associated with other inner ear malformations, which may diminish the success of cochlear implantation in those children. Promising results in adults after auditory brainstem implantation led to the expansion of candidacy to include the pediatric populations who were contraindicated for CIs.
Objective
To review the outcomes of cochlear implantation versus that of auditory brainstem implantation in children with various conditions of the auditory nerve.
Methods
This retrospective chart review study comprised two pediatric groups. The first group consisted of seven ABI recipients with cochlear nerve aplasia and the second group consisted of another seven children with cochlear nerve deficiencies who underwent CI surgery. The participants’ auditory skills and speech outcomes were assessed using different tests selected from the Evaluation of Auditory Responses to Speech (EARS) test battery.
Results
There were some individual variations in outcomes depending on the status of the auditory nerve. The mean CAP score of the ABI group was 2.87, while the mean SIR score was 0.62. On the other hand, the mean CAP score of the CI group was 1.29, while the mean SIR score was 0.42.
Conclusion
Our results are in good agreement with the reported auditory perception and speech and language development outcomes of pediatric auditory brainstem implantation. We added to the growing body of literature on the importance of verifying and identifying the status of the cochlear nerve in the decision-making process of the surgical management of those pediatric groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The cochlear implant (CI) is a very effective form of hearing rehabilitation for congenital or acquired severe-to-profound sensorineural hearing loss (SNHL). In both adult and pediatric populations with congenital or acquired SNHL, there are subset populations for whom a CI would be have very limited or no benefit. These subset populations are usually contraindicated for a CI, because the anatomy or state of health of the cochlea renders it unsuitable for implantation and/or because cochlear nerve deficiencies, such as nerve aplasia or nerve hypoplasia, could be identified using MRI [1]. The cochlear nerve is considered aplastic if it could not be verified on axial, coronal, or oblique sagittal imaging, and is considered hypoplastic if its size appeared small compared to the other nerves of the internal auditory canal (IAC) [2]. In those cases, the auditory brainstem implant (ABI) may be the last option to restore the hearing pathway.
The auditory brainstem implant (ABI) was developed for adults with SNHL due to neurofibromatosis type 2 (NF2). By now, ABI candidacy for adults includes inner ear malformation, inner ear ossification, temporal bone fracture with cochlear nerve avulsion, otosclerosis with gross cochlear destruction, and cochlear nerves that were severed during surgical procedures [3]. Promising results in non-NF2 adult ABI users led to the expansion of candidacy to include the pediatric populations who were contraindicated for CIs. Merkus et al. [4] conducted a systematic review of literature on the indications and contraindications in non-NF2 adult and pediatric cases. A total of 144 cases were reviewed. The authors recommended that diagnostic imaging and auditory testing should be geared toward cochlear implantation; if an intact cochlear nerve and an open cochlea on at least one side can be verified, the strong recommendation was made to attempt cochlear instead of auditory brainstem implantation. Bilateral absent cochlear nerve fibers, bilateral complete cochlear aplasia, and bilateral Michel deformity were the only indications for which the authors felt an ABI was the only solution.
Noij et al. [5] reviewed 21 publications that featured a total of 162 non-NF2 pediatric ABI users. Some of the publications concluded that ABIs supported the development of oral language. However, auditory outcomes were observed to vary considerably between individual users and were more variable compared to the outcomes seen in their CI user peers, when matched for the same demographic factors. Bayazit et al. [3] observed that the development of oral language in pediatric ABI users depended on several factors: for instance, age at implantation, the presence or absence of additional disabilities, and parents’ expectations during the rehabilitation process.
The study by Wu et al. [6] featured a large population of 656 children with SNHL who underwent cochlear implantation and MRI at their center. Children who received their CI on the side with auditory nerve hypoplasia were more likely to perform better than children who received their CI on the side with auditory nerve aplasia. In addition, the children with auditory nerve hypoplasia produced CAP (Categories of Auditory Performance) and SIR (Speech Intelligibility Rating) scores that did not differ significantly from the children’s scores who had no nerve deficiency. Teagle et al. [7] and Rajeswaran et al. [8] emphasized that significant auditory and communication developmental trends could be identified in pediatric ABI users, but these developmental trends occurred at slower rates than those of their CI peers.
The primary objective of the current study was to review the auditory perception outcome, and speech and language outcomes of cochlear implantation versus those of auditory brainstem implantation in children with various conditions of the auditory nerve. A secondary objective was to contribute to the pool of literature that discusses selection criteria and factors that affect the decision-making process between cochlear and auditory brainstem implantation in pediatric populations with auditory nerve deficiencies.
Materials and methods
Study design
This retrospective chart review considered two pediatric groups. The first group consisted of seven children with cochlear nerve aplasia who had undergone ABI surgery and the second group consisted of seven children with cochlear nerve deficiencies who underwent CI surgery. All children were required to meet the following criteria: a prelingual onset of deafness; severe-to-profound SNHL; use of a hearing aid for 3–6 months before implantation; a minimum of 2 years of CI use (control group) or ABI use (study group); rehabilitation for at least 1 year with auditory-verbal therapy; preoperative CT and MRI.
Demographics
Table 1 summarizes the demographic data and the status of the cochlear nerve of both the control and study groups. Table 2 summarizes the mean age characteristics of the two groups.
Outcome measures
Several audiometric, auditory perception, and speech and language outcome measures are routinely taken after implantation. Auditory perception tests are selected from the Evaluation of Auditory Responses to Speech (EARS) test battery: Categories of Auditory Performance (CAP), Listening Progress Profile (LIP), Meaningful Auditory Integration Scale (MAIS), and the Monosyllabic Trochee Polysyllabic (MTP) tests. Speech intelligibility and language development tests are also selected from the EARS test battery: Meaningful Use of Speech Scale (MUSS) and Speech Intelligibility Rating (SIR). The children’s CAP and SIR scores that were measured 2 years after implantation were considered in this chart review to facilitate a comparison between the study outcomes and the results of other studies.
Results
The first group consisted of seven children who received unilateral CIs; five in the left ear and two in the right ear. The mean age at cochlear implantation was 2.57 ± 1.13 years (range 1.5–2.5 years). MRI of the internal auditory canal revealed that two children had a hypoplastic cochlear nerve and five children had an aplastic auditory nerve. The second group consisted of seven children who received unilateral ABIs; three in the left ear and four in the right ear. The mean age at implantation was 3.43 ± 0.53 years (range 2–4 years). All children in the ABI group had bilateral absent cochlear nerves on MRI of the internal auditory canal (demographic data are shown in Tables 1 and 2).
Table 3 shows the mean and standard deviation of post-operative aided PTA and SDT in both groups. The mean PTA of the CI group was 60.44 (± 22.35) dB HL and 49.22 (± 17.59) dB HL for the ABI group. Three children from the CI group and four children from the ABI group achieved aided PTA of 40 dB HL or better. The group mean SDT was 56.42 ± 22.67 dB HL for the CI group and 41.43 ± 18.19 dB HL for the ABI group.
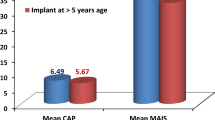
The assessment of auditory perception in the CI group revealed the following: CAP 1.28 (± 2.21), LIP 12 (± 20.49), MAIS 10.28 (± 15.98), and MTP 1.50 (± 3.96). Assessment of auditory perception in the ABI group revealed: CAP 2.87 (± 1.88), LIP 26.25 (± 20.68), MAIS 19.12 (± 12.60), and MTP 5.62 (± 7.76) (Table 4). The mean of speech intelligibility and language development in CI group are MUSS 7 (± 9.84) and SIR 0.42 (± 0.78). On the other hand, the mean scores of the ABI group are MUSS 8 (± 3.92) and SIR 0.62 (± 1.06) (Table 5).
Discussion
In the present study, we reviewed the auditory perception and speech and language outcomes of cochlear implantation and of auditory brainstem implantation in children with various conditions of the cochlear nerve. To assess which implantation method might be most beneficial to each pediatric population, we compared our results to the literature. The audiological outcomes of the ABI group are in agreement with the consensus statement made by Sennaroğlu et al. [9], who reported that a PTA between 30 and 60 dB HL can be achieved with an ABI.
Post-implantation outcome measures of the CAP, LIP, MAIS, MUSS, SIR, and MTP were obtained for all subjects included in the study. However, only the CAP and SIR results were analyzed for interpretation and comparison of the outcomes with other relevant studies. The mean CAP score of the CI group was 1.29; a CAP score of 1 indicates the awareness of environmental sounds. Five out of the seven participants in the CI group scored 0, which means that they showed no awareness of environmental sounds. These participants all had auditory nerve aplasia, which is probably the reason for their poor performance with the CI. One participant (her age at implantation was 2 years) scored 4 which means that she can discriminate some speech sounds without lip reading. Another participant (aged 7) scored 5, which corresponds to understanding common phrases without lip reading. This participant’s age at implantation was 4 years. Her post-implantation mode of communication is oral, which means that her CAP score is a reliable indication of her auditory perception. Both participants had auditory nerve hypoplasia.
Govaerts et al. [10] reported that pediatric CI users with an age at implantation between 2 and 4 years generally tend to achieve a CAP score of 5, 2 years after implantation. At least half of them achieve scores of 6 or 7 after 3 years (i.e., if one were to again follow up on the whole group after 1 year). The other half achieves scores of 6 or 7, 4 years after implantation (i.e., follow-up after another 2 years). However, their study did not investigate cochlear implantation in children with cochlear nerve deficiencies; it featured a study population of children with normal cochleae. That might explain why our two participants with cochlear nerve hypoplasia had slightly lower CAP scores. Wu et al. [6] made a similar observation: the CAP scores of children with cochlear nerve hypoplasia were not significantly different from the CAP scores of children without any nerve deficiency, once matched for age, hearing threshold, and device use. The CAP scores of children with cochlear nerve aplasia were, however, significantly lower than those of children without any nerve deficiency, once matched for age, hearing threshold, and device use.
The mean CAP score of the ABI group was 2.57; a CAP score of 3 corresponds to the ability to identify environmental sounds. Four participants scored four; these participants had an age at implantation of 3–4 years. One participant (aged 4 years) scored 0, which means that this participant had no awareness of environmental sounds. Another participant (aged 7 years) scored 1; the awareness of environmental sounds. After 2 years of follow-up, these two participants have not yet derived benefit from auditory brainstem implantation. Notably, the 4-year-old had an age at implantation of 2 years, which means that this participant could still increase their CAP score with suitable rehabilitation.
Our results for the ABI group are in good overall agreement with the results of Bayazit et al. [3], who reported on the preliminary outcomes in 12 pediatric users of MED-EL ABI devices. The individual CAP scores of the participants ranged 0–5; five participants scored 0. The median CAP score of the study population was two. However, this study population was on average younger and less experienced with their devices than our study population. The clinical data on this study population should be considered in more detail to make a comparison with our results. Six participants had cochlear aplasia and one participant had cochlear nerve aplasia; one participant had cochlear nerve hypoplasia, an absent internal auditory canal, and Muenke syndrome. One participant received a cochlear implant prior to receiving an ABI. Five out of the twelve participants had additional non-auditory cognitive and/or intellectual disabilities, whereas none of the participants in our study group had any additional disabilities.
The SIR scores were chosen for the interpretation of the speech and language outcomes of the study participants. The group mean SIR score of the CI group was 0.42. The five participants who had a CAP score of 0 also had an SIR score of 0. These participants all had auditory nerve aplasia. The two remaining participants who had a CAP score of 4 and 5 (see the discussion about Table 4) each performed correspondingly well on the SIR scale. The participant who had a CAP score of 4 had an SIR score of 1. The participant who had a CAP score of 5 had an SIR score of 2. A SIR score of 2 indicates that while she perceives connected speech as unintelligible, intelligible speech is starting to develop with single words when a lot of context is provided, and lip-reading cues are provided. Note that this participant’s mode of communication is oral, so her SIR score is a reliable indicator of her speech and language skills. Both participants had auditory nerve hypoplasia. Our results for the CI group are thus consistent with those of Wu et al. [6], who observed SIR scores of 3 or higher in children with auditory nerve hypoplasia and SIR scores of 3 or lower in children with auditory nerve aplasia after 3 years of device use.
The group mean SIR score of the ABI group was 0.62. The individual SIR scores were slightly more variable than in the CI group. A similar observation was made by Colletti, and Zoccante [11], that the results of speech intelligibility and language development tend to be highly variable between individual pediatric ABI users. Five participants had an SIR score of 0. These participants had CAP scores of 0, 1, 1, 4, and 4. The remaining two participants had SIR scores of 1. Both participants had CAP scores of 4.
A more recent study [12] presented early evidence of the linguistic development in two children who underwent auditory brainstem implantation by the age of 2 years. With increasing hearing age, pre-canonical vocalizations developed into canonical babbling and prelexical vocalizations developed into lexical vocalizations. This observation suggests that long-term device use may assist in the maturation of oral production in pediatric ABI users and potentially lower their dependence on sign language in their daily communication. The developmental trends observed in both children seem to follow the same trajectory that has been observed in their normal-hearing (NH) and CI peers of the same hearing age. This further suggests that with suitable speech and language therapy, the benefits for oral language development in pediatric auditory brainstem implantation could be comparable to that seen in pediatric cochlear implantation.
The status of the auditory nerve was considered in the retrospective case review by Kutz et al. [13]. Nerve aplasia or nerve hypoplasia was identified by MRI in nine children who underwent cochlear implantation. The two children who had auditory nerve hypoplasia developed early and consistent closed-set word recognition, respectively, but they could not achieve the levels of speech understanding that children with normal auditory nerves achieved over the same period. Although the speech awareness threshold (SAT) and speech perception category (SPC) scores were used as outcome measures in this study, our results are consistent with their conclusions. Our individual results of CI trials for children with auditory nerve hypoplasia delivered acceptable outcomes of auditory and speech abilities as measured by CAP and SIR. This indicates that cochlear implantation can be considered a potential option for those children with CN hypoplasia.
The Second Consensus Meeting on Management of Complex Inner Ear Malformations [9] reported on the long-term results in pediatric ABI users and presented a framework for the decision-making process between cochlear and auditory brainstem implantation. Clinicians reported that most pediatric ABI users took longer than their hearing aid and CI peers to spontaneously respond to environmental sounds. Consequently, pediatric ABI users’ exposure to spoken language is extremely limited. Even with long-term ABI use, their expressive and receptive language developments remain delayed compared to their NH and CI peers. As with CI surgery, ABI surgery should occur before the age of 2 years, preferably age 1–1.5 years, for optimal outcomes in auditory perception and language development [9].
In contrast to these reports of promising results with the ABI, Merkus et al. [4] concluded that the 144 cases they reviewed all had unsatisfactory results with their ABIs and could have been CI recipients. Speech perception outcomes with CIs are generally better than those with ABIs. The authors saw only one benefit of auditory brainstem implantation—an ABI is very effective at facilitating oral communication and supporting lip reading. The stringent ABI indications that the authors identified from their review highlight that cochlear implantation remains the preferred and most reliable method of rehabilitation in terms of the safety and the predictability of its auditory and speech outcomes.
There are a few limitations of the current study, for instance the small sample size and the relatively short duration of follow-up post-implantation (2 years). However, due to the complex setup required for ABI surgeries, there was a limitation on the number of recipients that met the selection criteria and who could be recruited for the current study. Moreover, this might be considered a preliminary study with a follow-up period of 2 years. It would be of interest to our clinic and as a contribution to the literature to follow up on the study participants over another 2 years. This would allow us to measure changes in the trajectories of both auditory perception and language development especially for our youngest participants.
Conclusion
The results of our preliminary study were in good general agreement with reported auditory perception and speech and language development outcomes of pediatric auditory brainstem implantation. We added to the growing body of literature on the importance of verifying the status of the cochlear nerve and identifying the type of nerve deficiency in the decision-making process leading up to pediatric auditory brainstem implantation.
References
Deep NL, Roland JT Jr (2020) “Auditory brainstem implantation: candidacy evaluation, operative technique, and outcomes.” Otolaryngol Clin North Am 53(1):103–113. https://doi.org/10.1016/j.otc.2019.09.005
Glastonbury CM, Davidson HC, Harnsberger HR, Butler J, Kertesz TR, Shelton C (2002) “Imaging findings of cochlear nerve deficiency.” AJNR Am J Neuroradiol 23(4):635–643
Bayazit YA et al (2014) “Methods and preliminary outcomes of pediatric auditory brainstem implantation.” Ann Otol Rhinol Laryngol 123(8):529–536. https://doi.org/10.1177/0003489414525123
Merkus P et al (2014) “Indications and contraindications of auditory brainstem implants: systematic review and illustrative cases.” Eur Arch Otorhinolaryngol 271(1):3–13. https://doi.org/10.1007/s00405-013-2378-3
Noij KS et al (2015) “Systematic review of nontumor pediatric auditory brainstem implant outcomes.” Otolaryngol Head Neck Surg 153(5):739–750. https://doi.org/10.1177/0194599815596929
Wu CM, Lee LA, Chen CK, Chan KC, Tsou YT, Ng SH (2015) Impact of cochlear nerve deficiency determined using 3-dimensional magnetic resonance imaging on hearing outcome in children with cochlear implants. Otol Neurotol 36(1):14–21
Teagle HFB, Henderson L, He S, Ewend MG, Buchman CA (2018) “Pediatric auditory brainstem implantation: surgical, electrophysiologic, and behavioral outcomes.” Ear Hear 39(2):326–336. https://doi.org/10.1097/aud.0000000000000501
Rajeswaran R, Kameswaran M (2020) “Auditory brainstem implantation (ABI) in children without neurofibromatosis type II (NF2): communication performance and safety after 24 months of use.” Cochlear Implant Int 21(3):127–135. https://doi.org/10.1080/14670100.2019.1690264
Sennaroğlu L et al (2016) “Consensus statement: long-term results of ABI in children with complex inner ear malformations and decision making between CI and ABI.” Cochlear Implant Int 17(4):163–171. https://doi.org/10.1080/14670100.2016.1208396
Govaerts PJ et al (2002) Outcome of cochlear implantation at different ages from 0 to 6 years. Otol Neurotol 23(6):885–890. https://doi.org/10.1097/00129492-200211000-00013
Colletti L, Zoccante L (2008) “Nonverbal cognitive abilities and auditory performance in children fitted with auditory brainstem implants: preliminary report.” Laryngoscope 118(8):1443–1448. https://doi.org/10.1097/MLG.0b013e318173a011
Faes J, Gillis S (2019) “Auditory brainstem implantation in children with hearing loss: effect on speech production.” Int J Pediatr Otorhinolaryngol 119:103–112. https://doi.org/10.1016/j.ijporl.2019.01.014
Kutz JW Jr, Lee KH, Isaacson B, Booth TN, Sweeney MH, Roland PS (2011) “Cochlear implantation in children with cochlear nerve absence or deficiency.” Otol Neurotol 32(6):956–61. https://doi.org/10.1097/MAO.0b013e31821f473b
Acknowledgements
The authors are grateful to the Deanship of Scientific Research, King Saud University, for providing funding through the Vice Deanship of Scientific Research Chairs. This research project was recommended by the Saudi Otorhinolaryngology Society. The authors would like to thank Wilnelia Adams for her help in editing the paper.
Funding
There are no funders to report for this submission.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical approval was obtained by the Local Ethical Committee. All procedures performed in studies involving human par- ticipants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Written consent was taken from all participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yousef, M., Mesallam, T.A., Almasaad, A. et al. Cochlear implantation versus auditory brainstem implantation in children with auditory nerve deficiencies. Eur Arch Otorhinolaryngol 279, 1295–1300 (2022). https://doi.org/10.1007/s00405-021-06792-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-06792-8