Abstract
The decision whether to perform an elective neck dissection in patients with head and neck squamous cell carcinoma and clinically negative lymph nodes (cN0) is made based on the probability of micrometastases in the neck for the given subsite and size of the primary. A retrospective chart review was performed of 203 patients with hypopharyngeal SCC who received a bilateral neck dissection. The frequency of histologically unveiled bilateral neck metastases was determined. A high frequency of contralateral metastases above 20% was detected for all carcinomas affecting the midline and those involving the medial wall of the pyriform sinus except of T1-stages (13%) and a low frequency for laterally located primaries (3%). Ipsilateral nodal status predicted contralateral neck metastases. Bilateral neck dissection should be recommended for primaries affecting the midline and T2–4 tumors involving the medial wall of the pyriform sinus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The management of the contralateral N0 neck (neck without clinical evidence for cervical lymph node metastases) in patients with hypopharyngeal carcinoma is controversial [6, 10]. It is widely accepted among head and neck surgeons to perform an elective neck dissection of the N0 neck in patients with head and neck squamous cell carcinoma (HNSCC), when the cervical metastatic risk exceeds 15–20% [6, 9, 17, 18]. This risk cannot accurately be estimated from the literature to date, because in most of the published studies that assessed neck dissection specimens the operation was performed bilaterally only in a small number of patients [1, 2, 12,13,14]. One recent study focused only on medial wall pyriform sinus carcinoma reporting only on patients who had received bilateral neck dissection [5].
Early studies suggested the frequency of contralateral metastases to be only around 10% [8, 15], but studies of the mid-nineties identified the contralateral neck as most frequent site of failure despite of radiotherapy. These studies identified the tumor size, a location involving the posterior pharyngeal wall or the medial pyriform sinus/outer larynx and ipsilateral nodal metastases as risk factors for contralateral cervical metastases [12, 14]. The only prospective study with serial sections of all dissected nodes indicates that the rate of occult metastases in the contralateral neck might be as high as 47%. Accordingly, a recent review about the current management of hypopharyngeal carcinoma states that clearance of the contralateral neck may be considered in the at-risked group, including those with tumors involving the medial wall of the pyriform sinus, post-cricoid region or the posterior wall, and those with ipsilateral palpable nodal metastases [4]. The aim of this retrospective analysis was to determine the probability of bilateral cervical lymph node metastases of hypopharyngeal carcinoma for the different risk situations from a large number of bilateral neck dissection specimens.
Methods
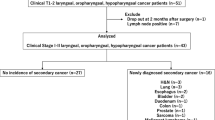
A retrospective analysis was performed of patients treated with hypopharyngeal SCC between 1990 and 2007 at the Department of Otorhinolaryngology, Head and Neck Surgery of the Ludwig-Maximilians-University of Munich, Germany. A total of 781 patients were identified from the Munich cancer registry database and history files were obtained from the clinics archive. Either no or insufficient history files were available of 169 patients. 263 patients had (chemo-) radiation as final treatment and 3 patients received no treatment at all. Of the 346 surgically treated patients 46 were excluded from final data analysis because they had other malignant diseases simultaneously or in their medical history and one patient because he had a tumor histology other than squamous cell carcinoma. 40 patients could not enter the final data analysis because their history files did not contain reports precisely determining primary location or tumor stage and in 6 patients this information was not available because the surgery comprised either the tumor resection or the neck dissection alone.
203 patients received a tumor resection together with a bilateral neck dissection as primary treatment and were included into the main data analysis. Only tumor resection and unilateral neck dissection was performed in 50 patients.
To assess the bias that is inflicted by the surgeon’s decision to perform either unilateral or bilateral neck dissection, a second data analysis was performed of all 253 patients who had received either unilateral or bilateral neck dissections under the assumption, that none of the unilaterally operated patients had contralateral cervical metastases.
The frequency of bilateral and contralateral cervical lymph node metastases was determined depending on the T-classification of the tumor, on whether the primary tumor affected the midline or not, for different subsites of the primaries not affecting the midline and depending on the ipsilateral nodal status (N0, N1 and N2 or greater). The different subsites investigated were medial wall of pyriform sinus together with post-cricoid region, anterior wall/apex of pyriform sinus, lateral wall of pyriform sinus and posterior pharyngeal wall. Due to the proximity of the subsites most of the tumors involved more than one subsite. Regarding the established elevated risk for contralateral metastases from tumors involving the medial wall of the pyriform sinus we compared this subsite with the more laterally located subsites moving from lateral to medial: tumors involving only the lateral wall of pyriform sinus (LW) vs. medial wall/post-cricoid region (MW); tumors involving the lateral and anterior wall (LW + AW) vs. MW; tumors involving the lateral and posterior wall (LW + PW) vs. MW. To compare the areas at high risk for contralateral metastases we compared tumors crossing the midline with tumors of the medial wall of the pyriform sinus without midline affection. SigmaPlot 12.5 was used to analyze the results. The relationship between variables and bilateral neck metastases was analyzed by either Chi-squared (χ 2) or Fischer’s exact test. p < 0.05 was considered significant.
Results
Of the 203 patients who received a bilateral neck dissection, 19.4% were female and 80.6% male. Mean age at the time of treatment was 56.5 years (range 29–84 years). Of the 406 neck dissections, 46 were radical, 36 modified radical and 324 selective neck dissection usually comprising the regions II–V.
Out of the 203 patients who received a bilateral neck dissection, 42 had contralateral neck metastases (20.7%). The frequency depending on different risk factors is given in Table 1 both for the patients who had received a bilateral neck dissection and for the patients who received either bilateral or unilateral neck dissection, which assumed that none of the unilaterally operated patients had contralateral cervical metastases.
Less bilateral metastases were detected in T1-tumors compared to more advanced primaries and in tumors that did not involve the midline compared to those involving the midline. No contralateral metastases were found in tumors of the lateral hypopharyngeal wall and those spreading towards the posterior wall without reaching the midline. One contralateral metastasis was found among the tumors that affected both the lateral and the anterior wall of pyriform sinus (n = 10). The risk of contralateral metastasis was markedly elevated when the medial wall of the pyriform sinus was involved even without midline affection (28 out of 136, 20.7%). We detected one isolated contralateral metastasis in a T4-tumor involving all regions but without crossing the midline among 40 patients with ipsilateral N0 necks. Patients with one or more ipsilateral neck metastases showed significantly more bilateral metastases (Table 1).
Discussion
The presented study is based on routine clinical documentation. There was no particular processing of the pathologic specimens focusing on the detection of micrometastases. This may result in a certain unreliability of the data with underestimation of the true metastatic risk, which is an inherent problem of every retrospective analysis. However, this study design allowed the analysis of a larger number of patients, offering the largest available data set on metastatic risk of hypopharyngeal cancer to the contralateral neck.
Feind and Cole [8] already discussed the issue of contralateral metastases in head and neck cancer based on radical neck dissection specimens. Of 50 patients with hypopharyngeal SCC 5 had contralateral metastases, all of which had either the posterior pharyngeal wall or the post-cricoid region involved [8]. Lindberg [15] published a comprehensive work on the clinical nodal status in head and neck cancer determined by palpation at admission for definitive treatment. The series encompassed 267 hypopharyngeal tumors with 28 contralaterally N+ necks detected [15]. Johnson et al. identified the neck as most frequent site of failure in 169 patients with surgically treated hypopharyngeal carcinomas. The majority of the patients (133) received a unilateral neck dissection and only 22 patients received a bilateral neck dissection. 12 neck failures occurred ipsilaterally and 15 contralaterally. All contralateral failures occurred in unoperated necks and 12 of 15 (80%) had received radiotherapy. A location of the primary in the medial pyriform sinus was identified as a significant risk factor for contralateral failure [12]. Kowalski and co-workers performed a retrospective analysis of 218 patients who received unilateral (n = 189) or bilateral (n = 27) neck dissection during primary treatment. Out of 35 neck recurrences 27 occurred in contralateral necks, none of which had been dissected. Predictors of contralateral neck failure were T- and N-stage, epilarynx and posterior wall involvement, hemilarynx fixation and ipsilateral level 1 metastases [14]. Koo et al. analyzed 43 specimens from bilateral neck dissections of patients with clinical N0 neck contralaterally. They found 7 occult metastases in patients with clinical N+ necks ispilaterally (n = 27) while all patients with ipsilateral cN0 necks (n = 16) were free of metastases contralaterally. A primary tumor crossing the midline was also a predictor of contralateral occult metastases, while T-stage, number of ipsilateral positive nodes, extracapsular spread and medial vs. lateral pyriform sinus involvement was not [13]. A study of Amar et al. retrospectively followed 147 surgically treated patients with hypopharyngeal carcinoma. Out of 48 patients who received a bilateral neck dissection, 22 had clinically palpable and 29 finally histologically proven metastases in the contralateral neck. 12 unilaterally operated patients suffered recurrence in the contralateral neck, 8 of them were surgically salvaged, 3 of them remained disease free after 162 months. Primary locations involving the medial wall of the pyriform sinus or those crossing the midline, palpable ipsilateral metastases and clinically stage IV-disease were predictors of contralateral metastases [1]. Chung et al. assessed 68 medial wall pyriform sinus carcinoma patients who had received a bilateral neck dissection. 10 patients (14.7%) had contralateral metastases and all of these patients also had ipsilateral metastases [5].
From the only prospective study conducted by Buckley and MacLennan, it becomes clear that all of the aforementioned studies as well as our investigation might dramatically underestimate the true risk of contralateral metastases. The authors prospectively evaluated the metastatic risk of laryngeal and hypopharyngeal cancers with serial 6 µm-sections of all dissected nodes. They found that one-third of the metastatic nodes were smaller than 3 mm in diameter. Out of 15 contralateral N0 necks of hypopharyngeal tumors, 7 (47%) contained micrometastases [2].
The presented study is the so far largest series of patients with hypopharyngeal carcinomas who have received bilateral neck dissections. This data is up to date the best available for risk assessment of bilateral neck metastases in the individual patient with hypopharyngeal carcinoma.
Interpreting the data, some bias should be considered: The patients who received bilateral neck dissection represent a selected group of patients with hypopharyngeal carcinoma. Patients with smaller tumors have a lower risk of bilateral metastases and those were more likely to receive a unilateral neck dissection (78% T1 and T2). Among the patients treated with (chemo-) radiation 75% had T4 tumors. Additionally, patients with extensive cervical metastases will have preferably received (chemo-) radiation. Therefore, performing an analysis of the group of patients who received bilateral neck dissection, the risk of bilateral metastases for small tumors (T1 and T2) is likely to be overestimated, but underestimated for advanced tumors.
While 203 patients received a bilateral neck dissection, 50 patients had neck surgery only unilaterally. The decision of the surgeons to perform the neck dissection bilaterally suggests an initially higher risk for bilateral neck metastases. To address this bias, a second calculation was performed under the unlikely assumption that none of the unilaterally operated patients had metastases of the contralateral neck. However, these numbers consequently represent a definite underestimation of the risk of bilateral neck metastases.
263 patients received (chemo-) radiation as initial therapy. During the whole study period until present, surgery used to be the first line therapy for hypopharyngeal carcinoma at our institution. (Chemo-) radiation was chosen as initial therapy if surgery could not be performed due to the extent of tumor growth and/or an inoperable condition of the patient or because the patient refused to have surgery. A frequent limitation for surgery might be an infiltration of neck metastases and the primary, respectively, into the carotid artery and/or the prevertebral fascia. By trend, the group of patients who received primary (chemo-) radiation is likely to contain a higher proportion of patients with widespread neck metastases in general and therefore also more patients with bilateral metastases. A detailed analysis of these patients—as performed for the patients after unilateral neck dissection—was not performed due to the high degree of uncertainty of clinical tumor staging.
Metastatic spread of a cancer is a function of its specific propensity to metastasize and time [7]. Our data show expectedly that T1 tumors have a lower risk of contralateral metastases compared to more advanced primaries, but T2, 3 and 4 tumors had an equal risk of contralateral metastases. This has also been observed for oropharyngeal carcinoma in a similarly designed study [16]. Tumors with high metastatic potential might be diagnosed due to cervical masses at an earlier local stage or might be no longer amenable to surgery at a locally advanced stage. Tumors still amenable to surgery at T3 or T4 stages may represent selected cancers with a biologically lower metastatic potential and the T-stage might thus be of limited significance to assess the metastatic risk to the contralateral neck in patients to be treated surgically.
A clinical marker for the general propensity of a tumor to metastasize is the nodal status of the ipsilateral neck, which therefore is an important predictor of contralateral neck metastases [1, 4, 5, 10, 13, 14]. In this study, we had one out of 40 patients with ipsilateral N0 necks who had a contralateral metastasis (2.5%), 7 out of 48 (14.6%) with ipsilateral N1-necks and 34 out of 115 (30.0%) with N2 or greater.
A prerequisite for contralateral neck metastases of a tumor is that the anatomic area of tumor growth has a drainage of lymphatic fluids to the contralateral neck. Even tumors with high metastatic potential will not spread to the contralateral neck from areas with strictly unilateral lymphatic drainage. Our dataset is the first one large enough to reliably define those safe areas. Out of 34 tumors that were located laterally and did neither reach the midline at the posterior pharyngeal wall nor the medial wall of the pyriform sinus anteriorly, only one—a tumor that infiltrated the apex of the pyriform sinus—had spread to the contralateral neck. Interestingly, none of the nine tumors that extended on to the posterior wall but did not reach the midline exhibited contralateral metastases. In contrast to that, Kowalski et al. found a higher rate of contralateral neck failure in posterior wall tumors, but they did not differentiate whether those tumors affected the midline or not [14]. The supraglottic larynx has a bilateral lymphatic drainage and expectedly—as first described by Kowalski et al. [14]—a significant proportion of 20.7% of tumors showed contralateral neck metastases when the medial wall of the pyriform sinus was affected even without midline involvement. This rate was higher compared to the observations of Chung et al. from 68 bilateral neck dissection specimens from this tumor location with 14.7% bilateral metastases [5]. Obviously, the proximity to the midline will be of importance for the risk of bilateral neck metastases. On this note, our data show that tumors crossing the midline have a higher risk of contralateral metastases compared to all tumors that do not affect the midline, but also compared to the tumors encompassing the medial wall of the pyriform sinus but without midline affection.
Detailed knowledge about the metastatic risk of hypopharyngeal cancer is an important basis for whatever treatment modality is employed. The alternative to the bilateral neck dissection is radiotherapy of the contralateral neck in case of a relevant risk of bilateral metastases, particularly in patients receiving planned adjuvant radiotherapy post-op. In contrast to radiotherapy, the neck dissection is not only a therapeutic procedure, but also a diagnostic one since it allows for the most reliable staging [6, 9, 18]. The selective neck dissection has a low long-term morbidity. The only frequent problem of accessory nerve damage with subsequent shoulder dysfunction can be minimized when level IIB and V are not dissected [3]. Metastases in the contralateral N0 neck of hypopharyngeal carcinoma are only found in levels IIa, III and IV [2, 5, 11], so that selective dissection of these levels should be sufficient. As such limited procedure, the neck dissection has few complications or non-transient side effects and offers the advantage of an accurate staging [9, 18]. For patients with surgically treated hypopharyngeal carcinoma with a relevant risk of contralateral metastases we, therefore, recommend neck dissection instead of prophylactic radiation therapy of the neck in most cases.
Based on the widely accepted practice to perform a neck dissection in the N0 neck when the individual metastatic risk exceeds 15–20%, the following recommendations might be made based on our data:
In tumors of the lateral hypopharyngeal wall that extend anteriorly at most into the apex of the pyriform sinus, but not to its medial wall and/or posteriorly onto the posterior pharyngeal wall, but do not affect the midline, a unilateral neck dissection seems sufficient, even in cases with ipsilateral metastases.
T1-tumors of the medial wall of the pyriform sinus showed an intermediate risk of contralateral metastases of 13.3%. In these cases, the contralateral neck dissection might be recommended in a clinical ipsilateral N+ situation. In clinically N0 necks the contralateral neck might later be irradiated when the ipsilateral neck dissection reveals neck metastases. The same regimen might make sense in laterally located tumors with limited extension onto the medial wall of the pyriform sinus.
Tumors larger than T1 with relevant tumor growth on the medial wall of the pyriform sinus and tumors crossing the midline should be treated with bilateral neck dissection.
The retrospective data supports our surgical planning. However, prospective data on the metastatic behavior of the different subsites of hypopharyngeal cancers and cancers of other origin in the head and neck are warranted in the future. Based on such data surgical intervention and accompanying morbidity could be significantly reduced keeping up ideal cancer treatment and patient safety.
References
Amar A, Dedivitis RA, Rapoport A et al (2009) Indication of elective contralateral neck dissection in squamous cell carcinoma of the hypopharynx. Braz J Otorhinolaryngol 75:493–496
Buckley JG, Maclennan K (2000) Cervical node metastases in laryngeal and hypopharyngeal cancer: a prospective analysis of prevalence and distribution. Head Neck 22:380–385
Celik B, Coskun H, Kumas FF et al (2009) Accessory nerve function after level 2b-preserving selective neck dissection. Head Neck 31:1496–1501
Chan JY, Wei WI (2013) Current management strategy of hypopharyngeal carcinoma. Auris Nasus Larynx 40:2–6
Chung EJ, Lee SH, Baek SH et al (2014) Pattern of cervical lymph node metastasis in medial wall pyriform sinus carcinoma. Laryngoscope 124:882–887
Coskun HH, Medina JE, Robbins KT et al (2015) Current philosophy in the surgical management of neck metastases for head and neck squamous cell carcinoma. Head Neck 37:915–926
Engel J, Eckel R, Kerr J et al (2003) The process of metastasisation for breast cancer. Eur J Cancer 39:1794–1806
Feind CR, Cole RM (1969) Contralateral spread of head and neck cncer. Am J Surg 118:660–665
Ferlito A, Rinaldo A, Silver CE et al (2006) Elective and therapeutic selective neck dissection. Oral Oncol 42:14–25
Ferlito A, Shaha AR, Buckley JG et al (2001) Selective neck dissection for hypopharyngeal cancer in the clinically negative neck: should it be bilateral? Acta Otolaryngol 121:329–335
Gross BC, Olsen SM, Lewis JE et al (2013) Level IIB lymph node metastasis in laryngeal and hypopharyngeal squamous cell carcinoma: single-institution case series and review of the literature. Laryngoscope 123:3032–3036
Johnson JT, Bacon GW, Myers EN et al (1994) Medial vs lateral wall pyriform sinus carcinoma: implications for management of regional lymphatics. Head Neck 16:401–405
Koo BS, Lim YC, Lee JS et al (2006) Management of contralateral N0 neck in pyriform sinus carcinoma. Laryngoscope 116:1268–1272
Kowalski LP, Santos CR, Magrin J et al (1995) Factors influencing contralateral metastasis and prognosis from pyriform sinus carcinoma. Am J Surg 170:440–445
Lindberg R (1972) Distribution of cervical lymph node metastases from squamous cell carcinoma of the upper respiratory and digestive tracts. Cancer 29:1446–1449
Olzowy B, Tsalemchuk Y, Schotten KJ et al (2011) Frequency of bilateral cervical metastases in oropharyngeal squamous cell carcinoma: a retrospective analysis of 352 cases after bilateral neck dissection. Head Neck 33:239–243
Pitman KT (2000) Rationale for elective neck dissection. Am J Otolaryngol 21:31–37
Wei WI, Ferlito A, Rinaldo A et al (2006) Management of the N0 neck–reference or preference. Oral Oncol 42:115–122
Acknowledgements
We did not receive grant support or relevant help of other individuals in the preparation of the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No financial or other relationships exist which may lead to a conflict of interest.
Human and animal rights statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was not necessary since the study consisted of a retrospective chart review only.
Rights and permissions
About this article
Cite this article
Olzowy, B., Hillebrand, M. & Harréus, U. Frequency of bilateral cervical metastases in hypopharyngeal squamous cell carcinoma: a retrospective analysis of 203 cases after bilateral neck dissection. Eur Arch Otorhinolaryngol 274, 3965–3970 (2017). https://doi.org/10.1007/s00405-017-4724-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-017-4724-3