Abstract
To provide retrospective, descriptive information on patients with cervical necrotizing fasciitis treated at a single center during the years 1998–2014, and to evaluate the outcome of a newly introduced treatment strategy. Retrospective analysis of clinical data obtained from medical records. Mortality, pre-morbidity, severity of illness, primary site of infection, type of bacteria, time parameters. The observed 3-month mortality was 6/59 (10 %). The most common initial foci of the infection were pharyngeal, dental or hypopharyngeal. The most common pathogen was Streptococcus milleri bacteria within the Streptococcus anginosus group (66 % of the cases). Using a combined treatment with early surgical debridement combined with hyperbaric oxygen treatment, it is possible to reduce the mortality rate among patients suffering from cervical necrotizing fasciitis, compared to the expected mortality rate and to previous historical reports. Data indicated that early onset of hyperbaric oxygen treatment may have a positive impact on survival rate, but no identifiable factor was found to prognosticate outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical necrotizing fasciitis (CNF) is a rare and potentially fatal infectious disease, which calls for early recognition and treatment [1, 2]. The condition was first described in the late nineteenth century [3] and later characterized as “necrotizing fasciitis” in 1952 [4]. Today, the incidence of CNF has been reported to be two per million per year [5], with reported mortality rates between 6 and 64 % [6–9].
The disease usually begins as a bacterial infection of dental or pharyngeal origin [2, 5, 10]. In contrast to forming a defined abscess, the infection spreads rapidly along the fascial planes, which become necrotic. Initially, the underlying muscles and overlapping skin are spared [11, 12], but the infection and the inflammatory response cause microembolies and hampered circulation, which leads to necrosis also to skin and soft tissue [13]. This generates further bacterial growth, and the patient becomes septic, with affected vital parameters [14, 15]. Without prompt treatment, the infection leads to multi-systemic organ failure, and death. For diagnostic purpose, attempts have been made to stage the clinical progress of the disease: stage 1 (early) includes tenderness, erythema, swelling and calor; stage 2, blistering and bullae and stage 3, crepitus, skin anesthesia, and skin necrosis [12, 16]. Nevertheless, to make an adequate diagnose in an early stage is often difficult. CNF can be mistaken for erysipelas or other localized infection, but should be considered among patients with disproportionate pain [12, 17].
Due to low incidence and diagnostic uncertainties, previous literature on CNF is limited. Given the high mortality rate and the presumed importance of early treatment, there is a clear need for more clinical data. The aim of the present study was to provide retrospective, descriptive information on patients diagnosed with CNF at a single center during the years 1998–2014, and to evaluate the outcome of a newly introduced treatment strategy. These patients were all treated with early surgical debridement, antibiotic treatment and daily hyperbaric oxygen (HBO) treatments at 2.8 bars.
Methods
The study is a retrospective, descriptive analysis of clinical data obtained from medical records and registers regarding patients diagnosed with CNF at the Karolinska University Hospital, Stockholm, during the years 1998–2014. In 1998, a new treatment protocol was introduced, including early and repetitive surgical debridement to eradicate all necrotic tissue, broad-spectrum antibiotics (clindamycin 600 mg three times daily, +Cilastatin/Imipenem 1000 mg/1000 mg four times daily) and HBO treatments (at 2.8 bar twice daily during 100–285 min, 3.9–113.4 ATA (atmospheric hours of oxygen) totally per patient).
Patient identification and inclusion
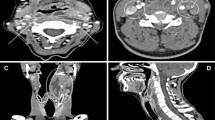
Patients were identified from a local quality register and through searching for International Classification of Disease (ICD) codes M726 (necrotizing fasciitis) and M354 (diffuse fasciitis) in the medical record database. Of the 166 identified patients, 59 met the inclusion criteria, defined as: (1) severe soft tissue infection in head and neck area with pain out of proportion, (2) radiological signs of free gas in tissue, and/or fascial oedema (computed tomography) (3) confirmed necrotic tissue at surgery associated with liquefied purulent secretion and a rotten, waste like odor, and (4) deranged vital parameters and need for intensive care. Patients with localized infections (erysipelas, cellulitis) and abscesses were excluded. In six cases, biopsies had been sent for pathological confirmation of diagnosis, which all showed signs of inflammation and necrosis.
Of the 59 included patients, 37 were originating from the Stockholm area and primarily handled at Karolinska Hospital, whereas 22 patients were referred from other parts of the country.
Surgical management
The aim of the surgical management was to remove all necrotic tissue to prevent further spread of the infection. This was performed through wide skin incisions over the affected region. Most often bilateral neck incisions were needed with extension of the incisions along the fascia planes up to the skull base. Incisions were sometimes needed further down over the shoulders, thorax and back region. The wounds were left open covered with saline dressings and drainage until no further spread was noted during the daily or twice daily check-ups by the surgeons. In cases where the infection spread to mediastinum thoracotomy was performed and multiple drainages were used. Notably nerves and vessels were rarely affected and could generally be spared as an organ preservation approach was used. Vessels were ligated only for exposure purposes. To prevent unnecessary spread of infection to the mediastinum patients were kept intubated as tracheostomy was avoided until the infection was under total control. The sequelae were mainly disfiguring scars, in some patients requiring secondary reconstructive surgery.
Collected data and parameters of interest
Information was collected regarding demographic data, previous medical history, foci of infection, and time parameters such as time from hospitalization to surgical intervention and duration of intensive care. The number of surgical procedures was documented. Based on the appearance of the tissue during surgery, extent of the disease was categorized into (1) necrotic sub-dermal tissue with intact fascia, (2) necrotic fascia and necrotic subcutaneous tissue but with preservation of the muscle tissue, or (3) necrotic fascia, muscle, fat and sometimes overlaying skin. Bacterial growth in cultures from blood or tissue was noted, as well as total HBO dose and extent of intensive care (need for dialysis, inotropic support and assisted ventilation). The APACHE-II score (clincalc.com) was used as a tool to measure severity of the illness and to calculate the estimated mortality risk, based on archived data from the first 24 h in the intensive care unit.
Parameters of interest were: mortality, pre-morbidity, severity of illness, and time parameters such as time to infection control. Infection control was defined as no further development of necrosis, C-reactive protein <100 and no need for inotropic support.
Statistical analyses
Mann–Whitney U test was used to analyze differences between two unrelated observations. The variance ratio test was used for the comparison of the variability of data in two populations.
Classified data from two independent populations were compared by the Fischer exact test. Standardized mortality ratio (SMR) and its 95 % confidence intervals were calculated as given by Liddell [18].
Statistics were evaluated by MS Excel (Microsoft Corporation, Redmond, Washington USA) and Graph Pad Instat 3.10 (Graph Pad Software inc. San Diego, USA).
p values less than 0.05 were considered as statistical significant. All reported p values were from two-sided tests.
Results
Age, gender and previous medical history
Fifty-nine patients met the inclusion criteria (30 female, 29 male). Median age was 60 years (range 17–89 years). Among the survivors the median age was 59 years (range 17–89 years) and in the group of diseased 64 years (range 53–75 years). The patients with a previous medical history were categorized into: heart and vascular diseases (n = 16), diabetes mellitus (n = 10), drug abuse (n = 7), pulmonary diseases and asthma (n = 6), malignancy (n = 3), psychiatric diseases (n = 3), or “other”, such as gastric reflux, Guillan Barré syndrome, or acne (n = 18). The remaining patients had no previous medical history and were considered healthy (n = 11) (Fig. 1).
Extent of necrosis
The necrotic process involved subcutaneous fatty tissue (n = 8), extending to fascia (n = 21), and muscle (n = 29). In one case data is missing, since the patient was primarily cared for at another hospital. Thoracic spread of the infection was observed in 23 patients, of which 4 patients died.
Foci of primary infection
The most common initial focus of the infection was pharyngeal (n = 23), dental (n = 20) or hypopharyngeal (n = 8). More rarely, the infection developed after surgical procedures or trauma (n = 4), salivary gland infection (n = 1), or axillary skin (n = 1). In two cases, the initial focus was not identifiable (Fig. 2).
Bacteria
Perioperative cultures from wound/tissue and blood were collected in all patients. Monobacterial growth was found in 29 patients, polybacterial growth in 25 patients, whereas no bacterial growth was detected in 5 patients. Gram-positive cocci were found in 48/59 (81 %) of the cases, of which the most common pathogen was Streptococcus milleri bacteria within the Streptococcus anginosus group, found in 39/59 (66 %). Beta-haemolytic streptococci (GAS) were seen only in 3/59 (5.1 %) of the cases. In 18/59 (31 %) of the cases both gram-positive cocci and anaerobic bacteria were found together (Table 1).
Time aspects
Early diagnosis and treatment are clinically emphasized and therefore attempts were made to analyze the time intervals (in days) between first healthcare contact to: (a) hospitalization (b) diagnosis (c) surgical treatment, (d) HBO treatment and to (e) infection control. Time intervals were generally slightly shorter for surviving patients compared to diseased patients, but did not reach statistical significance at a 5 % significance level (Mann–Whitney U test, two-tailed p value, Table 2).
Severity of the illness
Data for calculating the APACHE-II score was available in 54/59 patients. Median value was found to be 18 points (range 4–33 points). Median time in the intensive care unit was 15 days (2–46 days) mechanical ventilation 14 days (0–56 days). Total number of surgical debridement was 4 (median value; range 1–18). 14 % of the patients were in need of dialysis.
Mortality
The observed 3-month mortality was 6/59 (10 %). Derived from the Apache-II score, the estimated mortality risk was calculated to 35.9 % (median value; range 5.1–78.9 %) for all patients, with no statistical difference comparing surviving and diseased patients (p = 0.6327 Mann–Whitney U test). The standardized mortality rate (SMR) = (observed mortality/expected mortality), was found to be 0.267 (95 % Cl 0.0976–0.5816).
The clinical characteristics of the six patients with fatal outcome are listed in Table 3. Two of these patients had significant premorbidity (recurrent malignant disease and multiple cerebrovascular lesion, respectively), but in one case the patient had no previous medical conditions. four of the diseased patients had thoracic engagement of the infection.
HBO treatment
The patients received one to two HBO treatments each day, at 2.5 or 2.8 bar pressure. HBO treatment was generally started within 24 h from the first surgical intervention; 26 patients were treated the same day and 14 at 1 day after surgery. In one case, the HBO treatment was initiated 15 days before the onset of CNF due to another disease, and in one case the HBO treatment was resigned because of the patient’s status with a background malignancy. In three cases, the time of onset of HBO was unclear.
The total HBO dose varied from 3.9 to 113.4 atmosphere absolute (ATA) hours. The total number of treatments varied from 1 to 30, reflecting the varying time to control of infection. Of the six cases with fatal outcome, one did not receive HBO treatment, three started HBO treatment the same day as surgery, and two patients started HBO at 3 and 5 days after first surgical intervention.
Discussion
Synopsis of key findings
This report describes the clinical parameters and outcomes in 59 patients treated for CNF, a rare but clinically significant infectious disease. To our knowledge, this is one of the largest clinical studies focusing specifically on CNF. Compared to historical data [8, 19, 20] and to the estimated mortality risk, the observed mortality rate was found to be relatively low (10 %), which may be attributed to the treatment strategy introduced in 1998. At this time point, a protocol for cervical fasciitis was nonexistent and in addition the patients were treated with varying approaches at different hospitals in the Stockholm area. In 1998, a reorganization took place, and all in-patient treatment of Head and Neck patients were concentrated to Karolinska University Hospital, where the existing protocol for fasciitis in various other parts of the body was adopted to include also cervical fasciitis. The main differences to earlier varied treatment strategies were a more aggressive surgical approach with leaving the wounds open until infection control, and the addition of HBO treatment. Even though the relative contribution of HBO treatment remains to be clarified, its clinical effect is judged to be important. The present report further indicates a favorable effect of early initiation of treatment, even though comparisons did not reach statistical significance.
Comparison with other studies
In a previous report, Krenk et al. [5], showed a remarkable change in mortality rate from 75 to 0 % after introducing HBO, even though the number of cases was limited. Similarly, Wolf et al. [14] reported full survival in 17 patients with CNF as well as Flanagan et al. [7] and Maisel et al. [13], when HBO was used in addition to conventional treatment including antibiotics and surgery. HBO treatment has been showed to increase the partial oxygen pressure (PO2) severalfold in the tissue, providing “guaranteed oxygenation” of hypoxic tissues and also challenging numerous enzyme systems providing antimicrobial [21], anti-inflammatory and tissue preconditioning effects. These actions may be favorable in the case of CNF, where the local milieu in the infected tissue is characterized by hypoxia, microthrombosis and inadequate perfusion. However, the question still remains if HBO is the explanation for the relatively low mortality rate in the present material.
The most common pathogens were of the Streptococcus milleri group mixed with anaerobic bacteria, with primary dental or pharyngeal focus. This finding is in line with the previous report by Fihman et al. [22], where Strep. milleri was cultured in 54 % of the patients. However, the Fihman report uses a wider definition of CNF, and therefore may include other types of deep neck infections. In our material, where such patients were excluded, 66 % (39/59) Strep. milleri must be regarded distinctive.
Clinical applicability
Surviving patients seemed to be hospitalized and given HBO treatment slightly faster than diseased patients (Table 2). These time difference was, however, not statistically significant, nor was it possible to identify any other parameter regarding age, gender, pre-morbidity or treatment, with importance for infection control or survival. Nevertheless, given the rapid and sometimes dramatic progress of the disease, early diagnosis must still be considered important in order to achieve prompt initiation of treatment.
Dose of HBO can be expressed in different ways, i.e., number of treatments, intensity of treatments (number of treatments per day, and week), treatment pressure, time at treatment pressure, total time in HBO chamber, all of which have a potential to influence the treatment dose given to the patient. In our study, the patients were not subjected to a strict HBO protocol [23, 24]. Instead, HBO dose was individualized according to patient response/infection control, as judged by senior clinicians. To make the individualization of the HBO dose clear, we recorded the total HBO dose (“atmospheric hours of oxygen”). A consistent terminology for HBO dose would be an important issue to consider in future treatment protocols.
Conclusions
Using a combined treatment with early surgical debridement combined with hyperbaric oxygen treatment (HBO), it is possible to reduce the mortality rate among patients suffering from CNF, compared to the expected mortality rate and to previous historical reports. Early onset of HBO treatment may be associated with an increased survival rate, but no clear factor was found to prognosticate outcome. Further studies are needed to clarify the effect of HBO treatment, as well as to investigate the pathological mechanisms behind the rapid and sometimes fatal spread of this type of bacterial infection.
References
Mao JC, Carron MA, Fountain KR, Stachler RJ, Yoo GH, Mathog RH, Coticchia JM (2009) Craniocervical necrotizing fasciitis with and without thoracic extension: management strategies and outcome. Am J Otolaryngol 30(1):17–23. doi:10.1016/j.amjoto.2007.12.007
Djupesland PG (2000) Necrotizing fascitis of the head and neck–report of three cases and review of the literature. Acta oto-laryngol Suppl 543:186–189
Jones J (1871) Investigation upon the nature, causes and treatment of hospital gangrene as it prevailed in the Confederate Armies Mission 1861–1865. Sanitary Commission, New York, p 1871
Wilson B (1952) Necrotizing fasciitis. Am Surg 18(4):416–431
Krenk L, Nielsen H, Christensen M (2007) Necrotizing fasciitis in the head and neck region: an analysis of standard treatment effectiveness. Eur Arch Otorhinolaryngol 264(8):917–922. doi:10.1007/s00405-007-0275-3
Fenton CC, Kertesz T, Baker G, Sandor GK (2004) Necrotizing fasciitis of the face: a rare but dangerous complication of dental infection. J Can Dent Assoc 70(9):611–615
Flanagan CE, Daramola OO, Maisel RH, Adkinson C, Odland RM (2009) Surgical debridement and adjunctive hyperbaric oxygen in cervical necrotizing fasciitis. Otolaryngol-Head Neck Surg: Off J Am Acad Otolaryngol-Head Neck Surg 140(5):730–734. doi:10.1016/j.otohns.2009.01.014
Sarna T, Sengupta T, Miloro M, Kolokythas A (2012) Cervical necrotizing fasciitis with descending mediastinitis: literature review and case report. J Oral Maxillofac Surg: Off J Am Assoc Oral Maxillofac Surg 70(6):1342–1350. doi:10.1016/j.joms.2011.05.007
Lanisnik B, Cizmarevic B (2010) Necrotizing fasciitis of the head and neck: 34 cases of a single institution experience. Eur Arch Otorhinolaryngol 267(3):415–421. doi:10.1007/s00405-009-1007-7
Wong CH, Wang YS (2005) The diagnosis of necrotizing fasciitis. Curr Opin Infect Dis 18(2):101–106
Langford FP, Moon RE, Stolp BW, Scher RL (1995) Treatment of cervical necrotizing fasciitis with hyperbaric oxygen therapy. Otolaryngol-Head Neck Surg: Off J Am Acad Otolaryngol-Head Neck Surg 112(2):274–278
Ord R, Coletti D (2009) Cervico-facial necrotizing fasciitis. Oral Dis 15(2):133–141. doi:10.1111/j.1601-0825.2008.01496.x
Maisel RH, Karlen R (1994) Cervical necrotizing fasciitis. The Laryngoscope 104(7):795–798. doi:10.1288/00005537-199407000-00003
Wolf H, Rusan M, Lambertsen K, Ovesen T (2010) Necrotizing fasciitis of the head and neck. Head Neck 32(12):1592–1596. doi:10.1002/hed.21367
Bahu SJ, Shibuya TY, Meleca RJ, Mathog RH, Yoo GH, Stachler RJ, Tyburski JG (2001) Craniocervical necrotizing fasciitis: an 11-Year experience. Otolaryngol–Head Neck Surg 125(3):245–252. doi:10.1067/mhn.2001.118182
Thakur JS, Verma N, Thakur A, Sharma DR, Mohindroo NK (2013) Necrotizing cervical fasciitis: prognosis based on a new grading system. Ear Nose Throat J 92(3):149–152
Young MH, Aronoff DM, Engleberg NC (2005) Necrotizing fasciitis: pathogenesis and treatment. Expert Rev Anti-infect Ther 3(2):279–294. doi:10.1586/14787210.3.2.279
Liddell FD (1984) Simple exact analysis of the standardised mortality ratio. J Epidemiol Community Health 38(1):85–88
Lin C, Yeh FL, Lin JT, Ma H, Hwang CH, Shen BH, Fang RH (2001) Necrotizing fasciitis of the head and neck: an analysis of 47 cases. Plast Reconstr Surg 107(7):1684–1693
Shindo ML, Nalbone VP, Dougherty WR (1997) Necrotizing fasciitis of the face. Laryngoscope 107(8):1071–1079
Lind F, Öhlen G, Lindén V, Eriksson BM, Forstell C (2011) Fokusrapport: Treatment with Hyperbaric Oxygen (HBO) at Karolinska University Hospital
Fihman V, Raskine L, Petitpas F, Mateo J, Kania R, Gravisse J, Resche-Rigon M, Farhat I, Bercot B, Payen D, Sanson-Le Pors MJ, Herman P, Mebazaa A (2008) Cervical necrotizing fasciitis: 8-years’ experience of microbiology. Eur J Clin Microbiol Infect Dis 27(8):691–695. doi:10.1007/s10096-008-0491-9
Harch PG (2009) The dosage of hyperbaric oxygen in chronic brain injury. http://www.hbot.com/article/dosage-hyperbaric-oxygen-chronic-brain-injury. Accessed 13 Mar 2016
Rogatsky GG, Shifrin EG, Mayevsky A (2003) Optimal dosing as a necessary condition for the efficacy of hyperbaric oxygen therapy in acute ischemic stroke: a critical review. Neurol Res 25(1):95–98. doi:10.1179/016164103101201003
Acknowledgments
The authors wish to thank Anna Westman and Bengt Gårdlund for valuable advice on microbiological aspects.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Author one to five declares that he/she has no conflict of interest.
Ethical approval
The study is approved by the Swedish Central Ethical Review Board (Dnr 2015/73-31/2). This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Elander, J., Nekludov, M., Larsson, A. et al. Cervical necrotizing fasciitis: descriptive, retrospective analysis of 59 cases treated at a single center. Eur Arch Otorhinolaryngol 273, 4461–4467 (2016). https://doi.org/10.1007/s00405-016-4126-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-016-4126-y