Abstract
A standard treatment procedure for necrotizing fasciitis in the head and neck region was introduced in 1999 at Rigshospitalet (National Hospital of Denmark) Copenhagen. The new procedure introduced more drastic surgical debridement than before, combined with a set antibiotic regime and intravenous gamma globulin and adjunctive hyperbaric oxygen treatment (HBO). To evaluate the effect of this, a retrospective study was undertaken, involving 19 patients treated for NF at the ENT department from 1996–2004. Between 1996 and 1999 eight patients were treated (non-HBO) from 1999–2004 eleven patients were treated (HBO group). Length of antibiotic treatment was very similar in the two groups (mean 22.5 days) as was bacteriology. Aetiological focus differed marginally with the HBO group showing a clear tendency towards odontogen focus. The HBO group was found to undergo significantly more debridement procedures (3.36). The most drastic difference in the two groups however, was the reduction in mortality. The non-HBO group had a mortality of 75% and in the HBO group they all survived. This obviously resulted in a prolonged hospital stay for the HBO group (mean 30.8 days). The study concluded that the reduction in mortality was due to the combined effects of the different entities in the new treatment guidelines. It was not possible to isolate a specific factor responsible for the change.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Necrotizing fasciitis (NF) was first described in 1871 by Joseph Jones, an army surgeon, who encountered the infection during the American Civil War. NF is the preferred term because fascial necrosis is the most consistent manifestation of the disease, which includes a wide variety of syndromes [1–4]. In 1952, Wilson et al. [1] found this infection to be primarily caused by staphylococci species. However, since then, it is widely used to describe an acute infection of the superficial fascia and surrounding soft tissue, often polymicrobial and including streptococci and anaerobes in synergistic coexistence [1–7]. The symptoms develop acutely and quick diagnosis is of crucial importance to reduce mortality and morbidity [8–10]. The progression of the disease is classically divided into three stages. Initially the primary symptom is a patchy erythema often mistaken for cellulites or erysipelas. The skin lesion does not correspond with the true extent of subcutaneous involvement. Often the patients experience tenderness of the area and a run fever. The infection quickly spreads and in the second phase the patient suffers from severe pain of the affected area and bullae often develop. Systemic symptoms get more severe with typical signs of septicaemia. The last stage of the disease is characterized by cyanotic skin discoloration typical of necrosis. The pathogenesis behind this necrotic development is thought to be endarteritis obliterans in the nutrient vessels going through the fascia. On palpitation there can be marked crepitation of the soft tissue due to subcutaneous bacterial gas production. The patient gradually goes into septic shock and multi organ failure (MOF) [2, 5, 7, 8, 11–13]. The continuous problem with early diagnosis is due to the paucity of specific clinical signs during the early progression of the disease [3, 8].
The total number of NF in Denmark has been reported to be 25–50 per year (in a population of about 5 million) in the head and neck region the incidence is 5–10. The total number of recorded cervical and craniofacial NF cases in the literature includes about 200 patients [14]. NF in the head and neck region has different characteristics depending on location. Cervical NF dominates among males and has a higher mortality and is more often polybacterial than infection originating from the craniofacial region [4, 15].
The quick spread of infection and vast bacterial load cause devastating consequences for the patients and the literature reports extremely high mortality and morbidity. To reduce this, a guideline to standardize treatment was implemented in 1999 at the department of Otolaryngology-head and neck surgery at Rigshospitalet (National Hospital in Denmark). This standard procedure includes primary extensive surgical debridement, intensive antibiotic and intravenous gamma globulin treatmentFootnote 1. and hyperbaric oxygen treatment (HBO).
Theoretically HBO and intravenous gamma globulins should reduce the bacterial proliferation and spread and therefore also reduce necrotic development. The use of HBO in treating NF is controversial [16]. Theoretically HBO treatment increases polymorphonuclear cell function, further fibroblast proliferation and collagen production. Furthermore, hyperbaric oxygen is directly bactericidal on anaerobes [3, 17, 18]. All these factors combined improve healing and are thought to diminish the volume of debrided tissue.
The aim of the present study is to evaluate the new treatment by comparing the modalities before and after 1999. In this evaluation it has not been possible to separate the different entities in the new procedure. It is therefore the combined effect that has been analyzed.
Materials and methods
From 1996–2004, 19 patients were treated for NF at the Head and Neck and Otolaryngology Surgical Department at Rigshospitalet [19]. All patient records were reviewed retrospectively and two groups were identified; the non-HBO group (n = 8) before the new guideline with HBO as adjunctive therapy, and the HBO group (n = 11) after the new guideline. Host factors including age, sex, aetiological focus, bacteriology and co-morbidity were analyzed. Length of hospital stay, duration of antibiotic treatment, number of surgical procedures and mortality were also evaluated. For the purpose of this study, operations were classified as: Debridement, describing necrotic tissue removal until clearly vital tissue was reached, or incision and drainage (I&D), describing only wound inspection and drainage. An estimate of the clinical status on arrival, pathology findings and surface area debrided proved to be unmanageable due to incomplete data.
The HBO protocol for necrotizing fasciitis involved administering hyperbaric oxygen at 2.8 atmospheres pressure for 90 min in a multiplace chamber (Drass Gallazzi Sp.A). Patients received HBO treatment as an adjunct therapy three times within the first 24 h after admission, and then twice during the following days. This protocol was followed until there was no on-going evidence of necrosis.
The results were tested for significance using Wilcoxon’s test, t-test for independent data, Binomial test and Fisher’s exact test. A P-value less than 0.05 was considered significant.
Results
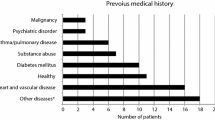
Host factors like age, sex, co-morbidity, etiological focus and bacteriology are illustrated in Tables 1, 2, 3 and 4. Age and sex were very similar in the two groups. Co-morbidity differed marginally. In the HBO groups there were significantly more patients with diabetes and smoking. In the non-HBO group significantly more patients with a substantial alcohol abuseFootnote 2.
Wound and blood bacteriology showed a tendency towards streptococcal species and generally a polybacterial colonisation.
The duration of antibiotic treatment was not significantly different in the two groups, i.e., 23.3 days in the HBO group and 21.1 days in the non-HBO group. However, there was an obvious variation in the initial choice of antibiotics due to change in protocol. Antibiotic treatment was adjusted according to the sensitivity of cultured organisms.
The HBO group underwent a total of 88 surgical procedures (mean 8.0) and the non-HBO only a total of 20 (mean 2.5). The HBO group underwent significantly more operations of the debridement type than the non-HBO patients (P < 0.002), while the number of I&D in the two groups were similar (0.05 < P < 0.1). In the HBO group the mean for debridements was 3.36 versus 0.5, and I&D 4.63 versus 2.13, respectively. Reconstructive surgery was also performed. However, this was only the case in the HBO patients where seven patients underwent reconstructive surgery.
HBO treatment followed a specific protocol and the patients had a mean of six dives. Sixty four percent of the patients had five or less. No patient received more than 11 dives. In this analysis only dives where necrotizing fasciitis was the indication for treatment were included. One patient developed osteomyolitis of the jaw and underwent HBO treatment on a regular basis for a 2-month period after his soft tissue infection had resolved. This patient’s data was not included in the evaluation of HBO treatment.
Mortality was vastly reduced from 75% in the non-HBO group to zero in the HBO group (P < 0.001). This reflected directly on the length of hospital stay. Resulting in a mean duration of 30.8 days in the HBO treated patients versus 15.3 days in the non-HBO group (P < 0.02). The cause of death in the non-HBO groups was mainly due to progressive multi-organ failure. In both groups the complications typically included sepsis with haemodynamic instability and adult respiratory distress syndrome.
Discussion
In treating this group of patients, physicians were left with the impression that the patients were more susceptible to infection and compromised healing due to vascular disease and general immunodeficiency. Diabetes and smoking combined with excessive alcohol intake or intravenous drug abuse was the most common co-morbidity. Even though only few of the evaluated co-morbidity factors were significantly more frequent in our patients than the population in general, Table 2 shows a marked tendency to substantiate the initial impression. Systemic disease is thought to be a contributing but not necessary factor for NF to develop in these patients [4, 5, 8, 9, 11].
Duration of antibiotic therapy was reported to be marginally longer in this study than what is usually reported in the literature [9, 21], with no significant difference between the two groups. However, in our study the duration of antibiotic treatment was very varied, and it gives no clear impression of the optimal length of antimicrobial therapy. Antibiotics were combined with intravenous immunoglobulin, especially in the HBO group where 9/11 patients received immunoglobulin for a total of three days. The rationale behind this adjuvant antimicrobial therapy is to reduce bacterial spread and inflammation in the soft tissue by inhibition of superantigen activity reducing septicaemia and fluid sequestration [8, 22, 23]. The simultaneous use of several different broadspectrum antibiotics illustrates the different resistance profile and variation in bacterial species cultured from these patients. McMahon et al. [8] found the oropharynx and oral cavity to be the aetiological focus of cervical NF. This finding correlates well with our findings. However, none of the patients in the non-HBO group showed odontogen infection focus, differing clearly from the findings of Maisel and Karlen, who found the majority of cervical NF to be of odontogen focus just like the HBO group. This difference in focus can not be readily explained. However, it has been suggested that NF in the head and neck region can not be considered as one entity but must be divided into cervical and craniofacial NF [4, 15]. Cervical and craniofacial NF differ in two main aspects. Cervical NF has a higher mortality, and it is more often caused by multiple bacterial species, both anaerobes and aerobes [15]. Due to the limited number of patients in this study it was decided not to subdivide NF in the head and neck region further.
Our study differentiated surgical procedures according to removal of necrotic tissue or simple drainage. Our findings clearly showed that the HBO group underwent significantly more surgical debridement procedures than the non-HBO patients, with a mean of 3.36 versus 0.5. This differed drastically from Risemann et al. [10] who found a marked reduction in the need for debridement in the HBO treated group. Risemann et al. [10] found a need for debridement in HBO group to be less than half of the non-HBO group (1.6 and 3.25, respectively). Their findings contrast directly with the two-fold increase in debridements in the HBO group found by Brown et al. [21] in 1994 when reviewing 54 cases of truncal NF. Our study correlates well with the findings of Brown et al. [21] with a mean of 2.4 and 1.3 in the HBO and non-HBO patients, respectively. Several factors are relevant in analyzing these results. First of all the patient populations differ in respect to aetiological focus. Riseman et al. looked at NF in the extremities and Brown et al. [21] reviewed truncal infections and our study only included cervical and craniofacial NF. Different aetiology could have an effect on surgical control of the infection. Furthermore, in Riseman and Browns studies a distinct differentiation between different types of surgical procedures has not been clearly described and this could account for some of the discrepancy between the results. We made a clear distinction between debridement and I&D, as previously described; this makes direct comparison difficult. The drastic reduction in mortality could also play a part in explaining the need for more surgical procedures in the HBO treated group. Increase in surgical debridement in the HBO group left the patients with greater soft tissue defects, and hence a greater need for reconstructive surgery. The need for a functional and cosmetically acceptable end result was also enhanced in this patient group (see Figs. 1, 2 and 3).
The literature generally reports mortality rates between 6 and 76% with NF. This correlates well with the mortality of 75% in the non-HBO group. In the HBO group all the patients survived their infection. This drastic reduction in mortality between the two groups must be due to the specific treatment procedure, aiding the admitting doctor in diagnosing and initiating rapid treatment of this acute infection. McMahon et al. [5] and Balcerak et al. [8] both found quick diagnosis and surgical debridement to be very important factors in reducing mortality.
Conclusion and perspectives
In the present study it has not been possible to differentiate the entities in the new guideline, and the revolutionary survival in the HBO group must be a result of the combined effect of quick and major debridement, broad-spectrum antibiotic treatment, intravenous gamma globulins and HBO treatment. This drastically changes the prognosis for patients with necrotizing fasciitis.
In the future it would be interesting to evaluate if the volume of soft tissue removed could be lessened making the need for reconstructive surgery smaller and more achievable, leaving the patients with an even better result than today. HBO effectiveness has not been tried in randomized trials. This would be advisable, though probably unlikely due to the very small number of patients with this infection. Also the question of human ethics should be considered after finding such a marked difference in mortality.
Since the conclusion of this study 14 cases of NF in the head and neck region have been identified and treated as our HBO group. All have survived. There has been a slight increase in the incidence of NF, probably due to increased awareness. In future studies it would be interesting to look at patient status on arrival, including blood count, temperature, blood pressure and a standardized measure of tissue involvement. This would make it possible to evaluate possible prognostic factors for development of septic shock and also give an idea of the possible effect of HBO and immunoglobulin in reducing tissue volume removed.
Notes
Consist of Meronem 2 g bolus followed by 1 g three times daily, Ciproxin 400 mg twice daily, Dalacin 600 mg three times daily. Gammaglobulin is 25 g once a day for 3 days. All given intravenously
Defined according to the Board of National Health in Denmark, to be more than 14 U per week for women and more than 21 U per week for men.
References
Wilson B (1952) Necrotizing fasciitis. Am Surg 416–431
Lin C, Yeh F-L, Lin J-T et al (2001) Necrotizing fasciitis of the head and neck. Plast Reconstr Surg 107:1684–1693
Lepawsky M (2003) Necrotizing soft tissue infections. Hyperbaric Oxygen Committee Report 69–78
Djupesland P (2000) Necrotizing fasciitis of the head and neck. Acta Otolaryngol 543:186–189
Balcerak RJ, Sisto JM, Bosack RC (1988) Cervicofacial necrotizing fasciitis. J Oral Maxillofac Surg 46:450–459
Maisel RH, Karlen R (1994) Cervical necrotizing fasciitis. Laryngoscope 104:795–798
Wong C, Wang Y (2005) The diagnosis of necrotizing fasciitis. Curr Opin Infect Dis 18:101–106
McMahon J, Lowe T, Koppel DA (2003) Necrotizing soft tissue infections of the head and neck. Oral Surg Oral Med Oral Pathol Oral Radio Endod 95:30–37
Elliot DC, Kufera MA, Myers RAM (1996) Necrotizing soft tissue infections. Ann Surg 224:672–683
Risemann JA, Zamboni WA, Curtis A et al (1990) Hyperbaric oxygen therapy for necrotizing fasciitis reduces mortality and the need for debridements. Surgery 108:847–850
Seal DV (2001) Necrotizing fasciitis. Curr Opin Infect Dis 14:127–132
Bisno AL, Stevens DL (1996) Streptococcal infections of skin and soft tissues. New Eng J Med 334:240–245
McGee EJ (2005) Necrotizing fasciitis: review of pathophysiology, diagnosis and treatment. Crit Care Nurs Q 28:80–84
Marioni G, Rinaldi R, Ottaviano G et al (2006) Cervical necrotizing fasciitis. J Infect 53:219–222
Banerjee AR, Murty GE, Moir AA (1996) Cervical necrotizing fasciitis. J Laryngol Otol 11:81–86
Jallali N, Withey S, Butler PE (2005) Hyperbaric oxygen as an adjuvant therapy in the management of necrotizing fasciitis. Am J Surg 189:462–466
Kang TS, Gorti GK, Quan SY et al (2004) Effect of hyperbaric oxygen on the growth factor profile of fibroblasts. Arch Facial Plast Surg 6:31–35
Tibbles PM, Edelsberg JS (1996) Hyperbaric oxygen therapy. New Eng J Med 334:1642–47
Nielsen HUK, Rasmussen N (2000) Nekrotiserende Fasciitis: Et tiltagende alvorligt problem. Ugeskr Læger 162:1745–1747
http://www.si-folkesundhed.dk/susy 31 December 2006
Brown DR, Noelle LD, Lepawsky M et al (1994) A multicenter review of the treatment of major truncal necrotizing infections with and without hyperbaric oxygen therapy. Am J Surg 167:485–489
Norby-Teglund A, Muller MP, McGeer A et al (2005) Succesfull management of severe group A streptococcal soft tissue infections using aggressive medical regimen including intravenous polyspecific immunoglobulin together with conservative surgical approach. Scand J Infect Dis 37:166–172
Norby-Teglund A, Ihendyane N, Darenberg J (2003) Intravenous immunoglobulin adjunctive therapy in sepsis, with special emphasis on severe invasive group A streptoccocal infections. Scand J Infect Dis 35:683–689
Acknowledgments
The authors would like to thank The Biostatistical Department of University of Copenhagen for assistance in statistical testing. Furthermore, we would like to thank associate professor Erik Jansen from the Anaesthesiology and Pressure Chamber Department, associate professor Jacob S. Andersen from the intensive care unit and associate professor Niels Rasmussen from the department of Otolaryngology-head and neck surgery at Rigshospitalet for their valuable help in the completion of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Krenk, L., Nielsen, H.U. & Christensen, M.E. Necrotizing fasciitis in the head and neck region: an analysis of standard treatment effectiveness. Eur Arch Otorhinolaryngol 264, 917–922 (2007). https://doi.org/10.1007/s00405-007-0275-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-007-0275-3