Abstract
The efficiency of titanium middle ear prosthesis for ossicular reconstruction in chronic ear disease is investigated in a Scandinavian two-center retrospective study from a Norwegian tertiary otology referral center and a Finnish otology referral center. Retrospective chart reviews were performed for procedures involving 73 titanium prostheses between 1999 and 2004. All patients that underwent surgery including the Kurz Vario titanium prosthesis were included in the study, 38 procedures including the partial ossicular replacement prosthesis (PORP) and 35 procedures including the total ossicular replacement prosthesis (TORP). Mean follow-up was 14 months. The ossiculoplasty was performed alone (29 patients) or in combination with other chronic ear surgery procedures (34 patients). Comparisons of preoperative and postoperative pure tone averages (0.5, 1, 2, and 3 kHz) according to AAO-HNS guidelines are presented, as well as data for different PTA definitions. Otosurgery procedures, complications, revisions, and extrusion rates are reported. A postoperative air-bone gap (ABG) of ≤20 dB was obtained in 77% of the patients, 89% for the Bell (Porp) prosthesis, and 63% for the Arial (Torp) prosthesis. Overall mean pure tone averages improved 20.6 dB with ABG improvement of 19.3 dB. The overall extrusion rate was 5% (4 patients). Titanium prostheses have been easy and fast to handle and effective implants for reconstruction of the ossicular chain. We found no difference between reconstruction with or without cholesteatoma surgery during the same procedure. The combination of CWD and Torp gave significant inferior hearing thresholds as compared to Torp/CWU and Porp/CWD combinations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The middle ear ossicles are the key to a functional middle ear. Ossicular reconstruction has always been a challenge for the otosurgeon. More than half of chronic middle ear diseases are reported to have ossicular involvement [1]. There are a variety of materials to choose from when performing ossicular reconstruction, including autogenous tissues and alloplasts.
Implant design, stability, ease of use, and functional results are all accounted for in prosthesis selection. The limitations of ossiculoplasty are well known, most distressing are extrusions and the long-term deterioration in functional result. Of all available materials, hydroxyapatite (HA) is the most commonly used in recent years [2]. Long-term studies for HA alloplasts have been reported with an extrusion rate of 5–15% [3, 4]. Present evidence indicates that titanium has a greater ability to transmit sound than the heavier HA [5], and titanium is known for its biocompatibility in orthopedic and orthodontic surgery [6].
The use of titanium ossicular prosthesis was first reported by Stupp et al. in 1999 [7], and later reports have shown success rates (ABG ≤ 20 dB) ranging between 57 and 76% [8–11]. We report our results with a total of 73 implants. Comparison of preoperatively and postoperatively pure tone averages and air-bone gaps (ABGs) was performed at frequencies recommended by AAO-HNC [12]. For easy comparison to other studies we have also included data with different PTA calculations, as well as a selection of patients with a recommended follow-up of more than 12 months.
Materials and methods
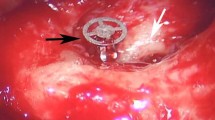
Kurz (Kurz GmbH, DuBlingen, Germany) titanium total ossicular replacement prostheses (Torp, Aerial) and partial ossicular replacement prostheses (Porp, Bell) with adjustable lengths were used in all procedures. All surgery procedures with titanium prosthesis from the start in 1999 until March 2004 are included in the report. The data include 71 patients and 73 surgical procedures. One patient was operated on both ears. The other patient with two procedures needed a revision of the prosthesis due to bad contact on the stapes. The first operation on this patient is included in the data as an implant with unsuccessful hearing result.
The surgery was performed initially by JS and FSV in cooperation (nine procedures, JS as the senior surgeon), 42 procedures were then performed by FSV in Bergen, Haukeland University Hospital, Norway, and 22 by JS in Lahti, Päijät-Häme Central Hospital, Finland. All charts were analyzed in an otosurgical database. Tragal cartilage was interposed between the prosthesis and the tympanic membrane in all cases. The Porp prosthesis was never placed under the malleus, but was positioned in the upper posterior quadrant as for the Torp. In some cases, the Porp prosthesis was bend about 15–20° to parallel the top of the prosthesis to the plane of the tympanic membrane.
Preoperative audiograms with bone and air conduction were obtained the day before surgery. The most recent available postoperative audiograms were reviewed. Pure tone air frequencies at 0.5, 1, 2, and 3 kHz, as recommended by AAO-HNS, were used in the PTA calculations. In addition, other calculations including PTA (0.5, 1, and 2 kHz) and PTA (0.5,1, 2, and 4 kHz) were done for comparison, as indicated in the figures and tables. A postoperative ABG of 20 dB or less was considered a successful hearing result. Statistical analyses were done by paired (pre and postoperative data) and independent (between different operations) Student’s t tests. ANOVA tests were performed for multigroup analyses. High frequency pure tone bone conduction average (HPTBC) was calculated for 1, 2, and 4 kHz to measure postoperative sensorineural hearing loss (AAO-HNS). Mean change in HPTBC was 1.1 dB ± 5.4 (SD), two patients had a loss of >10 dB (HPTBC change of −13 and −16 dB). AAO-HNS recommends at least 1-year follow-up for evaluation of hearing results. The data was therefore also analyzed with regard to the recommended follow-up time. The data is separated in different groups according to type of prosthesis (Porp/Torp), length of follow-up, type of chronic ear disease, and amount of mastoid surgery.
Results
The main characteristics of the patient material and results are given in Table 1.
Hearing results
The mean overall hearing results are shown in Tables 2 and 3. PTA improved from preoperative 50 to 30 dB, whereas the ABG improved from 33 to 14 dB. We have also included different PTA values in the calculations for easier comparison with other studies. Data from patients with follow-up for at least 12 months as suggested by the AAO-HNS were also analyzed. As shown in Table 2, we found no decrease in the hearing results after 12 months compared to the overall material.
The ABGs in 10 dB cumulative increments are shown in Table 4. We found that 76% of the patients had an ABG of 20 dB or less, 63% for the Torp prostheses and 89% for the Porp. Similar results were also obtained with PTA calculations using the average of 0, 5, 1, and 2 kHz and 0.5, 1, 2, and 4 kHz (Table 4).
Procedures and diagnoses
Hearing results with respect to surgical procedure are shown in Table 5. The ABG ≤ 20 dB score from primary ossiculoplasty operations was 20% higher than the results from revisions. The 19 revision operations included mainly earlier unsuccessful ossiculoplasty operations with autological incus, or prior cholesteatoma operations without ossiculoplasty. We could not find any difference between the revision CWU and CWD group.
The material was also separated with respect to diagnosis (Table 6). Forty procedures included removal of cholesteatoma at the same time as the titanium implantation (Tables 5, 6). Interestingly, we found that the hearing result for both the cholesteatoma and noncholesteatoma groups and the CWD and CWU groups showed only variation within 10% in success rate. Earlier studies have indicated that Torp prosthesis or the absence of the posterior canal wall may correlate to a significant decrease in success rate [8–11]. We therefore investigated the relationship between the prosthesis type and the posterior canal wall (Tables 7, 8). We found that subgroups of both Torp and CWD patients gave good results. A significant decrease in the hearing results was found only with the combination of Torp and CWD (Table 8). The Porp gave good hearing results despite canal wall down procedures, whereas the Torp prosthesis gave good results in CWU surgery.
Complications
Four patients had an extrusion of the prosthesis (5%) and these are included in the material as procedures with unsuccessful hearing results. All these patients developed an atelectatic middle ear and two needed revision surgery with myringoplasty, a new implant was not given. Two patients had a postoperative infection with otorrhea, one of these had an implant extrusion and is mentioned above. Four patients with Torp prosthesis need treatment with ventilation tube, the hearing results are successful. Two patients had a postoperative sensorineural hearing loss of 13 and 16 dB, as measured by HPTBC (see Materials and methods).
Discussion
Studies with the Kurz Porp and Torp prosthesis have reported successful hearing results (ABG ≤ 20dB) ranging between 57 and 76% [8–11]. We report a success rate of 77%. Every surgery with titanium prosthesis is included in the calculation to avoid masking of failures by revision operations. All studies including ours have found better results with Porp compared to the Torp prosthesis. Most of the published data have not used the AAO-HNS recommended follow-up and/or frequencies for ABG calculation. We have included different PTA calculations for easier comparison to other studies. As expected, the 0.5, 1, 2 kHz PTA and the 0.5, 1, 2, 4 kHz PTA calculations gave a minor increase and decrease in success rate, respectively. We found no difference between patients with a follow-up of more or less than 12 months, as recommended by AAO-HNS.
Our surgical procedures were mainly a mixture between primary or revision ossiculoplasty and cholesteatoma surgery with titanium reconstruction in the same procedure. As shown in Table 5, we found the same success rate in the ossiculoplasty group and the cholesteatoma group. Thus, the titanium implants seem to be well suited for one-stage cholesteatoma surgery.
Compared to canal wall up procedures and the use of Porp prostheses, both the canal wall down situation and the Torp prosthesis have been reported to associate with lower rates of success. Interestingly, we found that the Torp prosthesis and canal wall down by themselves did not give lower success (Tables 7, 8). However, the combination of the two factors gave approximately a 50% significant reduction in success rate. The preservation of the posterior canal wall and the stapes suprastructure are both factors in our material that promote stability for the middle ear prosthesis. We assume that the existence of one of these two factors is sufficient for good hearing results. The reported difference between the titanium Porp and Torp may be explained by the fact that Torp prostheses are more frequently used in canal wall down surgery.
As shown in earlier reports, atelectasis of the tympanic membrane is a major reason for poor hearing results after tympanoplasty, especially for children [13]. Estimation of the future middle ear ventilation of the patient before surgery is a challenge for the otosurgeon. Selection of the right patient to offer an implant may be as important as the correct surgical technique. Patients with severe retraction pockets or atelectasis of the pars tensa were not given an implant during primary surgery. Eighteen of our patients were under 16 years of age at the time of operation. Only 2 (11%) of them have developed retraction and atelectasis of the tympanic membrane. The corresponding figure for adults is 9% (4/44), which matches the figures presented for adults [13]. We have paid extra attention to postoperative tympanic ventilation and four patients are treated with ventilation tubes.
We conclude that the Kurz titanium middle ear implants are well suited for ossiculoplasty. They are easy to handle and give excellent hearing results, both compared to autograft [14] and other alloplastic materials [15]. The Torp prosthesis in our material is associated with lower success rate for patients with canal wall down surgery.
References
Chole RA (1999) Ossiculoplasty with banked cartilage. Otolaryngol Clin N Am 27:717–726
Goldenberg RA, Emmet JR (2001) Current use of implants in middle ear surgery. Otol Neurotol 22:145–152
Shinohara T, Gyo K, Saiki T (2000) Ossiculoplast using hydroxyapatite prosthesis: long-term results. Clin Otolaryngol 25:287–292
Goldenberg RA, Driver M (2000) Long-term results with hydroxyapatite middle ear implants. Otolaryngol Head Neck Surg 112:635–642
Meister H, Walger M, Mickenhagen A, von Wedel H, Stennert E (1999) Standardized measurements of the sound transmission of middle ear implants using a mechanical middle ear model. Eur Arch Otorhinolaryngol 256:122–127
Williams D (2001) The golden anniversary of titanium biomaterials. Med Device Technol 12:8–11
Stupp CH, Dalchow C, Grun D, Stupp HF, Wustrow J (1999) Three years of experience of titanium implants in the middle ear. Laryngorhinootologie 178:299–303
Wang X, Song J, Wang H (1999) Results of tympanoplasty with titanium implants. Otolaryngol Head Neck Surg 121:606–609
Krueger WW, Feghali JG, Shelton C, Green JD, Beatty CW, Wilson DF, Thedinger BS, Barrs DM, McElveen JT (2002) Preliminary ossiculoplasty results using the Kurz titanium prostheses. Otol Neurotol 23:836–839
Ho SY, Battista RA, Wiet RJ (2003) Early results with titanium ossicular implants. Otol Neurotol 24:149–152
Martin AD, Hardner SG (2004) Ossicular reconstruction with titanium prosthesis. Laryngoscope 114:61–64
Committee on Hearing Equilibrum (1995) Guiedelines for the evaluation of results of treatment of a conductive hearing loss. Otolaryngol Head Neck Surg 113:186–187
Silvola J, Palva T (1999) Long-term results of pediatric primary one-stage cholesteatoma surgery. Int J Pediatr Otorhinolaryngol 148:101–107
O’Reilly RC, Cass SP, Hirsch BE, Kamerer DB, Bernat RA, Poznanovic SP (2005) Ossiculoplasty using incus interposition: hearing results and analysis of the middle ear risk index. Otol Neurotol 26:853–858
Yung MW (2003) Literature review of alloplastic materials in ossiculoplasty. J Laryngol Otol 117:431–436
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vassbotn, F.S., Møller, P. & Silvola, J. Short-term results using Kurz titanium ossicular implants. Eur Arch Otorhinolaryngol 264, 21–25 (2007). https://doi.org/10.1007/s00405-006-0149-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-006-0149-0