Abstract
Ossicular defects due to chronic ear disease are common and continuous problem for otologic surgeon. Ossicular reconstruction prostheses are widely used to restore ossicular continuity when the incus is eroded or missing, for example, in chronic otitis media or cholesteatoma. In this regard; the total and partial ossicular replacement prosthesis (TORP and PORP) have been enthusiastically endorsed. Traditionally, either PORP or TORP is applicable, depending primarily on whether there is an intact stapes superstructure or only a stapes footplate. Laser interferometer studies on the mechanics of the reconstructed human middle ear have shown that, from a mechanical viewpoint, the malleus to footplate type of reconstruction gives a more favourable result compared with a malleus to stapes superstructure reconstruction even in presence of intact stapes suprastructure. However, it is still unclear whether ossicular reconstruction has a better long-term outcome with PORP or TORP in the presence of stapes suprastructure. A prospective randomised trial of 60 patients with Austin type A defects divided into two groups was conducted. In one group TORP was used and in other group PORP. Outcomes were studied in terms of hearing gain, AB gap closure and stability of the prosthesis. Preoperative PTA of Moderate Conductive Hearing loss (40–55 db) was most found followed by severe conductive hearing loss (> 55 db) with standard deviation of 7.155 and mean hearing loss was 46.30 db in TORP group. In this group post operative pure tone averages improved to mild hearing loss (26–30 db) in about 90 percent of patients with mean of 32 db and standard deviation of 7.06. Preoperative PTA of severe Conductive Hearing loss (> 55 db) was most found followed by moderate Conductive Hearing loss (45–55 db) with standard deviation of 6.471 and mean hearing loss was 47 db in PORP group. Post operative Pure Tone averages improved to Mild Hearing loss (26–30 db) in about 90 percent of patients with mean of 33 db and standard deviation of 5.431 in PORP group. ABG reduction in TORP group was 22.603 ± 12.34 while in PORP group was17.79 ± 10.743. Hearing gain and ABG closure is almost comparable with both TORP and PORP, however because of increased stability of TORP we recommend TORP for better long-term outcomes in Austin type A ossicular defects.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
An adequate auditory function is important for acquiring knowledge and enhancing the productivity of human beings. World Health Organization (WHO) estimates that, there are about 63 million people in India are experiencing significant auditory impairment [1]. Causes of hearing loss may stem from either a conductive or sensorineural component. Almost all conductive causes of hearing loss have a surgical option for complete cure. Despite recent advances in public health and medical care, it continues to be prevalent. According to WHO, chronic suppurative otitis media is considered as the most common cause of persistent mild to moderate conductive hearing impairment among children and young people in developing countries.
WHO has indicated that a prevalence rate of chronic suppurative otitis media(CSOM) greater than 4% in a defined population is suggestive of a substantial public health concern demanding immediate attention, while, India, has a noteworthy prevalence rate of 7.8%, which further highlights the need for effective treatment strategies [2]. CSOM is a chronic condition which has infectious etiopathogenesis. Among the two types of CSOM, tubotympanic and atticoantral, the former is characterised by central perforation in the pars tensa surrounded by residual tympanic membrane and the latter involves posterosuperior part of middle ear cleft. Erosion of the incudostapedial joint with intact malleus is the most common ossicular defect encountered in both tubotympanic and atticoantral type of Chronic Otitis Media. Austin estimated that malleus and stapes suprastructure are intact in about 60% cases [1]. Pure tone audiogram usually shows a hearing impairment of more than 40 dB in patients with ossicular erosion.
Therefore, the focus is towards attaining a near normal neo membrane with continuous ossicular chain and a postoperative middle ear status which functionally bears close resemblance to the normal state. Hence, the surgical goals for chronic ear disease include eradication of the disease and reconstruction of the sound conduction mechanism. Numerous ossiculoplasty techniques have been used to reconstruct the ossicular chain. A major challenge in the surgical management of conductive hearing loss, from an acoustic standpoint, is the improvement of hearing [3]. However, from a surgical standpoint, hearing outcomes are highly variable and determined by many factors, both internal and external, including ossicular chain reconstruction.
All ossicular reconstructions can be generally divided into two types of models: Partial Ossicular Replacement Prosthesis (PORP) and Total Ossicular Replacement Prosthesis (TORP).Traditionally, either PORP or TORP is applicable, depending primarily on whether there is an intact stapes superstructure or only a stapes footplate [4]. Although, the existing literature underscores the clinical significance of ossicular reconstructions in restoring sound conduction mechanisms, but a definitive consensus on the superiority of PORP or TORP in terms of long term stability and more favourable hearing outcomes, still remains elusive. Several clinical investigations show that reconstruction with PORP leads to better hearing than TORP. Conversely, there are studies that show ossicular reconstructions to the stapes footplate with TORP result in significantly better hearing outcomes than the reconstructions to the stapes superstructure with PORP. In addition, some investigations suggest that there is no significant difference between the two models [1]. In light of the current discrepancy of conclusive evidence, our research aims to address this lacuna and divulge into the nuances of ossicular reconstruction through a meticulous examination of the outcomes associated with both PORP and TORP in patients diagnosed with Chronic Otitis Media. Our study seeks to not only uncover the nuances of ossicular reconstructions in the context of CSOM but also to provide clarity on the long-debated question of whether PORP or TORP offers a more favourable outcome. By doing so, we aspire to contribute meaningful insights that extend beyond the confines of our study, addressing the larger question of how to best manage and alleviate the burden of chronic ear diseases on global auditory health.
Material and Methods
This study was carried out in the Department of ENT and Head Neck, Sri Guru Ram Das University of Health Sciences, Amritsar.
Study Period
January 2018–January 2023.
Study Design
Prospective randomised comparative cohort study of patients undergoing ossiculoplasty in our hospital.
Study Population
Patients who attended the ENT outpatient department at SGRDUHS hospital with chronic otitis media and ossicular erosion.
Sample Size
60.
Classification Used
Austin’s classification of ossicular defects as modified by Kartush was used to define the ossicular status encountered [5]. In this analysis, those patients allocated to Austin Kartush type A ossicular defect (stapes and malleus present) were selected for PORP and TORP implantation from the malleus to stapes head or footplate depending upon the group allocated.
Financial support
It was a non-funded study.
Inclusion Criteria
-
Age between 10 and 70 years.
-
Tubotympanic type of CSOM with pure conductive hearing loss on Pure tone audiometry more than or equal to 40 db
-
Intact suprastructure of stapes and intact malleus with erosion of incus
-
Good Eustachian tube function evidenced by diagnostic nasal endoscopy
-
No other external ear, middle ear or inner ear pathology.
Exclusion Criteria
-
(1)
Complicated CSOM
-
(2)
Atticoantral type of CSOM
-
(3)
Mixed hearing loss
-
(4)
Stapes fixation
-
(5)
Only hearing ear
-
(6)
History of previous ear surgery.
-
(7)
Unhealthy or polypoidal middle ear mucosa
-
(8)
Congenital ear anomalies
-
(9)
Patient not reporting for follow up
-
(10)
Pregnant and lactating mother
-
(11)
Uncontrolled systemic diseases which affect the healing process.
After eliciting the complaints and history of the patients included in the study, they were subjected to detailed clinical examination of the ear, nose and throat. The size, site of perforation, status of middle ear mucosa and ossicles was examined using otoscope and the findings were documented. Clinical findings were confirmed by oto-endoscopic examination. Tuning fork tests were done using 256 Hz, 512 Hz and 1024 Hz tuning fork and findings recorded. The patients were subjected to pure tone audiometry, and graphical recordings of their hearing thresholds were made. Pure tone averages and air bone gap were calculated. Diagnostic nasal endoscopy was done to rule out nasal and nasopharyngeal foci of infection and to assess the pharyngeal end of the Eustachian tube. High resolution Computed tomography (HRCT) temporal bone was done before surgery to know about status of middle ear, integrity of ossicular chain,to rule out cholesteatoma and congenital anomalies. Systemic examination and investigations were done to assess fitness for surgery. All patients underwent examination under microscope and the ossicular status was determined. The ossicular status on EUM was considered gold standard assessment.Patients were sequentially allocated into two groups; Group A; the patients underwent TORP ossiculoplasty and Group B underwent PORP ossciuloplasty.
Surgical Technique
The following equipment was used.
-
Operating microscope: CARL ZIESS OPMI VARIO S88
-
Ossicle holder
-
Microdrill: MEDTRONIC
-
Otologic instrumentation tray
-
Ossicular prosthesis: PORP ( KURZ) & TORP ( GRACE MEDICAL)
Preparation
All cases were performed in the setting of general anaesthesia.
The ear was prepped and draped in a sterile fashion. After area preparation, sterile draping and local infiltration with 2% lignocaine and 1 in 200,000 adrenaline given in post auricular, endaural area and external auditory canal to promote haemostasis. This was done under direct visualization of the operating microscope to precisely deliver the injection into the ear canal at the bony-cartilaginous junction in the subperiosteal plane to result in a diffuse blanch. Ear canal wash done with betadine. Access to the middle ear cavity was obtained through the endural approach through Lemperts incision.Temporalis Fascia was harvested and tympanic membrane was visualized. The margins of the perforation were freshened. The tympanomeatal flap is elevated via a trans canal approach by making two 8 mm radial longitudinal incisions lateral to the annulus superiorly at the tympanosquamous suture line (12 o’clock) and inferiorly (6 o’clock). The two incisions are joined by a transverse incision laterally to form a medially-based U-shaped flap. The canal skin and periosteum are then elevated in continuity with the fibrous annulus, which is then raised out of its bony groove. After raising posterior canal wall flap, circular incision was taken with circular knife anteriorly and anterior canal wall flap elevated till fibrous annulus. Tympanomeatal flap left attached to malleus. Posterior tympanomeatal flap is then reflected forward to access the posterior mesotympanum and ossicles.. Status of middle ear and ossicular chain inspected.
Malleus Relocation Technique
After dissecting the malleus free from the TM, the tensor tympani was sectioned as close as possible to its insertion into the malleus handle. Entire separation of the malleus from the TM was required. Any remnant of the incus (even within the epitympanum) was removed. Relocation was done using a strong 90-degree hook placed anterior to the neck of the malleus. Progressive posterior retraction of the malleus was applied until it came to lie directly above the stapes capitulum or footplate. Subsequent anterior retraction of the malleus was avoided by overstretching the anterior malleal ligament, the position thereby being maintained by the superior ligament of the malleus, which was preserved. In the relocated position, the malleus should lie immediately over the stapes footplate Precise measurement from the relocated malleus to the stapes capitulum or footplate can then be undertaken using a modified stapes-measuring rod. Placement of the shaft of the prosthesis was performed first, followed by easy positioning of the malleus handle into the groove of the prosthesis head in case of TORP and over the head of the prosthesis in case of PORP. In its final position, the prosthesis’ head should rest directly under the malleus handle without undue tension, and the malleus neck should stay away from the superior wall of the external auditory canal [6].
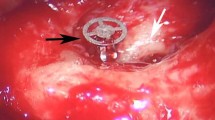
TORP Ossiculoplasty
Total ossicular replacement prosthesis done for half of patients. The prosthesis which we used for ossiculoplasty is Titanium Prosthesis with silastic band and teflon head with groove for malleus handle Distance between stapes footplate and neck of malleus was measured with measuring rod.Tympanic membrane grafting was done by interlay technique. Prosthesis was cut according to size measured with sizer provided with prosthesis. False membrane over stapes footplate was removed and mobility of foot plate is confirmed with round window reflex, then handle of malleus is repositioned after fracturing malleolar ligaments with curved hook and brought close to stapes area,minimum distance from footplate to under surface of malleus considered for TORP was 5 mm. Prosthesis was then placed on foot plate and repositioned handle of malleus was relocated over the groove for the malleus in the Teflon head of the prosthesis.
Round window reflex was checked and the tympanic membrane positioned.Grafted new tympanic membrane was repositioned Gelfoam was placed. Ear packing was done for 07 days.
PORP Ossiculoplasty
The prosthesis which we used for ossiculoplasty is Kurz Titanium Prosthesis Distance between stapes head and neck of malleus was measured with measuring rod.Tympanic membrane grafting was done by interlay technique. Prosthesis was cut according to size measured with a sizer provided with prosthesis. False membrane over stapes head was removed and mobility of stapes is confirmed with round window reflex, then handle of malleus is repositioned with curved hook and brought close to stapes area, Prosthesis was then placed on superstructure and repositioned handle of malleus was relocated over prosthesis head.Small piece of cartilage is used as interposition graft between prosthesis and tympanic membrane.Round window reflex was checked and the tympanic membrane positioned. Gel foam was placed. Ear packing was done for 07 days.
Post Operative Course
Post-operatively, patients belonging to both the study groups were treated similarly with parenteral antibiotics for 7 days. Periodical dressing change done. Suture removal and ear wick removal done on the 8th post-operative day. They were discharged on the 9th post-operative day after ensuring that the aural wound was healthy and there was no abnormal ear discharge. Patients were asked to keep the ear dry and given oral antibiotics for a week and topical antibiotic-steroid drops for 2 weeks.
Assessment of Results
Patients were followed up with otoscopic examination every week for first one month. Graft uptake was recorded at the end of the 1st month. Patients with successful graft uptake were carried forward in the study and followed up till 1 year. At 1 year follow up oto-endoscopic examination done to know about the status of the graft and prosthesis followed by pure tone audiometry to assess the air conduction thresholds and air conduction and bone conduction gap. Pure tone average, air bone gap, hearing gain were assessed. The quantitative data was used to analyse the improvements in hearing outcome and was statistically analysed using student t tests while qualitative data was assessed using the Pearson Chi square test. SPSS statistical software was used and P values < 0.05 were considered statistically significant. The results were tabulated and analysed statistically.

Reporting Guidelines
CONSORT Guidelines (Consolidated Standards of Reporting Trials).
Statstical software used.
SPSS (SPSS Statistics is a statistical software suite developed by IBM).
P value was calculated by Independent Test and Paired T test.
Ethical Considerations
Current clinical trial was duly passed by ethical committee of institutional board members, before recruitment of subjects.This study fully complied with the principles of the Declaration of Helsinki. Patient confidentiality was maintained at every point of study. Due written informed consent regarding treatment, pros and cons of treatment, potential risk, benefits and complications, was taken from every patient in language best understood by them. Assent was taken from parents for younger children who needed treatment.
Sample size Sample size calculator was used in calculating the sample size.
Results
Preoperative PTA of Moderate Conductive Hearing loss (40–55 db) was most found followed by severe conductive hearing loss (> 55 db.) with standard deviation of 7.155 and mean hearing loss was 46.30 db in TORP group. In this group post operative pure tone averages improved to mild hearing loss (26–30 db) in about 90 percent of patients with mean of 32 db. and standard deviation of 7.06. Preoperative PTA of severe Conductive Hearing loss (> 55 db) was most found followed by moderate Conductive Hearing loss (45–55 db) with standard deviation of 6.471 and mean hearing loss was 47 db in PORP group. Post operative Pure Tone averages improved to Mild Hearing loss (26–30 db) in about 90 percent of patients with mean of 33 db and standard deviation of 5.431 in PORP group. (Table 1, Fig. 1) ABG reduction in TORP group was 22.603 ± 12.34 while in PORP group was17.79 ± 10.743(Table 1, Fig. 1) The intergroup comparison between TORP and PORP in terms of ABG closure and Hearing gain was not statistically significant (Tables 2, 3 and Figs. 2, 3). The extrusion rate was 0.2 ± 0.406 In PORP group compared to 0.03 ± 0.182 in TORP group (Table 4, Fig. 4).
Discussion
Chronic middle ear infections (otitis media) damage the middle ear and lead to the development of conductive hearing loss. Surgery is the treatment of choice for chronic otitis media. In general, there are two aims of this approach. The first is to clear the infection by removing abnormal tissue and the second aim is to improve hearing by reconstructing the sound transmission apparatus, i.e., the eardrum, the ossicular chain and the middle ear cavity. Traditionally, either PORP or TORP is applicable, depending primarily on whether there is an intact stapes superstructure or only a stapes footplate. However, it is still unclear whether ossicular reconstruction has a better long-term outcome with PORP or TORP. Several clinical investigations show that reconstruction with PORP leads to better hearing than TORP [7,8,9]. Conversely, there are studies that show ossicular reconstructions to the stapes footplate with TORP result in significantly better hearing outcomes than reconstructions to the stapes superstructure with PORP even in cases with only incus erosion [10]. In addition, some investigations suggest that there is no significant difference between the two models [11, 12].
To determine which hypothesis is accurate, current study was undertaken in our department comparing hearing gain and long-term stability by using TORP and PORP in Austin A classification. Age group more than 40 years was most affected in both TORP and PORP groups. Second most common age group affected in both TORP and PORP groups was between 15 and 30 years which is in correlation with studies conducted by Alaani et al. [13], Eleftheriadou et al. [14], Ho et al. [15], Kobayashi et al. [16], Mardassi et al. [17], Martin et al. [18], Nikolaou et al. [19]. Females were most commonly affected with ossicular erosion than males. Large perforation followed subtotal perforation followed by medium perforation were most common presenting feature in PORP group, similar trends were also seen in TORP group, which correlated with study conducted by Tripathi, Nautiyal et al. [20]. Left ear was most affected in both PORP and TORP groups, although gender and laterality does not influence the outcome procedure,still the results of present study in terms of gender and laterality correlated with large series conducted by Abraham et al. [21]. Sensitivity and specificity for incus erosion was 73.1% and 57.8% respectively. P value was less than 0.05, which exactly correlated by study conducted by Singh et al. (2019) [22].
Preoperative pure tone audiometry in PORP group showed severe conductive hearing loss of more than 55 db. in 16 patients while 14 patients showed moderate conductive hearing loss with mean hearing loss of 47.34 db. and standard deviation of 6.471 db., these results were quite like TORP group where 14 patients showed severe conductive, and 14 patients showed moderate conductive hearing loss with average of 46.30 db., and standard deviation of 7.155. Mean air borne gap in TORP group was 39.14 db with standard deviation of 8.23.As compared to TORP group mean ABG in PORP group was 42.6 db with standard deviation of 7.364. Preoperative audiometric findings of present study correlated with studies conducted by, Karja Je et al., Mohanty et al. and Ebenezer, where similar audiometric results were found in presence of incudal necrosis [23,24,25].
Both groups were quite comparable with respect to ABG and preoperative PTA in preoperative selection criteria. Over all incidence of middle ear anomalies is extremely rare and it was found out to be around 1:3800 births, however in present study also there was no incidence of middle ear anomalies [26]. Post operative PTA audiometry in PORP group at 3 months improved to mild conductive hearing loss in 27 out of 30 patients with mean of 33.07 db and SD of 5.432 which was almost similar in results as compared to TORP group where average 32.37 db was found with 27 PTA reports out of 30.(Table 1, Fig. 1).
Average ABG reduction in TORP group was 22.6 db. and average reduction in PORP group was 17.79 db with respective standard deviation of 12.34 db and 10.74 db respectively (Table 2, Fig. 2). Above mentioned difference was not statistically significant as both groups showed almost similar results in improvement. Average Hearing gain in TORP group was 15.30 db with standard deviation of 7.24 and average hearing gain in PORP group was1 4.25 db. with standard deviation of 6.114.Above mentioned findings were again not statistically significant as both groups showed almost comparable gain in hearing (Table 3; Fig. 3).When individual group were compared in terms preoperative and postoperative PTA and ABG improvement both groups showed statistically significant improvement (Table 1; Fig. 1) However, there was statistically significant difference in terms of rates of extrusion when both groups were compared. TORP showed better stability as compared to PORP (Table 4; Fig. 4).
The literature is controversial as to which is superior and better. Several studies have favoured PORP over TORP with better A-B gap closures with the former [7, 15]. The other studies especially retrospective reviews favour TORP over PORP. The reason for this as per their research is less extrusion and failure rates of TORP over long- term compared to PORP with comparable A-B gap closure [12, 15, 27, 28]. In study conducted by Macias et al., in series of 60 cases, they found out that overall extrusion of PORP was more than at end of one year, extrusion of PORP was 4.9 percent and no torp was extruded in their study [6]. Other studies maintain a neutral stance over which prosthesis is better with main focus being improvement in hearing which is more in favour for PORP group in some studies or comparable for both the prosthesis in others. These studies comment only on overall extrusion rates [29,30,31,32]. Mardaasi et al. concluded that increasing the length of the ossicular prosthesis, especially TORP, may improve postoperative functional results [22].
A significant study by Vincent et al. found out that the overall failure rate in PORP group was 31.2% (90 cases) compared with 15.2% (43 cases) in TORP group, they postulated that stability of the implant and hearing outcomes was better in TORP than PORP in their series Vincent et al. used TORP prosthesis with a new design. Their titanium prosthesis had a Teflon head with groove for malleus and a silastic band at the handle of the prosthesis. Through the silastic rubber band, the prosthesis is attached to the stapes superstructure by means of a silastic band which was claimed to solve the problems of instability and displacement [6, 33].
Present study also concluded same that stability of TORP is better than PORP in long term follow up which can be attributed to reason of malleus relocation technique and silastic banding with stapes suprastructure as introduced by prof Robert Vincent. The only cases of Austin type A where we found PORP easier than TORP was cases where facial nerve was overhanging and covering the stapes footplate.
Limitation and Strengths of Current Study
Among the positive attributes of the current study were its study design. Study was carefully designed with every effort taken to properly randomise the current study, despite randomisation subjects in the study were properly balanced with respect to age, nature of disease, degree of hearing loss,method of surgery, quality of types of implants used. All possible biases which could influence the results of study were carefully studied and every and best possible effort was tried to reduce the confounding factors.
Extensive literature was studied to design material and methods of study. Selection and exclusion criteria were carefully discussed with the ethical committee of the institute. It was ensured that a single well-trained surgeon with good experience in alloplastic ossicular implants should complete the cases in each group with a similar approach.
Follow up was carefully designed and a single audiologist was allocated a to follow all the cases in both the groups and the audiologist was blinded to the prosthesis used. Every possible effort was taken to document the patients preoperative, intraoperative and postoperative follow up data in the most scientific and logical manner. Implants used were carefully selected ensuring their certification and good quality.
Despite all these merits, there were still many shortcomings in present study. Although study was well randomised, but it could not be blinded because number of surgeons participating in present study were limited.There can be issues of generality of results which is highly attributed to specific surgical training of this technique, number of subjects who participated in study were less hence there are concerns for external validity.
Summary
In current study TORP and PORP were used as choice of ossicular implants to study hearing outcome in Austin type A classification. It was found that there was significant improvement in preoperative and post operative hearing again in both the groups. Air borne gap significantly improved from moderate and moderate severe to mild hearing loss in both groups. There were also significant improvements in pre-operative pure tone thresholds when compared to post-operative thresholds in both groups. When stability of both implants was studied with respect to extrusion rates and post operative displacements, TORP secured better results as compared to PORP, long term stability results of TORP were better than PORP. Although material of both implants was titanium, but TORP implants used here had specific advantage of design where TORP had fluoroplastic head along with silastic band which can be secured to stapes neck. Two other factors which enhanced stability of TORP were use of malleus reposition technique and length of implants,majority of cases length from stapes to neck of malleus was 6.5 mm, length of implant greatly influences the stability of implants. All patients selected had lower Middle Ear risk index which improved hearing results in both groups. Gender, age and laterality did not have significant impact on outcome of results of ossiculoplasty in both groups. Incidence of Middle ear anomalies were exceeding low, and no patient had any middle ear anomaly in both the groups. HRCT temporal bone has high specificity and sensitivity to know about incus erosion. Reduction of preoperative air borne gap along with reduction of preoperative pure tone thresholds were main parameters used for evaluation of outcomes.
Conclusion
Although Both PORP and TORP can be used for ossiculoplasty in Austin type A classification, but we recommend TORP with silastic banding to stapes neck along with malleus reposition technique for better and stable long term hearing results.
References
Operational Guidelines for 12th Five Year Plan, Ministry of Health & Family Welfare Government of India National Programme for Prevention and Control of Deafness (NPPCD)
Acuin DJ (2004) Prevention of blindness and deafness. Child and adolescent health and development. W.H.O bulletin, Geneva
Pfiffner F, Caversaccio MD, Kompis M (2011) Comparisons of sound processors based on osseointegrated implants in patients with conductive or mixed hearing loss. Otol Neurotol 32:728–735
Asai M, Huber AM, Goode RL (1999) Analysis of the best site on the stapes footplate for ossicular chain reconstruction. Acta Otolaryngol 119:356–361
Kartush JM (1994) Ossicular chain reconstruction. Capitulum to malleus. Otolaryngol Clin North Am 27(4):689–715
Vincent R et al (2004) Malleus relocation in ossicular recon- struction managing the anteriorly positioned malleus: results in a series of 268 cases. Otol Neurotol 25:223–230
Javia LR, Ruckenstein MJ (2006) Ossiculoplasty. Otolaryngol Clin North Am 39(6):1177–1189
Zhang LC, Zhang TY, Dai PD, Luo JF (2011) Titanium versus non-titanium prostheses in ossiculoplasty: a meta-analysis. Acta Otolaryngol 131:708–715
Bayazit Y, Goksu N, Beder L (1999) Functional results of Plas- tipore prosthesis for middle ear ossicular chain reconstruction. Laryngoscope 109:709–711
Jackson CG, Glasscock ME 3rd, Schwaber MK, Nissen AJ, Christiansen SG, Smith PG (1983) Ossicular chain reconstruction: the TORP and PORP in chronic ear disease. Laryngoscope 93(8):981–988. https://doi.org/10.1288/00005537-198308000-00001
Slater PW, Rizer FM, Schuring AG, Lippy WH (1997) Practical use of total and partial ossicular replacement prosthesis in os-siculoplasty. Laryngoscope 107:1193–1198
Moretz WH Jr (1998) Ossiculoplasty with an intact stapes: superstructure versus footplate prosthesis placement. Laryngoscope 108(Suppl 89):1–12. https://doi.org/10.1097/00005537-199811001-00001
Alaani A, Raut VV (2010) Kurz titanium prosthesis ossiculopl- asty–follow-up statistical analysis of factors affecting one year hearing results. Auris Nasus Larynx 37:150–154
Eleftheriadou A, Chalastras T, Georgopoulos S, Yiotakis J, Ma-nolopoulos L, Iliadis I, Charalabopoulos K, Kandiloros D (2009) Long-term results of plastipore prostheses in reconstruction of the middle ear ossicular chain. ORL J Otorhinolaryngol Relat Spec 71:284–288
Ho SY (2003) Early results with titanium ossicular implants. Otol Neurotol 24(2):149–152
Kobayashi T, Gyo K, Shinohara T, Yanagihara N (2002) Ossic- ular reconstruction using hydroxyapatite prostheses with inter- posed cartilage. Am J Otolaryngol 23:222–227
Mardassi A, Deveze A, Sanjuan M, Mancini J, Parikh B, El-bedeiwy A, Magnan J, Lavieille JP (2011) Titanium ossicular chain replacement prostheses: prognostic factors and preliminary functional results. Eur Ann Otorhinolaryngol Head Neck Dis 128:53–58
Martin AD, Harner SG (2004) Ossicular reconstruction with titanium prosthesis. Laryngoscope 114:61–64
Nikolaou A, Bourikas Z, Maltas V, Aidonis A (1992) Ossicu- loplasty with the use of autografts and synthetic prosthetic materials: a comparison of results in 165 cases. J Laryngol Otol 106:692–694
Tripathi P, Nautiyal S (2017) Incidence and preoperative predictive indicators of incudal necrosis in CSOM: A prospective study in a tertiary care centre. Indian J Otolaryngol Head Neck Surg 69(4):459–463. https://doi.org/10.1007/s12070-017-1224-0
Abraham ZS, Ntunaguzi D, Kahinga AA, Mapondella KB, Massawe ER, Nkuwi EJ, Nkya A (2019) Prevalence and etiological agents for chronic suppurative otitis media in a tertiary hospital in Tanzania. BMC Res Notes 12:1–6
Singh J, Bhardwaj B (2019) How efficacious is HRCT temporal bone in determining the ossicular erosion in cases of safe and limited squamous type CSOM? Indian J Otolaryngol Head Neck Surg 71(Suppl 2):1179–1182. https://doi.org/10.1007/s12070-018-1250-6
Kärjä J, Jokinen K, Seppälä A (1976) Destruction of ossicles in chronic otitis media. J Laryngol Otol 90(6):509–518. https://doi.org/10.1017/S0022215100082402
Mohanty S, Gopinath M, Subramanian M, Sudhir A (1998) Relevance of pure tone average (PTA) as a predictor for incus erosion middle ear cholesteatoma. Indian J Otol. 4(2):55
Ebenezer J, Rupa V (2010) Preoperative predictors of incudal necrosis in chronic suppurative otitis media. Otolaryngol Head Neck Surg 142(3):415–420. https://doi.org/10.1016/j.otohns.2009.11.026
Thorn L (1994) Entwicklung des Ohres (einschließlich Entstehung von Missbildungen, experimentelle Embryologie und In-vitro-Studien). In: Helms J (ed) Oto-Rhino-Laryngologie in Klinik und Praxis. Thieme, Stuttgart, pp 1–22
Nguyen DQ, Morel N, Dumas G, Troussier J, Lavieille JP, Schmerber S (2005) Ossiculoplasty with KURZ titanium pros- thesis. Ann Otolaryngol Chir Cervicofac 122:187–193
Michael P, Fong J, Raut V (2008) Kurz titanium prostheses in paediatric ossiculoplasty—short term results. Int J Pediatr Otorhinolaryngol 72:1329–1333
Schmerber S, Troussier J, Dumas G, Lavieille JP, Nguyen DQ (2006) Hearing results with the titanium ossicular replacement prostheses. Eur Arch Otorhinolaryngol 263:347–354
Vassbotn FS, Moller P, Silvola J (2007) Short-term results using Kurz titanium ossicular implants. Eur Arch Otorhinolaryngol 264:21–25
Quaranta N, Fernandez-Vega Feijoo S, Piazza F, Zini C (2001) Closed tympanoplasty in cholesteatoma surgery: long-term (10 years) hearing results using cartilage ossiculoplasty. Eur Arch Otorhinolaryngol 258:20–24
Vincent R, Rovers M, Mistry N, Oates J, Sperling N, Grolman W (2011) Ossiculoplasty in intact stapes and malleus patients: a comparison of PORPs versus TORPs with malleus relocation and silastic banding techniques. Otol Neurotol 32:616–625
Vincent R et al (2005) Ossiculoplasty with intact stapes and absent malleus the silastic banding technique. Otol Neurotol 26:846–852
Funding
It was a non-funded study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest.
Ethical Approval
Before starting the study, ethical clearance was taken from institutional ethical committee as per Declaration of Helsinki.
Informed Consent
Informed consent was taken by all the patients before surgery and enrolment into the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Singh, J., Sood, A.S., Bhardwaj, B. et al. TORP Versus PORP in Austin Type A Ossicular Defects: Which is the Right Choice?. Indian J Otolaryngol Head Neck Surg (2024). https://doi.org/10.1007/s12070-024-05087-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12070-024-05087-8