Abstract
Background
Most women suffer from perineal trauma during childbirth, whether it is natural tears or episiotomy.
Objectives
To perform a systematic review and network meta-analysis investigating the effectiveness of different PFMT relevant strategies in the prevention of perineal trauma.
Search strategy
PubMed, Embase, the Cochrane Library, CINAHL, CNKI, CBM, WANFANG DATABASE, and ClinicalTrials.gov were searched for citations published in any language from inception to 1 July 2021.
Selection criteria
Randomized controlled trials (RCTs) of PFMT relevant prevention strategies for preventing perineal trauma during childbirth.
Data collection and analysis
Data were independently extracted by two reviewers. Relative treatment effects were estimated using network meta-analysis (NMA).
Main results
Of 12 632 citations searched, 21 RCTs were included. Comparing with usual care, “PFMT combine with perineal massage” and PFMT alone showed more superiority in intact perineum (RR = 5.37, 95% CI: 3.79 to 7.60, moderate certainty; RR = 2.58, 95% CI 1.34–4.97, moderate certainty, respectively), episiotomy (RR = 0.26, 95% CI 0.14–0.49, very low certainty; RR = 0.63, 95% CI 0.45–0.90, very low certainty, respectively), and OASIS (RR = 0.35, 95% CI 0.16–0.78, moderate certainty; RR = 0.49, 95% CI 0.28–0.85, high certainty, respectively). “PFMT combine with perineal massage” showed superiority in reducing perineal tear (RR = 0.41, 95% CI 0.20–0.85, moderate certainty).
Conclusions
In view of the results, antenatal “PFMT combine with perineal massage” and PFMT were effective strategies for the prevention of perineal trauma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Issue : How effective is PFMT in preventing perineal trauma? What is already known : PFMT can be effective in preventing and treating pelvic floor muscle dysfunction, but its preventive effect on perineal injury has yet to be verified. What this paper adds : With moderate certainty of evidence, “PFMT combine with perineal massage” and PFMT showed more superiority for preventing perineal trauma. |
Introduction
Most women suffer from perineal trauma during childbirth, whether it is natural tears or episiotomy, affecting 53–79% of women [1]. In Queensland, 59.16% women required surgical repair because of perineal trauma in 2020 [2]. Injury to the perineum without involvement of the anal sphincter does not generally cause long term problems for women. In contrast, injury to the anal sphincter can result in long term sequelae, such as fecal incontinence, and can significantly affect women’s quality of life [1]. Episiotomy and obstetric anal sphincter injuries (OASIS) rates are commonly used as quality indicators of health systems and health care. [3]
The prevention of perineal trauma through exercise during pregnancy was feasible and effective, which has been verified and recommended by a number of guidelines and clinical studies [4,5,6,7,8,9,10]. However, the results concerning the relationship between different antenatal PFMT relevant prevention strategies and perineal trauma seemed to be inconclusive. Therefore, we intended to use network meta-analysis method to combine results of RCTs to assess the relative effectiveness of different PFMT relevant strategies in the prevention of perineal trauma during childbirth.
Methods
Our systematic review and NMA manuscript were written in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension statement for reporting systematic reviews incorporating NMA [11].
Search strategy
We searched PubMed, Embase, the Cochrane Library, CINAHL, CNKI, CBM, WANFANG DATA and ClinicalTrials.gov for citations published in any language from inception to 1 July 2020. We also reviewed reference lists of included studies and related systematic reviews. The search strategy was provided in Appendix Table 2
Study selection and criteria
We included RCTs of different strategies (except antenatal perineal massage) used to prevent perineal trauma in pregnant women. We followed the PICO (population, strategies, comparison, outcome) framework to determine the research question and to facilitate literature search: (1) Population: single pregnant women, there were no other restrictions; (2) Strategies: PFMT relevant strategies; (3) Comparison: usual care or other strategies. Usual care means that pregnant women only receive routine guidance and nurse during pregnancy; (4) Outcome: perineal trauma; (5) Study design: RCTs. We excluded: (1) in vitro and animal studies, (2) studies whose data were unable for extraction and analysis. Appendix Table 3 shows the definitions of different prevention strategies.
Data extraction
Pairs of reviewers (XC, QY) independently screened all citations and extracted data from the included studies. Discrepancies in study inclusion were resolved by deliberation within the reviewer pairs or with input from a third reviewer (MYS). The following items were extracted from each identified study: (1) basic information: title, authors, publication year, etc.; (2) risk of bias domains; and (3) study outcomes: the rate of intact perineal, the rate of episiotomy, the rate of perineal tear, etc.
Risk of bias assessment
Two reviewers independently assessed risk of bias with adjudication by a third reviewer, using a Cochrane Collaboration tool [12]. This tool included seven domains: random sequence generation, allocation concealment, blinding of participants and personal, blinding of outcome assessment, incomplete outcome data, selective reporting, and other bias.
Statistical analysis
We conducted network meta-analysis with R version 4.1.2 and Stata 17.0 [13, 14]. For the dichotomous outcomes, we calculated risk ratios (RRs) and 95% confidence intervals, and mean differences (MDs) and 95% confidence intervals for the continuous outcomes. We assessed the heterogeneity in strategies effects among studies using visual inspection of forest plots and the I2 We assessed the transitivity (similarity) assumption by comparing the distribution of the population, the strategies, and the methodological characteristics of the studies across strategies comparisons [15]. To assess incoherence, we assessed the global incoherence for the entire network for each outcome under the assumption of a full design-by-strategies interaction random effects model, and then local incoherence for each comparison using the node-splitting model [16, 17]. We ranked strategies according to their P score, which is between 0 and 1 [18]. We used the egger’s test and the funnel chart test to publish bias.
Certainty of evidence assessment
We used the GRADE (Grading of Recommendations, Assessment, Development, and Evaluation) approach to assess the certainty of evidence [19]. Regarding the certainty of evidence in estimates: high certainty means that further research is very unlikely to change our confidence in the estimate of effect; moderate certainty means that further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate; low certainty means that further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate; and very low certainty means that any estimate of effect is very uncertain. [20]
Results
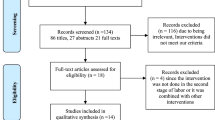
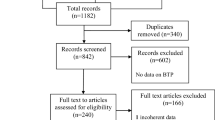
The search strategies generated 12,632 citations, 21 RCTs were eligible [21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41]. Figure 1 presents the study flow diagram.
Characteristics of included studies
Twenty-one RCTs with sample sizes from 20 to 596, enrolled a total of 4931 patients. All RCTs included pregnant women, and 12 of these included primiparous women, one of these included primiparous women with bladder neck mobility (BNM), one of these included pregnant women ≥ 35 years, one of these included pregnant women with pelvic floor dysfunction.
Figure 2 presents the network plot including all studies and demonstrated that the most common comparisons were between PFMT relevant strategies and usual care. Ten RCTs compared PFMT with usual care; five RCTs compared Epi-NO with usual care; three RCTs compared “PFMT combine perineal massage” with usual care; one RCT compared “PFMT combine perineal massage” with perineal massage; two RCTs compared yoga with usual care (one Pilates, one yoga). Table 1 presents detailed characteristics of individual RCTs.
Risk of bias assessment
Most of the included studies showed a low or ambiguous risk of bias in seven areas, with one study (4.76%) showed a high risk of bias in random sequences generation and two studies (9.52%) showed a high risk of bias in the blindness. Because pelvic floor muscle exercise required patient participation, it was difficult to implement blinding method. All outcome indicators were measurable objective, we considered the impact of blinding method was small. Overall, only four studies were assessed as to be low risk of bias, and the remaining 17 studies were all high risk of bias. Appendix Fig. 5 presents the risk of bias.
Primary outcome
In this network meta-analysis, none of the outcomes formed a closed loop. Therefore, we did not need to test the inconsistency. Appendix Figs. 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32 presents forest plots for each outcome. No publication bias was observed, see Appendix Figs. 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33.
The rate of intact perineum
Eight RCTs [25, 27, 30, 31, 35, 36, 38, 39] reported the rate of intact perineum, included usual care, PFMT, Epi-NO, “PFMT combine with perineal massage”, perineal massage, and Yoga. Compared with usual care, moderate certainty of evidence suggested that “PFMT combine with perineal massage” (RR = 5.37, 95% CI 3.79–7.60), Yoga (RR = 3.81, 95% CI 2.55–5.69), PFMT (RR = 2.58, 95% CI 1.34–4.97), Epi-NO (RR = 1.77, 95% CI 1.30–2.40) could significantly improve the rate of intact perineum. There were no differences between strategies except the comparison between “PFMT combine with perineal massage” and Epi-NO. Figure 3 shows the GRADE summary of findings.
The rate of episiotomy
Twenty RCTs [21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37, 39,40,41] reported the rate of episiotomy, included usual care, PFMT, Epi-NO, “PFMT combine with perineal massage”, perineal massage, and Yoga. Compared with usual care, low certainty of evidence suggested that “PFMT combine with perineal massage” (RR = 0.26, 95% CI 0.14–0.49) and PFMT (RR = 0.63, 95% CI 0.45–0.90) could significantly reduce the rate of episiotomy, and combined strategy was better than PFMT alone (RR = 0.41, 95% CI 0.20–0.85; low certainty). There were no significant differences between other strategies (Fig. 3).
The rate of perineal tear
Ten RCTs [21,22,23, 25, 30, 36,37,38,39,40] reported the rate of perineal tear, included usual care, PFMT, Epi-NO and “PFMT combine with perineal massage” strategies. Compared with usual care, low certainty of evidence suggested that “PFMT combine with perineal massage” could significantly reduce the rate of perineal tear (RR = 0.52, 95% CI 0.31–0.88). There were no significant differences between strategies (Fig. 4).
The rate of OASIS
Nine RCTs [21, 23, 26, 27, 29, 30, 34, 38, 41] reported the rate of OASIS, included usual care, PFMT, Epi-NO and “PFMT combine with perineal massage” strategies. Compared with usual care, high certainty of evidence suggested that PFMT (RR = 0.49, 95% CI 0.28–0.85) and moderate certainty of evidence suggested that “PFMT combine with perineal massage” (RR = 0.35, 95% CI 0.16–0.78) could significantly reduce the rate of OASIS. Results suggested no significant differences between any of strategies (Fig. 4).
Secondary outcomes
Compared with usual care, “PFMT combine with perineal massage” (RR = 0.70, 95% CI 0.56–0.88, moderate certainty) and perineal massage (RR = 0.60, 95% CI 0.39–0.93, low certainty) could significantly reduce the rate of slight perineal tear; Epi-NO improved the rate of assisted vaginal delivery (RR = 1.59, 95% CI 1.04–0.42, moderate certainty); PFMT combine with perineal massage (RR = 1.38, 95% CI 1.04–1.82, low certainty) and yoga (RR = 1.75, 95% CI 1.47–2.08, moderate certainty) could significantly improve the rate of natural childbirth; PFMT combine with perineal massage (RR = 0.31, 95% CI 0.12–0.83, low certainty) and yoga (RR = 0.47, 95% CI 0.32–0.71, low certainty) could significantly reduce the rate of caesarean section; PFMT combine with perineal massage (RR = 0.35, 95% CI 0.16–0.78, low certainty) and PFMT (RR = 0.49, 95% CI 0.28–0.85, low certainty) could significantly reduce the rate of fetal distress; PFMT (MD = − 20.27, 95% CI − 38.63–1.90, low certainty) could significantly reduce the duration of the second stage of labor. Figure 5 presents the GRADE summary of findings for secondary outcomes.
Discussion
Main findings
Our meta-analysis showed that both “PFMT combine with perineal massage” and PFMT showed advantages in terms of the primary outcomes compared with usual care. This suggested that “PFMT combine with perineal massage” and PFMT might be the most effective first line strategy for the prevention of perineal trauma.
Some systematic review found that exercise could not prevent perineal trauma, but one found that perineal massage could prevent perineal trauma [12,13,14,15]. In the present network meta-analysis, we focused on the relationship between different antenatal PFMT relevant strategies and perineal trauma. Therefore, we did not deeply compare PFMT relevant strategies with perineal massage. This network meta-analysis provided moderate certainty evidence for the use of “PFMT combine with perineal massage” and PFMT to prevent perineal trauma.
Strengths and limitations
The strength of our study was that we considered most current PFMT relevant strategies for the prevention of perineal trauma. Application of the network meta-analysis framework allowed to compare multiple relative strategies and rank the best agents for preventing perineal trauma given the evidence to date from RCTs. However, there were several limitations in our study. First, we did not consider all antenatal strategies; therefore, our conclusion was limited to these strategies we focused on. Second, we did not consider cost effectiveness, scalability, and sustainability of these strategies. Third, we have not found any research about patient’s preference; therefore, the most effective strategy might not be accepted by pregnant women.
Interpretation
The strategies of PFMT and perineal massage were popular in many countries. However, now, PFMT is more used in the PFM recovery, and perineal massage is more used in intrapartum. Several effective antenatal strategies, including perineal massage and exercise were already accessible in some clinical and community settings. However, the decision to use any of these strategies, and the order in which they might be used, was based on choices made by physician and patient, and to some extent was influenced by many factors.
In view of the results, with moderate certainty of evidence, antenatal “PFMT combine with perineal massage” and PFMT were effective in the prevention of perineal trauma. Clinicians and healthcare professionals could consider to recommend these strategies based on the condition and preference of pregnant women.
References
American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Obstetrics (2016) Practice bulletin No 165: prevention and management of obstetric lacerations at vaginal delivery. Obstet Gynecol 128(1):e1-e15. DOI: https://doi.org/10.1097/AOG.0000000000001523.
Queensland Health (2020). Mothers birthing in Queensland 2020. https://www.health.qld.gov.au/__data/assets/pdf_file/0019/1130491/6-labdel2020.pdf (Accessed 20 May 2022).
World Health Organization (2016). Standards for improving quality of maternal and newborn care in health facilities. Geneva: World Health Organization. https://www.who.int/publications-detail-redirect/9789241511216 (Accessed 20 May 2022).
Queensland Health (2020). Queensland Clinical Guidelines: Perineal care. https://www.health.qld.gov.au/__data/assets/pdf_file/0022/142384/g-pericare.pdf (Accessed 20 May 2022).
Waldman R (2019) ACOG practice bulletin no. 198: Prevention and management of obstetric lacerations at vaginal delivery. Obstet Gynecol 133(1):185. https://doi.org/10.1097/AOG.0000000000003041
Ducarme G, Pizzoferrato AC, de Tayrac R, Schantz C, Thubert T, Le Ray C et al (2019) Perineal prevention and protection in obstetrics: CNGOF clinical practice guidelines. J Gynecol Obstet Hum Reprod 48(7):455–460. https://doi.org/10.1016/j.jogoh.2018.12.002
Abdelhakim AM, Eldesouky E, Elmagd IA, Mohammed A, Farag EA, Mohammed AE et al (2020) Antenatal perineal massage benefits in reducing perineal trauma and postpartum morbidities: a systematic review and meta-analysis of randomized controlled trials. Int Urogynecol J 31(9):1735–1745. https://doi.org/10.1007/s00192-020-04302-8
Gomes Lopes L, Maia Dutra Balsells M, Teixeira Moreira Vasconcelos C, Leite de Araújo T, Teixeira Lima FE, de Souza AP (2022) Can pelvic floor muscle training prevent perineal laceration? A systematic review and meta- analysis. Int J Gynaecol Obstet 157(2):248–254. https://doi.org/10.1002/ijgo.13826
Brito LG, Ferreira CH, Duarte G, Nogueira AA, Marcolin AC (2015) Antepartum use of Epi-No birth trainer for preventing perineal trauma: systematic review. Int Urogynecol J 26(10):1429–1436. https://doi.org/10.1007/s00192-015-2687-8
Masoud AT, AbdelGawad MM, Elshamy NH, Mohamed OM, Hashem ZY, Abd Eltawab AK et al (2020) The effect of antenatal exercise on delivery outcomes: a systematic review and meta-analysis of randomized controlled trials. J Gynecol Obstet Hum Reprod 49(6):101736. https://doi.org/10.1016/j.jogoh.2020.101736
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C et al (2015) The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care strategies: checklist and explanations. Ann Intern Med 162(11):777–784. https://doi.org/10.7326/M14-2385
Cumpston MS, McKenzie JE, Welch VA, Brennan SE (2022). Strengthening systematic reviews in public health: guidance in the Cochrane Handbook for Systematic Reviews of Interventions, 2nd edition. J Public Health (Oxf) 28:fdac036. Doi: https://doi.org/10.1093/pubmed/fdac036.
Rücker G (2012) Network meta-analysis, electrical networks and graph theory. Res Synth Methods 3(4):312–324. https://doi.org/10.1002/jrsm.1058
Chaimani A, Higgins JP, Mavridis D, Spyridonos P, Salanti G (2013) Graphical tools for network meta-analysis in STATA. PLoS ONE 8(10):e76654. https://doi.org/10.1371/journal.pone.0076654
Higgins JPT, Jackson D, Barrett JK, Lu G, Ades aE, White IR (2012) Consistency and inconsistency in network meta-analysis: concepts and models for multi-arm studies. Res Synth Methods 3(2):98–110. https://doi.org/10.1002/jrsm.1044
Dias S, Welton NJ, Caldwell DM, Ades AE (2010) Checking consistency in mixed strategies comparison meta-analysis. Stat Med 29(7–8):932–944. https://doi.org/10.1002/sim.3767
Krahn U, Binder H, König J (2013) A graphical tool for locating inconsistency in network meta-analyses. BMC Med Res Methodol 13:35. https://doi.org/10.1186/1471-2288-13-35
Rücker G, Schwarzer G (2015) Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med Res Methodol 15:58. https://doi.org/10.1186/s12874-015-0060-8
Brignardello-Petersen R, Bonner A, Alexander PE, Siemieniuk RA, Furukawa TA, Rochwerg B et al (2018) Advances in the GRADE approach to rate the certainty in estimates from a network meta-analysis. J Clin Epidemiol 93:36–44. https://doi.org/10.1016/j.jclinepi.2017.10.005
Brignardello-Petersen R, Florez ID, Izcovich A, Santesso N, Hazlewood G, Alhazanni W et al (2020) GRADE approach to drawing conclusions from a network meta-analysis using a minimally contextualized framework. BMJ 371:m3900. https://doi.org/10.1136/bmj.m3900
Agur W, Steggles P, Waterfield M, Freeman R (2008) Does antenatal pelvic floor muscle training affect the outcome of labour? A randomised controlled trial. Int Urogynecol J Pelvic Floor Dysfunct 19(1):85–88. https://doi.org/10.1007/s00192-007-0391-z
Dias LA, Driusso P, Aita DL, Bø K, Ferreira CHJ (2011) Effect of pelvic floor muscle training on labour and newborn outcomes: a randomized controlled trial. Rev Bras Fisioter 15(6):487–493. https://doi.org/10.1590/s1413-35552011005000011
Dieb AS, Shoab AY, Nabil H, Gabr A, Abdallah AA, Shaban MM et al (2020) Perineal massage and training reduce perineal trauma in pregnant women older than 35 years: a randomized controlled trial. Int Urogynecol J 31(3):613–619. https://doi.org/10.1007/s00192-019-03937-6
HP Dietz,S Langer,K Atan,KL Shek,J Caudwell-Hall,RG Rojas (2014). Does the Epi-No birth trainer prevent vaginal birth-related pelvic floor trauma? A multicenter prospective randomised controlled trial. 44th Annual Meeting of the International-Continence-Society (ICS)Volume: 33
Lekskulchai O, Wanichsetakul P (2014) Effect of pelvic floor muscle training (PFMT) during pregnancy on bladder neck descend and delivery. J Med Assoc Thai 97(Suppl 8):S156–S163
Kamisan Atan I, Shek KL, Langer S, Guzman Rojas R, Caudwell-Hall J, Daly JO, Dietz HP (2016) Does the Epi-No(®) birth trainer prevent vaginal birth-related pelvic floor trauma? A multicentre prospective randomised controlled trial. BJOG 123(6):995–1003. https://doi.org/10.1111/1471-0528.13924
Leon-Larios F, Corrales-Gutierrez I, Casado-Mejía R, Suarez-Serrano C (2017) Influence of a pelvic floor training programme to prevent perineal trauma: a quasi-randomised controlled trial. Midwifery 50:72–77. https://doi.org/10.1016/j.midw.2017.03.015
Rodríguez-Díaz L, Ruiz-Frutos C, Vázquez-Lara JM, Ramírez-Rodrigo J, Villaverde-Gutiérrez C, Torres-Luque G (2017) Effectiveness of a physical activity programme based on the Pilates method in pregnancy and labour. Enferm Clin 27(5):271–277. https://doi.org/10.1016/j.enfcli.2017.05.008
Ruckhäberle E, Jundt K, Bäuerle M, Brisch KH, Ulm K, Dannecker C et al (2009) Prospective randomised multicentre trial with the birth trainer EPI-NO for the prevention of perineal trauma. Aust N Z J Obstet Gynaecol 49(5):478–483. https://doi.org/10.1111/j.1479-828X.2009.01044.x
Shek KL, Chantarasorn V, Langer S, Phipps H, Dietz HP (2011) Does the Epi-No Birth Trainer reduce levator trauma? A randomised controlled trial. Int Urogynecol J 22(12):1521–1528. https://doi.org/10.1007/s00192-011-1517-x
Deng XP (2019) Significance of pelvic floor muscle function exercise guidance for primiparas who give birth naturally. Contemp Med Essays 17(10):9–11
Huang JL, Yan Q, Shen SW, You WH, Huang LX (2020) The effect of perineal massage combined with Kegel exercise during pregnancy on the delivery outcome of primipara. China Pract Med 15(21):35–37. https://doi.org/10.14163/j.cnki.11-5547/r.2020.21.013
Shi S (2018) The influence of yoga during pregnancy on pregnancy outcome of primipara. China Urban Rural Ent Health 33(06):46–48. https://doi.org/10.16286/j.1003-5052.2018.06.018
Salvesen KA, Mørkved S (2004) Randomised controlled trial of pelvic floor muscle training during pregnancy. BMJ 329(7462):378–380. https://doi.org/10.1136/bmj.38163.724306.3A
Wang K (2015) Clinical research on PFMT behavior guidance for pregnant and lying-in women before and after childbirth. J Inn Mong Med Univ 37(S1):301–303. https://doi.org/10.16343/j.cnki.issn.2095-512x.2015.s1.076
Wang Y, Zhou GL, Zou HY, Wang CX, Xiao SL, Pan JF et al (2015) Study on the effect of modified Kegel functional exercise nursing on the delivery method of pregnant women with pelvic floor dysfunction. Mod Diagnosis Treat 26(18):4294–4295
Cai HL (2019) The effect of antenatal perineal massage combined with Kegel exercise on the delivery outcome of primipara. Nurs Pract Res 16(17):87–89. https://doi.org/10.3969/j.issn.1672-9676.2019.17.039
Liang H (2020) The effect of antenatal perineal massage combined with Kegel exercise on the delivery outcome of primipara. Nurs Pract Res 17(18):101–103. https://doi.org/10.3969/j.issn.1672-9676.2020.18.039
Hu Z, Qi GH, Wu YH (2014) The effect of continuous guidance of pelvic floor muscle exercise on the maternal and infant delivery outcome of primipara. Hainan Medicine 25(09):1351–1352
Kovacs GT, Heath P, Heather C (2004) First Australian trial of the birth-training device Epi-No: a highly significantly increased chance of an intact perineum. Aust N Z J Obstet Gynaecol 44(4):347–348. https://doi.org/10.1111/j.1479-828X.2004.00265.x
Wang M, Zhang HH (2017) The application effect of perineal massage combined with Kegel exercise in the natural delivery of primipara in the third trimester of pregnancy. Nurs Res 31(33):4243–4246. https://doi.org/10.3969/j.issn.1009-6493.2017.33.017
Acknowledgements
This research not supported by any institution or individual.
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Contributions
XC: the conception of the work, the acquisition, analysis, and interpretation of data for the work, draft and revise the work. QYY: the conception of the work, the acquisition, analysis, and interpretation of data for the work. QW: the conception of the work, the acquisition, analysis, and interpretation of data for the work, revise the work. SH: the design of the work, the acquisition, analysis, and interpretation of data for the work. LH: the conception of the work, the acquisition, analysis, and interpretation of data for the work, revise the work. MS: the conception of the work, the acquisition, analysis, and interpretation of data for the work. HL: the conception of the work, the acquisition, analysis, and interpretation of data for the work, revise the work. CW: the conception of the work, the acquisition, analysis, and interpretation of data for the work. YW: the conception of the work, the acquisition, analysis, and interpretation of data for the work. LX: the design of the work, the acquisition, analysis, and interpretation of data for the work, revise the work. XL: the design of the work, revise the manuscript, final approval of the version to be published. JT: the design of the work, revise the manuscript, final approval of the version to be published. LG: the conception and design of the work, revise the manuscript, final approval of the version to be published, coordinate the overall work. CL: t the conception and design of the work, revise the manuscript, final approval of the version to be published, coordinate the overall work.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have not disclosed any competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cao, X., Yang, Q., Wang, Q. et al. PFMT relevant strategies to prevent perineal trauma: a systematic review and network meta-analysis. Arch Gynecol Obstet 308, 387–401 (2023). https://doi.org/10.1007/s00404-022-06769-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-022-06769-w