Abstract
It is thought that antenatal pelvic floor muscle training (PFMT) might produce a strong pelvic floor resulting in prolonged labour, whilst some believe it produces well-controlled muscles that facilitate rotation of the foetal head and shortens the duration of labour. This secondary analysis (of a previously published randomised controlled trial) assesses the labour and delivery details of 268 primigravidae who were originally randomised at approximately 20 weeks gestation to supervised PFMT or a control group. Between the two groups, there was no difference in the duration of the second stage of labour or in the need for instrumental delivery. PFMT does not appear to facilitate or obstruct labour.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many women are encouraged to train their pelvic floor muscles after delivery because there is evidence suggesting that this might prevent urinary incontinence in the short-term [1]. However, there have been different views regarding the effects of antenatal pelvic floor muscle training (PFMT) on labour and delivery. Anecdotal evidence suggests that an excessively strong pelvic floor might obstruct labour and result in perineal trauma that negate the beneficial effects of antenatal PFMT [2]. Others believe that it produces flexible, well-controlled muscles that can facilitate labour and reduce the need for instrumental delivery [3].
Few studies have assessed the possible effects of PFMT on the outcome of labour. One prospective study of 86 women found no difference in the course of delivery or the frequency of complications between those who trained their pelvic floor muscles antenatally and those who did not [4]. Another secondary analysis of a randomised controlled trial of antenatal PFMT has shown that a structured training programme in un-selected primigravidae seems to facilitate rather than obstruct labour [5]. PFMT was found to be associated with fewer cases of active pushing in the second stage of labour of more than 60 min compared with controls, although the total duration of the second stage was not significantly shorter in the training group [5].
This current study, a secondary analysis of a randomised controlled trial of antenatal PFMT [6], aims to assess whether supervised PFMT has an effect on the outcome of labour in a population of at-risk primigravidae with antenatal bladder neck mobility (BNM) [7].
The primary outcome of the original study was the incidence of post-partum stress urinary incontinence (SUI) at 3 months. A significant reduction in the incidence of post-partum urinary incontinence was seen in women allocated to the PFMT group (19.2%) compared with the un-treated controls (32.7%; p < 0.023) [6]. This secondary analysis assesses the effects of PFMT on the duration of the second stage of labour and on the mode of delivery and whether the data are consistent with those of a similar randomised controlled trial [5]. Local ethical approval was granted.
Materials and methods
Primigravidae with BNM on perineal ultrasound attending the antenatal clinic at hospital booking (approximately 20 weeks) were allocated to 1 of the 2 study groups. Two hundred and sixty-eight participants were randomised to either supervised PFMT with a physiotherapist at monthly intervals from 20 weeks until delivery or to an un-treated control group where they received the usual verbal advice on PFMT from their midwives.
The supervised PFMT regimen comprised 3 repetitions of 8 contractions each held for 6 s with 2 min rest between repetitions. These were repeated twice daily. Patients were also instructed to contract the pelvic floor every time when coughing or sneezing. At 34 weeks gestation, the number of contractions per repetition was increased to 12. Those un-able to follow this regimen due to the inability to contract the pelvic floor had individualised programmes until they could follow the study regimen. The regimen was the one advocated by Bo [8] and similar to that recommended by the 2nd International Consultation on Incontinence [9].
Compliance in the training group was monitored using diaries to record the number of daily exercises performed from 20 weeks to delivery. According to the amount of data recorded, the training group was categorised into 3 sub-groups; participants who kept no diary data (n = 52), those who had data for <28 days (n = 13) or those who had recorded ≥28 days (n = 55) of PFMT antenatally. The control group did not keep a formal record of any un-supervised exercises/PFMT they might have been undertaking. However, as part of the history recorded at each visit, each woman was asked if she was doing any pelvic floor exercises, and if so, how frequently.
The primary outcome measure was the duration of the second stage of labour (total and active) and the incidence of instrumental deliveries (forceps or vacuum) in the two groups. The total duration of the second stage of labour was defined as the period starting at full cervical dilatation and ending with delivery of the baby. The duration of the active (pushing) phase of the second stage was recorded as well.
Comparisons using the original group assignments (intervention or control) were made using non-parametric methods; Mann–Whitney’s test for the labour durations because these data were skewed; independent t-tests for head circumference and birth weight and χ 2-tests for all other comparisons. Statistical significance was set as p < 0.05.
Results
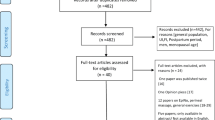
The flow of participants in the study is presented in Fig. 1. All were primigravidae with a median age of 28 years (ranging from 16 to 47 years). The demographic characteristics of the participants in the PFMT group were comparable to those in the control group regarding age (27 vs 29 years), body mass index (24.9 vs 24.1), pelvic floor strength (9.5 vs 10.4 cmH2O; as measured by perineometry at 20 weeks) and the presence of BNM >10 mm (25% vs 29%; as measured by perineal ultrasound scan at 20 weeks) [6].
There was no significant difference between the 2 groups regarding the epidural rate (51.7% vs 48%; p = 0.32), episiotomy rate (30.9% vs 31%; p = 0.41) or degree of perineal trauma (46.8% vs 56.9%; p = 0.21). There was one third-degree tear in each group.
Mode of delivery
Caesarean section (CS) rates were comparable between the 2 groups. Of the 22 (16.3%) participants in the PFMT group who delivered by CS, 17 were in labour (first or second stage). The control group showed similar figures with 17 (13.6%) participants delivering by CS (of which 15 were performed during labour). After excluding those who had CS (n = 39), vaginal breech deliveries (n = 1) and those with no available data (n = 8), we examined the labour and delivery details of the 220 primigravidae who had a vaginal delivery of a single foetus in the cephalic presentation at term (112 in the PFMT group and 108 in the control group).
The rate of assisted vaginal delivery was similar in the two groups. Eighty-eight (78.6%) participants in the PFMT group had un-assisted deliveries (compared to 82 (75.9%) in the control group; p = 0.40) whilst 24 (21.4%) needed instrumental assistance (compared to 26 [24.1%] of the control group; p = 0.40). The induction of labour rates were not significantly different between the PFMT and the control groups (34 [30.4%] and 22 [20.4%], respectively, [p = 0.12]). However, there was a small but significant difference in birth weight and head circumference: the study group babies being larger than those of the control group. Participants in the PFMT group had babies with a mean birth weight of 3.41 kg (compared to 3.23 kg in the control group; p < 0.01) and a mean head circumference of 34.7 cm (compared to 34.2 cm in the control group; p < 0.01).
Duration of the second stage of labour
Table 1 compares the durations of labour between the two groups. The total duration of the second stage of labour was not significantly different between the two groups (p = 0. 87) nor was the median duration of the active (pushing) second stage (p = 0.89).
Thirty-nine (35.8%) participants in the PFMT group had an active phase of more than 60 min compared to 32 (30.5%) in the control group, but this difference was not significant (p = 0.47).
Discussion
Although PFMT during pregnancy might result in improved muscle control and flexibility, it does not appear to facilitate or obstruct labour or result in a higher incidence of prolonged labour or instrumental delivery compared with the controls. These data are consistent with the findings of Salvesen and Morkved [5] on the mean duration of the second stage between the two groups. This adds reassurance that antenatal PFMT does not adversely affect the course of labour (or the mode of delivery) in a selected population that has been shown to be at risk of post-partum SUI.
BNM has been suggested to be a surrogate marker of pelvic floor weakness and a possible limitation of the study is the participants not being representative of the general population of pregnant women. They were a high-risk group recruited to the study for the prevention of SUI. However, if BNM suggests a weak pelvic floor, then one would expect less resistance during labour. Nevertheless, strengthening those patients’ pelvic floor during pregnancy did not seem to have a deleterious effect on the outcome of labour despite the significant reduction in the incidence of post-partum SUI.
The two groups were not significantly different regarding epidural rate, episiotomy rate or degree of perineal trauma. Although the difference between the two groups regarding birth weight and head circumference has reached statistical significance (in favour of the PFMT group), this probably had little effect on the overall outcome.
Although the sample size calculation (initially designed for the detection of a target difference in post-partum SUI) was not repeated (as this is a secondary analysis), it is likely that studying the labour and delivery details of 214 subjects was reasonably sufficient to detect a major difference in the outcome. With that sample size, a 90% powered new study with 5% significance level would be able to detect a target difference of 15 min in the duration of labour (with a standard deviation of 30 min) and of 5% in the rate of instrumental deliveries (with a standard deviation of 10%).
In the original study [6], fewer women in the supervised PFMT group reported post-partum SUI suggesting a beneficial effect of training the pelvic floor. This difference was shown despite the fact that 23% of the women in the control group did claim to have carried out some form of PFMT during their pregnancy (un-supervised). Bo et al. [10] have described what they term the ‘avis effect’; the potential stimulus of the control subjects to carry out pelvic floor training (which they will have been advised to do by their midwives) by attending for pelvic floor strength and BNM measurements during the original study. However, any ‘exercises’ performed by participants in the control group were not assessed or supervised (unlike the study group) and it isn’t possible to know whether these were being performed correctly or not. Moreover, participants in the PFMT group who completed more than 28 days training had reported less post-partum SUI compared with the controls (who kept no diaries) and those who performed less than 28 days training. This not only suggests a causal relationship between the reporting of training frequency and the primary outcome but also demonstrates a certain level of compliance with supervised training within the PFMT group. The significant difference in the incidence of post-partum SUI between the two groups confirms the previous finding that supervised training is more effective in preventing post-partum SUI than mere verbal instruction [10]. Antenatal PFMT has been recommended by the 3rd International Consultation on Incontinence (ICI) [11] and the National Institute of Clinical Excellence (NICE) [12] as a form of prevention of post-partum SUI in primigravidae.
This is the second study to show no adverse effect of supervised antenatal PFMT on the outcome of labour and delivery. With enough evidence accumulated, pregnant women and their midwives can be re-assured that antenatal PFMT can prevent post-partum urinary incontinence whilst not increasing the risks of prolonged labour or operative deliveries.
References
Glazener C, Herbison P, Wilson P, MacArthur C, Lang G, Gee H, Grant A (2001) Conservative management of persistent postnatal urinary and faecal incontinence: randomised controlled trial. BMJ 323(7313):593–596
UK Midwifery Archives (2000) Does horse-riding affect the pelvic floor? http://www.radmid.demon.co.uk/pelvicfloor.htm (Accessed 12 March 2007)
University of Michigan Health System (2007) Exercises to help prepare your body for labour and delivery. http://www.med.umich.edu/obgyn/smartmoms/exercise. (Accessed 12 March 2007)
Nielsen CA, Sigsgaard I, Olsen M, Tolstrup M, Danneskiold-Samsoee B, Bock JE (1988) Trainability of the pelvic floor. A prospective study during pregnancy and after delivery. Acta Obstet Gynecol Scand 67(5):437–440
Salvesen KÅ, Mørkved S (2004) Randomised controlled trial of pelvic floor muscle training during pregnancy. BMJ 329(7462):378–380
Reilly ET, Freeman RM, Waterfield MR, Waterfield AE, Steggles P, Pedlar F (2002) Prevention of postpartum stress incontinence in primigravidae with increased bladder neck mobility: a randomised controlled trial of antenatal pelvic floor exercises. BJOG 109(1):68–76
King JK, Freeman RM (1998) Is antenatal bladder neck mobility a risk factor for postpartum stress incontinence? Br J Obstet Gynaecol 105(12):1300–1307
Bø K (1995) Pelvic floor muscle exercise for the treatment of stress urinary incontinence: an exercise physiology perspective. Int Urogynecol J 6:282–291
Wilson PD, Bo K, Nygaard I et al (2002) Conservative treatment for women. In: Abrams P, Cardozo L, Khoury S, Wein A (eds) Incontinence, 2nd International Consultation on Incontinence. Health Publications, Plymouth, p 581
Bo K, Talseth T, Holme I (1999) Single blind, randomised controlled trial of pelvic floor exercises, electrical stimulation, vaginal cones, and no treatment in management of genuine stress incontinence in women. BMJ 318(7182):487–493
Wilson PD, Hay-Smith J, Nygaard I et al (2004) Adult Conservative Management. In :Abrams P, Cardozo L, Khoury S, Wein A (eds) Incontinence, 3rd International Consultation on Incontinence. Health Publications, Plymouth, pp 867–869
National Institute of Clinical Excellence (NICE) (2006) The Management of Urinary Incontinence in Women, pp 50–53. http://www.nice.org.uk/guidance/CG40/guidance/pdf/English/download.dspx (Accessed 12 March 2007)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Agur, W., Steggles, P., Waterfield, M. et al. Does antenatal pelvic floor muscle training affect the outcome of labour? A randomised controlled trial. Int Urogynecol J 19, 85–88 (2008). https://doi.org/10.1007/s00192-007-0391-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-007-0391-z