Abstract
Purpose
To evaluate the effects of selective use of episiotomy on perineal trauma.
Methods
We performed a retrospective cohort study on consecutive vaginal deliveries from January 2010 to December 2016. From January 2010 to December 2011 episiotomy was performed liberally, based only on individual midwife/doctor’s decision. Since January 2012, a shared selective use of episiotomy policy has been introduced. To evaluate the range of perineal trauma in spontaneous second-degree perineal tears, a sub-classification of second-degree lacerations has been introduced dividing them into two sub-groups: A (smaller than the average episiotomy) and B (spontaneous vaginal tear larger than the average episiotomy). The primary outcomes were the incidence and type of perineal trauma, with the proportion of type A and type B second-degree spontaneous tears under a policy of selective episiotomy.
Results
Deliveries not exposed to selective use of episiotomy were 1583 (Group 1), those exposed to selective use of episiotomy were 6409 (Group 2). In Group 2 episiotomy rate decreased, and incidence of intact perineum, first- and second-degree lacerations increased. The incidence of third- and fourth-degree lacerations did not change. Spontaneous second-degree lacerations occurred in 19.4% and 36.8% of women in group 1 and 2, respectively. With a selective episiotomy policy, 88.3% of second-degree tears was classified as type A.
Conclusions
The selective use of episiotomy is clinically feasible and effective. This policy seems to be associated with a lower delivery-related perineal trauma as showed by the sub-classification, that could be a useful tool to monitor obstetric care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vaginal delivery is commonly accompanied by the trauma of the genital tract. A recent Cochrane Review [1] reports a very heterogeneous frequency of this kind of tears, with some estimates (that include episiotomy) indicating this occurs up to 85% of births [2]. Perineal trauma is classified into four degrees based on anatomic structures involved and severity of lacerations (Table 1) [3, 4]. Main complications of vaginal tears include bleeding, infection, dyspareunia and a prolonged hospital stay. Furthermore, in a small percentage of women, the vaginal and perineal tissues trauma can cause long-term problems such as pain, urinary fistula, urinary incontinence, rectal fistula, faecal incontinence, dyspareunia and pelvic organ prolapse [2].
Episiotomy is an intentional perineal incision performed to enlarge vaginal opening during the second stage of childbirth and has become the most common surgical procedure worldwide [1, 5, 6]. A routine use of episiotomy was proposed to prevent severe spontaneous lacerations (third and fourth-degrees) by enlarging the vaginal outlet and reducing vaginal soft tissue stretching and tension during childbirth [7,8,9]. As a consequence, the rate of episiotomy increased substantially during the first half of the twentieth century [1, 6]. However, routine use of episiotomy has been questioned, because of its own related complications and the possibility to cause unnecessary trauma. For these reasons, the selective use of episiotomy was proposed. According to this strategy, clinicians use their clinical judgement to determine the need for episiotomy, where the benefits outweigh the harms, in situations such as prolonged second stage of labour, shoulder dystocia, instrumental delivery, non-reassuring foetal heart rate and aiming to avoid severe perineal tear [10, 11].
Cochrane reviews [12, 13] failed to demonstrate a clear protective role of routine episiotomy, and a more recent Cochrane review [1] confirmed these results concluding that routine use of episiotomy has no benefits neither for the mother nor for the foetus and that selective episiotomy policies result in fewer incidence of severe trauma [1]. Moreover, in a recent Committee Opinion of the American College of Obstetrics and Gynaecology (ACOG), the rate of episiotomy in unassisted delivery was proposed as a possible marker of obstetric care quality [3].
A policy of selective use of episiotomy has been introduced in our Department since January 2012. The aim of this retrospective cohort study was to evaluate the effects of this strategy on perineal trauma. Moreover, to evaluate perianal trauma in the wide range of spontaneous second-degree tears, a sub-classification of second-degree lacerations has been introduced based on episiotomy extension.
Materials and methods
This is a retrospective cohort study on data about mothers, pregnancies, deliveries, and newborns of all deliveries from January 2010 to December 2016, that were prospectively recorded and collected in our labour ward’s database from January 2010. Perineal lacerations were described following the classification adopted by the Royal College of Obstetricians and Gynaecologists (Table 1) [4]. From January 2010 to December 2011 both midline and mediolateral episiotomy were performed, and indication for episiotomy was liberally based only on individual midwife/doctor’s decision, without a shared and uniform protocol and indications. Since January 2012, a new protocol based on the shared selective use of episiotomy policy has been introduced in our Department. The episiotomy was recommended in instrumental delivery, shoulder dystocia, and precipitous breech delivery. Conversely, midwife/doctors can opt for performing an episiotomy, according to their clinical judgment, only in situations where the literature suggests that episiotomy could confer some benefit such as imminent severe perineal rupture, prolonged second stage of labour and non-reassuring foetal heart rate [10, 11]. Only mediolateral technique has been used and the repair with an absorbable continuous unlocking suture has been introduced to fix episiotomies and vaginal tears [13, 14].
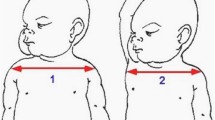
Second-degree lacerations sub-classification
The primary outcome was the change in incidence and grading of perineal trauma after the introduction of the selective use of episiotomy. However, second-degree lacerations comprise a wide range of lesions, from a minimal involvement to a massive damage of perineal muscles. To better evaluate the effects of selective use of episiotomy on the variable extension of second-degree tears, a sub-classification of second-degree lacerations has been introduced in our Obstetrics Unit since January 2012. The new sub-classification assumes that episiotomy involves the same anatomic structures of a second-degree laceration (perineal muscle, mucosa and skin) and divides them into two groups named A (spontaneous vaginal tear smaller than the average episiotomy) and B (spontaneous vaginal tear larger than the average episiotomy) based on the strict criteria reported in Table 2. The aim of this sub-classification was to allow understanding whether introduction of selective use of episiotomy is associated with a spontaneous anatomic damage smaller or larger than episiotomy (therefore, potentially less or more long-term complications), resulting in an advantage or disadvantage for the patient. To standardize the classification, a form based on criteria reported in Table 2 was introduced in clinical records. Both the attending doctor and midwife were asked to independently fill the form to classify spontaneous second-degree tears as type A or type B. This information was prospectively collected in the database from its introduction in January 2012.
Data analysis
Data of all vaginal deliveries were retrieved, and all cases in which episiotomy was recommended according to our labour ward’s procedures (such as shoulder dystocia, operative delivery with vacuum extractor, and precipitous breech delivery) have been excluded. Moreover, we excluded all deliveries with at least one missed record.
To better define the effect of selective use of episiotomy, we considered and analysed routinely recorded data about risk factors for severe perineal lacerations. Factors like nulliparity and increased birthweight are independently associated with severe perineal tears; also epidural anaesthesia, labour induction, and labour augmentation are more common among women with perineal lacerations [15, 16]. Finally, different racial/ethnic groups have varying rates of severe perineal trauma, with Asian women comprising the highest proportion [17, 18].
Statistical analysis was performed using SPSS (Statistical Package for the Social Sciences) version 24 software (SPSS, Chicago, IL, USA). Data are reported as the mean and standard deviation (SD) or median and interquartile range (IQR) for quantitative variables as appropriate and percentage for qualitative ones. Non-normally and normally distributed variables were analysed using the Mann–Whitney U test and Student’s t test, respectively. Binomial data were analysed using the Chi-squared test. Multivariate analysis was performed to adjust for known predictors of perineal injury that were not equally distributed between the cases and historical controls. A two-tailed p value < 0.05 was considered statistically significant.
Results
From January 2010 to December 2016, there were a total of 13,894 deliveries of which 9782 vaginal deliveries, with a caesarean section rate of 29.6%. Among 9782 vaginal deliveries, 283 (2.9%) met the exclusion criteria for shoulder dystocia, operative delivery with vacuum extractor, or precipitous breech delivery; and 1507 (15.4%) were excluded because of at least one missed record. Therefore, 7992 vaginal deliveries were included the study population. From January 2010 to December 2011, the deliveries not exposed to selective use of episiotomy were 1583 (Group 1). From January 2012 to December 2016, the deliveries exposed to selective use of episiotomy were 6409 (Group 2). Table 3 shows the incidence of perineal trauma in the two groups. Chi-squared test shows a significant different distribution of perineal trauma incidence between Group 1 and Group 2 (p < 0.001). Post-hoc pairwise comparison analysis, reported in Table 3, shows that the incidence of severe perineal trauma (third and fourth-degree lacerations) was not significantly different between the two groups (p = 0.329 and p = 1). Conversely, episiotomy rate has significantly decreased in Group 2 (p < 0.001), showing the effects of selective use of episiotomy policies. Furthermore, the percentage of second-degree laceration was significantly higher in the selective use of episiotomy group (p < 0.001). Interestingly, in Group 2, 88.3% (2086/2362) of second-degree lacerations were classified as 2A, and only 11.7% (279/2362) were described as 2B. The incidence of first-degree lacerations, finally, was significantly lower in Group 1 (p < 0.001), while intact perineum was significantly more frequently diagnosed in Group 2 (p < 0.001). Data reported in Table 3 are presented in Fig. 1, which shows the incidence of perineal trauma among all the deliveries occurred in the observed period. The overall agreement between doctors and midwives in the evaluation of second-degree sub-classification was 96.2%.
Table 4 shows the general characteristics of the two populations, and mean maternal age was significantly higher in Group 2 (p < 0.001). Conversely, the incidence of labour induction (p = 0.006), acceleration with oxytocin (p < 0.001), use of fundal pressure (p < 0.001), and prevalence of multipara (p < 0.001) were higher in Group 1. On that basis, to reduce the possible bias due to differences between the two populations, we performed a logistic regression to investigate the effect of risk factors on incidence of severe lacerations (Table 5). The multivariate analysis in Table 5 shows that the incidence of severe perineal lacerations remained stable across the two groups (relative risk = 1.053, p = 0.915), even after adjustment for known risk factors such as parity, maternal age, ethnicity, gestational age, induced labour, use of fundal pressure, use of oxytocin and foetal weight at birth.
As confirmation of our results, we decided to select a sub-population of nulliparas, excluding all patients with risk factors for severe perineal trauma (Asian ethnicity, use of fundal pressure, acceleration or induction of labour with oxytocin). Table 6 shows the selected sub-population characteristics, and age resulted significantly higher in Group 2 (p = 0.001). Moreover, the incidence of induced labour remains significantly higher in Group 1 (p = 0.008), even after the exclusion of all patients induced with oxytocin. Table 7 shows the incidence of perineal trauma before and after selective use of episiotomy. Chi-squared test shows a significant different distribution of perineal trauma incidence between Group 1 and Group 2 (p < 0.001) in the sub-population. Post-hoc pairwise comparison analysis, reported in Table 7, confirms a significant decrease in episiotomy rate after 2012 (p < 0.001) and a significant increased rate of non-severe vaginal tears (first- and second-degree lacerations) (p < 0.001). Once again, the increase in second-degree lacerations, according to our classification, was mainly due to 2A-degree lacerations. The rate of intact perineum significantly increased in Group 2 (p < 0.001). The incidence of severe lacerations was not significant different across the two groups (p = 0.518 and p = 1). Figure 2 shows the incidence of perineal trauma among all the sub-population deliveries occurred in the observed period.
Discussion
Main findings
Our results show that after the introduction of a selective use of episiotomy there was a significant decrease in the total number of episiotomies, with an increase in the rate of first and second-degree perineal laceration without a concomitant increase in the third and fourth-degree ones. In this study, we attempted to objectively assess whether the increased rate of spontaneous second-degree tears associated with selective episiotomy translates into a more severe perineal trauma. Using our sub-classification, the increased rate of second-degree laceration with a selective episiotomy policy was actually due to the increased rate of type A tears. This finding, together with the increase rate of intact perineum, suggests that restrictive episiotomy use is associated with less perineal trauma.
Interpretation
During the annual revision of our labour ward data, we noticed a high incidence of episiotomy, especially when compared with available literature data. Therefore, we decided to introduce a policy of selective use of episiotomy, sharing a protocol with standardized indications of episiotomy and suture technique. Clinical situations in which our procedures recommend performing episiotomy are precipitous breech delivery and shoulder dystocia [19]. Even though there is not a unanimous agreement in literature [20,21,22], operative/instrumental delivery in our setting are usually managed with recommended episiotomy, considering evidence of higher risk of more severe perineal trauma [4, 15, 23,24,25,26,27,28]. Conversely, according to clinical judgment, episiotomy was allowed only in situations where the literature suggests that some benefit could be provided, such as imminent severe perineal rupture, prolonged second stage of labour and non-reassuring foetal heart rate [10, 11]. Since 2012 up to now, this systematic approach led to a reduction of episiotomy incidence, as shown by our results (from 44% 2010–2012 to 13.8% 2012–2016). This incidence could be considered satisfactory when compared with data reported from the most recent Cochrane review (which reports rates in the selective arm from different studies ranging from 8 to 59% with a median of 32%) [1]. This reduction, however, led to a gradual increase of intact perineum rate and did not determine an increase of severe perineal lacerations (third and fourth-grade). These findings do not only confirm literature data but also reflects that the episiotomy was used correctly by midwives and doctors.
At the same time, with a decreased episiotomy incidence a concomitant increase of spontaneous perineal lacerations was expected [1]. Our data confirmed that prevision, showing an increase in lacerations of first and second-degree. Conversely to first-degree lacerations involving only vaginal mucosa and/or skin, second-degree lacerations are a very heterogeneous group including different severity grades of perineal muscle involvement. Therefore, to better understand the clinical significance of this expected increase of less severe lacerations, we decided to introduce a sub-classification of second-degree perineal lacerations (2A and 2B), defined, respectively, as a perineal trauma less and more important than episiotomy (Table 2). Our data showed that the reduction in episiotomy incidence leads to an increase in 2A lacerations, which causes an anatomic damage less or even equal to an episiotomy, without increasing 2B lacerations over years.
Our preliminary data compared heterogeneous groups for well-known risk factors for perineal trauma, that could be a confounder. As a matter of fact, several studies [29,30,31,32] have shown that factors such as nulliparity, use of fundal pressure, oxytocin use, epidural analgesia, length of labour’s stages (severe tears more frequent when labour length is more than 18 h), Asian ethnicity, and foetal weight (risk of severe tears rises almost linearly with increasing birthweight, from around 0.5% in women whose babies weighed only 2000 g, to 5% in women whose baby weighed close to 5000 g) are associated with more severe perineal lacerations. Conversely, although advanced maternal age has been associated with adverse perineal outcome [33], different studies failed to show association between higher maternal age and obstetric anal sphincter injuries, especially among groups with same parity [29,30,31,32]. On that basis, we decided to perform a logistic regression analysis that showed an incidence of severe perineal lacerations stable across the two groups (relative risk = 1.053, p = 0.915), even considering risk factors for perineal trauma. To further confirm results, we performed the sub-analysis comparing two populations of nulliparous women and removing risk factors for severe perineal trauma (Table 7). Even in this sub-population the results remain the same both in term of chronological trend of episiotomy and perineal tears over years. We could not consider analgesia and length of labour’s stages because of paucity of data.
As previously mentioned, the reduction of the episiotomy rate in unassisted vaginal delivery could be considered a candidate measure of obstetric care quality [3]. Strategies similar to ours, based on education, performance feedback, shared classifications and uniformity of management have already proven effective in reducing the rate of episiotomies [34, 35]. In this scenario, although designed to assess perineal trauma, our sub-classification of second-degree lacerations could be considered a useful tool for internal revision of perineal outcome and correct use of episiotomy. Moreover, it is interesting to notice that a recent study, investigating the effect of perineal lacerations on pelvic floor function at 6 months postpartum, has demonstrated that the subgroup of women with deeper (> 2 cm) perineal trauma shown increased likelihood of perineal pain (15.5% vs 6.2%) and weaker pelvic floor muscle strength (61.0% vs 44.3%) compared with women with more superficial trauma [36]. Therefore, future researches could focus on possible clinical implication of this sub-classification, in particular to determine if a 2B laceration could lead to long-term pelvic floor disorder (such as dyspareunia, urinary incontinence, genital prolapse) that could negatively impact the quality of life. If this relation will be confirmed, different strategies and appropriate follow-up could be applied in case of 2B lacerations.
Strengths and limitations
Our study and the sub-classification of second-degree perineal lacerations have some limitations and biases. First of all, the changes in episiotomy and perineal trauma incidence following the introduction of a policy of selective use of episiotomy were observed in a context that started from a high rate of episiotomy. Therefore, our results cannot be directly translated in all the clinical settings, and further evidence is required to confirm these observations in clinics with a lower rate of episiotomy. Regarding the sub-classification, the diagnosis of 2A and 2B lacerations is operator-dependent and not blinded, since the operator that grades second-degree tear is who attended the delivery. Furthermore, the sub-classification of second-degree made only in group 2 and the only partial comparability of the two groups are further limits of our study. Moreover, we acknowledge the risk of introducing non-contemporaneous control bias as over time there may have been changing factors affecting controls. Even after adjustment, we cannot rule out residual confounders. Finally, the retrospective design remains a limit to be acknowledged. However, many aspects of patient management remained constant over time; this, together with a shared anatomical definition (Table 2), staff training, use of forms, prospective data collected in a standardized database, logistic regression analysis, sub-analysis with more comparable groups, and classification of lacerations by two operators (doctor and midwife) may be considered the main strengths of the study.
Conclusion
Our data show that the selective use of episiotomy, as supported by the literature, is clinically feasible. Moreover, the introduction of our new classification better defined that it does not worsen perineal trauma at birth, being associated with a trauma lower than episiotomy. We can suggest that this sub-classification could be clinically useful to define the severity of second-grade lacerations and could be a new tool to asses obstetric care and the correct use of episiotomy. Furthermore, possible future goals may be the research for differences in quality of life between women who underwent an episiotomy and those who developed spontaneous 2A and 2B vaginal tears, helping to understand if this classification could be also useful to plan a different long term follow up of these patients. Finally, our study shows that a systematic approach with shared procedures, definitions and audit leads to an implementation of the obstetric care.
References
Jiang H, Qian X, Carroli G, Garner P (2017) Selective versus routine use of episiotomy for vaginal birth. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD000081.pub3
Kettle C, Frohlich J (2011) Perineal care. BMJ Clin Evid 4:1401–1439
A College of Obstetricians-Gynecologists (2016) Practice bulletin no. 165: prevention and management of obstetric lacerations at vaginal delivery. Obstet Gynecol 128:1–15. https://doi.org/10.1097/AOG.0000000000001523
Royal College of Obstetricians and Gynaecologists (2015) The management of third- and fourth-degree perineal tears. Green-top guideline N.29. RCOG. https://www.rcog.org.uk/en/guidelines-research-services/guidelines/gtg29/
FIGO Safe Motherhood N Health (SMNH) Committee (2012) Management of the second stage of labor. Int J Gynecol Obstet 119:111–116. https://doi.org/10.1016/j.ijgo.2012.08.002
Graham ID, Graham DF (1997) Episiotomy counts: trends and prevalence in Canada, 1981/1982 to 1993/1994. Birth 24:141–147. https://doi.org/10.1111/j.1523-536X.1997.00141.pp.x
Cunningham F (1993) Conduct of normal labor and delivery. In: Cunningham FG, MacDonald PC, Gant NF, Leveno KJ, Gilstrap LC III editor(s). Williams Obstetrics 19th, 19th ed. Appleton and Lange, Norwalk , pp 371–93
Ould F (1767) A Treatise of Midwifery. J Buckland, London
Thacker SB, Banta HD (1983) Benefits and risks of episiotomy: an interpretative review of the English language literature, 1860–1980. Obstet Gynecol Surv 38:322–338
A College of Obstetricians-Gynecologists (2006) practice bulletin: episiotomy. Clinical management guidelines for obstetrician-gynecologists. Number 71. Obstet Gynecol 107:957–962
Melo I, Katz L, Coutinho I, Amorim MM (2014) Selective episiotomy vs. implementation of a non episiotomy protocol: a randomized clinical trial. Reprod Health 11:66–71. https://doi.org/10.1186/1742-4755-11-66
Carroli G, Mignini L (2009) Episiotomy for vaginal birth. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD000081.pub2
Kettle C, Dowswell T, Ismail KM (2012) Continuous and interrupted suturing techniques for repair of episiotomy or second-degree tears. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD000947.pub3
Kettle C, Dowswell T, Ismail KM (2010) Absorbable suture materials for primary repair of episiotomy and second degree tears. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD000006.pub2
Schmitz T, Alberti C, Andriss B et al (2014) Identification of women at high risk for severe perineal lacerations. Eur J Obstet Gynecol Reprod Biol 182:11–15. https://doi.org/10.1016/j.ejogrb.2014.08.031
Pergialiotis V, Vlachos D, Protopapas A et al (2014) Risk factors for severe perineal lacerations during childbirth. Int J Gynecol Obstet 125:6–14. https://doi.org/10.1016/j.ijgo.2013.09.034
Yeaton-Massey A, Wong L, Sparks TN et al (2015) Racial/ethnic variations in perineal length and association with perineal lacerations: a prospective cohort study. J Matern Fetal Neonatal Med 28:320–323. https://doi.org/10.3109/14767058.2014.916675
Landy HJ, Laughon SK, Bailit JL et al (2011) Characteristics associated with severe perineal and cervical lacerations during vaginal delivery. Obstet Gynecol 117:627–635. https://doi.org/10.1097/AOG.0b013e31820afaf2
A College of Obstetricians-Gynecologists (2017) Practice bulletin no. 178: shoulder dystocia. Obstet Gynecol 129:e123–e133. https://doi.org/10.1097/AOG.0000000000002043
Sagi-Dain L, Sagi S (2015) Morbidity associated with episiotomy in vacuum delivery: a systematic review and meta-analysis. BJOG 122:1073–1081. https://doi.org/10.1111/1471-0528.13439
A College of Obstetricians-Gynecologists (2015) Practice bulletin no. 154: operative vaginal delivery. Obstet Gynecol 126:e56–65. https://doi.org/10.1097/AOG.0000000000001147
A College of Obstetricians-Gynecologists (2015) Committee opinion no. 647: limitations of perineal lacerations as an obstetric quality measure. Obstet Gynecol 126:e108–111. https://doi.org/10.1097/AOG.0000000000001151
de Vogel J, van der Leeuw-van BA, Gietelink D et al (2012) The effect of a mediolateral episiotomy during operative vaginal delivery on the risk of developing obstetrical anal sphincter injuries. Am J Obstet Gynecol 206:404.e1–404.e5. https://doi.org/10.1016/j.ajog.2012.02.008
Jangö H, Langhoff-Roos J, Rosthøj S, Sakse A (2014) Modifiable risk factors of obstetric anal sphincter injury in primiparous women: a population–based cohort study. Am J Obstet Gynecol 210:59.e1–59.e6. https://doi.org/10.1016/j.ajog.2013.08.043
Räisänen S, Vehviläinen-Julkunen K, Cartwright R, et al (2012) Vacuum-assisted deliveries and the risk of obstetric anal sphincter injuries-a retrospective register-based study in Finland: vacuum extraction and OASIS. BJOG Int J Obstet Gynaecol 119:1370–1378. https://doi.org/10.1111/j.1471-0528.2012.03455.x
Gurol-Urganci I, Cromwell D, Edozien L, et al (2013) Third- and fourth-degree perineal tears among primiparous women in England between 2000 and 2012: time trends and risk factors. BJOG 120:1516–1525. https://doi.org/10.1111/1471-0528.12363
Lund NS, Persson LK, Jangö H et al (2016) Episiotomy in vacuum-assisted delivery affects the risk of obstetric anal sphincter injury: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol 207:193–199. https://doi.org/10.1016/j.ejogrb.2016.10.013
van Bavel J, Hukkelhoven CW, de Vries C et al (2018) The effectiveness of mediolateral episiotomy in preventing obstetric anal sphincter injuries during operative vaginal delivery: a 10-year analysis of a national registry. Int Urogynecol J 29:407–413. https://doi.org/10.1007/s00192-017-3422-4
de Castro V, Monteiro M, Pereira GM, Aguiar RA et al (2016) Risk factors for severe obstetric perineal lacerations. Int Urogynecol J 27:61–67. https://doi.org/10.1007/s00192-015-2795-5
Hirayama F, Koyanagi A, Mori R, et al (2012) Prevalence and risk factors for third- and fourth-degree perineal lacerations during vaginal delivery: a multi-country study: prevalence and risk factors of severe perineal laceration. BJOG 119:340–347. https://doi.org/10.1111/j.1471-0528.2011.03210.x
Baghurst PA, Antoniou G (2012) Risk models for benchmarking severe perineal tears during vaginal childbirth: a cross-sectional study of public hospitals in South Australia, 2002–2008: risk models for severe perineal tears. Paediatr Perinat Epidemiol 26:430–437. https://doi.org/10.1111/j.1365-3016.2012.01300.x
Ampt AJ, Ford JB, Roberts CL, Morris JM (2013) Trends in obstetric anal sphincter injuries and associated risk factors for vaginal singleton term births in New South Wales 2001–2009. Aust N Z J Obstet Gynaecol 53:9–16. https://doi.org/10.1111/ajo.12038
Kudish B, Sokol RJ, Kruger M (2008) Trends in major modifiable risk factors for severe perineal trauma, 1996–2006. Int J Gynaecol Obstet 102:165–170. https://doi.org/10.1016/j.ijgo.2008.02.017
Zhang-Rutledge K, Clark SL, Denning S et al (2017) An initiative to reduce the episiotomy rate: association of feedback and the hawthorne effect with leapfrog goals. Obstet Gynecol 130:146–150. https://doi.org/10.1097/AOG.0000000000002060
Kozhimannil KB, Karaca-Mandic P, Blauer-Peterson CJ et al (2017) Uptake and utilization of practice guidelines in hospitals in the United States: the case of routine episiotomy. Jt Comm J Qual Patient Saf 43:41–48. https://doi.org/10.1016/j.jcjq.2016.10.002
Lawrence L, Rebecca R, Noelle B et al (2016) The effect of perineal lacerations on pelvic floor function and anatomy at six months postpartum in a prospective cohort of nulliparous women. Birth 43:293–302. https://doi.org/10.1111/birt.12258
Benchimol EI, Smeeth L, Guttmann A et al (2015) The reporting of studies conducted using observational routinely-collected health data (RECORD) statement. PLOS Med 12:e1001885. https://doi.org/10.1371/journal.pmed.1001885
Funding
None.
Author information
Authors and Affiliations
Contributions
All the authors conform the International Committee of Medical Journal Editors (ICMJE) criteria for authorship, contributed to the intellectual content of the study and gave approval for the final version of the article. MF conceptualized the study. MF, FG and FP participated in designing the study. FP, CL, SG and ASL managed the dataset and performed statistical analyses. MF, RR, AC and FG gave advice regarding the statistical analyses and methodology. All authors contributed to the interpretation of the results, as well as to the writing and editing of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no proprietary, financial, professional or other personal interest of any nature in any product, service or company. The authors alone are responsible for the content and writing of the paper.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The design, analysis, interpretation of data, drafting and revisions conform the Committee on Publication Ethics (COPE) guidelines (https://publicationethics.org/) and the RECORD (reporting of studies conducted using observational routinely-collected health data) statement [37], available through the EQUATOR (enhancing the quality and transparency of health research) network (www.equator-network.org). The study was approved by the Institutional Review Board (IRB) of the University of Verona. The study was non-advertised, and no remuneration was offered to encourage patients to give consent for the collection and analysis of their data.
Informed consent
Informed consent for all the procedures and to allow data collection and analysis for research purpose was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Franchi, M., Parissone, F., Lazzari, C. et al. Selective use of episiotomy: what is the impact on perineal trauma? Results from a retrospective cohort study. Arch Gynecol Obstet 301, 427–435 (2020). https://doi.org/10.1007/s00404-019-05404-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-019-05404-5