Abstract
Purpose
To evaluate the impact of a selective use of episiotomy combined with Couder’s maneuver on the incidence of perineal tears in spontaneous term deliveries.
Methods
A comparative, retrospective, mono-centric study in a university maternity unit was designed and included all primiparous women who delivered spontaneously after 37 weeks of gestation in cephalic presentation. Two cohorts were studied, before and after the practice of Couder’s maneuver. In the first cohort, the ''OSE cohort'' only selective episiotomies were performed from January 2009 to December 2010. In the second cohort, from January 2016 to December 2017, the ''SEC cohort'' selective episiotomies combined with Couder’s maneuver were performed by midwives and obstetricians. The primary outcome was the type of perineal tears, according to the Royal College of Obstetricians and Gynaecologists (RCOG) classification.
Results
A total of 2081 patients were included: 909 patients in the OSE cohort and 1172 patients in the SEC cohort. Couder’s maneuver was performed in 59% of the SEC cohort. In the SEC cohort, there were an increase in the number of intact perinea (55% versus 63%, p < 0.001), a decrease in second-degree perineal tears (18% versus 11%, p < 0.001) and a decrease in labia minora tears (48% versus 37%, p < 0.001). The rate of obstetrical anal sphincter injuries was less than 1% in both cohorts (0.3% versus 0.5%, p = 0.7).
Conclusion
A selective use of episiotomy combined with Couder’s maneuver could reduce the incidence of perineal tears, particularly second-degree perineal tears, without increasing the rate of obstetrical anal sphincter injuries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevention of perineal tears and obstetric anal sphincter injuries (OASIS) is a priority for midwives and obstetricians during vaginal deliveries. According to Willer et al., 85% of vaginal deliveries are accompanied by perineal lesions causing pelvic floor disorder that can lead to medico-social-psychological repercussions [1, 2]. The levator ani muscle, the main component of the pelvic floor, is damaged in 13–36% of patients during vaginal delivery [3, 4]. Muscle damage of the perineal floor increases the risk of genital prolapse, pelvic pain and dyspareunia [3, 5].
Episiotomy has long been considered a method of preventing these lesions. However, the implementation of episiotomies has not been shown to reduce the number of OASIS occurrences [6, 7]. On the other hand, the failure to perform an episiotomy can increase the number of occurrences of first- and second-degree perineal tears [8, 9]. To prevent muscle damage during fetal head release, several obstetrical maneuvers may be performed during the release of the fetal head and fetal shoulders. Ritgen's maneuver [2] releases the fetal head in a progressive and controlled manner. However, it does not prevent severe perineal lesions [10]. During Couder’s maneuver, the operator assists the release of the anterior fetal arm when the deltoid impression appears under the symphysis. This maneuver reduces the diameter from the bi-acromial diameter to the acromio-thoracic diameter. The shoulder-releasing axis is reduced by almost three centimeters [3, 11]. The solicitation of the posterior perineum during the release of fetal shoulders is thus significantly reduced (Fig. 1). In the literature, no study has studied the impact of performing Couder’s maneuver and the use of selective episiotomies on the perineum.
The main objective of this study was to compare the impact of a selective episiotomy policy combined with Couder’s maneuver on the incidence of perineal tears in spontaneous vaginal term deliveries in primiparous women.
Methods
This study is a comparative retrospective study conducted in a university maternity unit that compares two independent cohorts of nulliparous patients undergoing spontaneous vaginal deliveries with a selective episiotomy policy before and after the introduction of the Couder’s maneuver: ''Selective episiotomy without Couder’s maneuver'' cohort (Only Selective Episiotomy i.e. OSE cohort) from 1 January 2009 to 31 December 2010 and ''Selective episiotomy combined with a Couder’s maneuver'' cohort (i.e. SEC cohort) from 1 January 2016 to 31 December 2017.
All primiparous women who gave birth after 37 weeks of amenorrhea, by spontaneous vaginal delivery of a singleton fetus in a cephalic presentation were included. The exclusion criteria were multiparous patients, premature deliveries, breech presentations, caesarean sections or requiring assistance with instrumentation, multiple pregnancies or intrauterine fetal deaths.
Couder’s maneuver has been regularly performed in our maternity unit since 2016 by obstetricians (senior and junior) and midwives. During the maneuver, the operator assists the release of the anterior fetal arm when the deltoid impression appears under the symphysis. The objective is to reduce the diameter from the bi-acromial diameter to the acromio-thoracic diameter. The maneuver involves the insertion of two fingers under the pubic symphysis, along the anterior fetal humerus to the elbow using the hand whose palmar side faces the ventral side of the fetus. Then, the operator pushes the fetal arm behind the fetus’s back, allowing the forearm to bend. The fetal hand is then released under the pubic symphysis, allowing the release of the anterior arm [12]. (Supplementary Figures 1 to 3; Movie 1).
Since the guidelines for clinical practice from the French College of Gynaecologists and Obstetricians in 2005, a selective policy of episiotomy has been implemented within our maternity unit. Episiotomy indications are rare. Episiotomies are only performed in case of non-progression of a cephalic presentation which fights against an extremely tonic perineum associated with severe abnormalities of the fetal heart pattern. Episiotomies are performed by making a mediolateral right incision at an angle of 60° [6].
In this study, the primary outcome was the type of perineal tears according to the Royal College of Obstetricians and Gynaecologists (RCOG) classification. The secondary outcomes were neonatal issues and traumatic lesions in newborns.
All information required to conduct this study was collected from the institution's records and electronic files by a single investigator. Most of the data were collected in birth reports, including whether a Couder’s maneuver or an episiotomy was performed, the presence or absence of a perineal lesion and the posterior perineal tears type identified according to the classification described by Sultan and adopted by the RCOG [13, 14]. We also took into account anterior perineal tears: labia minora and periurethral tears. For each patient, we collected her age at the time of delivery, her body mass index at the beginning of pregnancy and the total weight gain during pregnancy which were assessed when she entered the maternity unit. The following comorbidities were recorded: pre-existing hypertension or hypertension during pregnancy, gestational diabetes, preeclampsia and pregnancy cholestasis. We identified the fetal head position. For each newborn, the data were collected on the day of birth: the gestational age, weight, head circumference, sex, presence or absence of trauma to the upper limbs (clavicular or humerus fracture) and Apgar score at 5 min of life.
The various qualitative and quantitative data were collected anonymously. The statistical study was carried out using R software. Missing data were not replaced. Outliers were replaced by empty values before the database freeze. Qualitative data were compared using the Chi-squared test. For small numbers, Fisher’s exact test was applied. Student’s test was employed to compare quantitative variables. The significance threshold was set at a p value of less than 0.05.
Under French regulations, this study was exempt from institutional review board approval because it was an observational investigation using anonymized data from medical records. In our centre, women are systematically informed that obstetrical and neonatal data can be used for the evaluation of medical practices and are explicitly informed that they can sign an opposition form.
Results
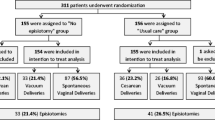
Over the two periods studied, 10,325 births were recorded (Fig. 2). In the first OSE cohort, 4606 births were recorded. Of these, 909 spontaneous vaginal deliveries in primiparous patients after 37 weeks of amenorrhea were analyzed, representing 19% of the total deliveries during this period. The episiotomy rate was 1.4% in this population. Couder’s maneuver had not been performed in any of these deliveries. In the second cohort, the SEC cohort, 5719 births were recorded. Of these, 1172 patients were included, representing 20.5% of the total number of births during this period, with the Couder’s maneuver being performed in 59% of the deliveries. The episiotomy rate in this second cohort was 0.4%.
The maternal characteristics of the two cohorts were comparable (Table 1). There were no statistically significant differences between the two groups. Obstetrical characteristics and delivery modalities were comparable (Table 2). There was no significant difference between the two cohorts in terms in fetal head position (occiput posterior delivery: 1.4% versus 1.3%, p = 0.5). It remains unknown in seven cases, because they were home births.
There was a statistically significant increase in the prevalence of intact perineum (55.4% in the OSE cohort versus 63.3% in the SEC cohort, p < 0.001) and a significant decrease in the rate of second degree perineal tears (18.4% in the OSE cohort versus 10.6% in the SEC cohort, p < 0.001) (Table 3). However, there was no statistically significant difference in the rate of first-degree perineal tears (25.9% in the OSE cohort versus 25.6% in the SEC cohort, p = 0.9) and in the rate of third-degree perineal tears (0.3% versus 0.5%, p = 0.7). There was no fourth-degree perineal tear. For anterior perineal tears, there was a statistically significant reduction in labia minora tears between the two groups (48.5% in the OSE cohort versus 36.65% in the SEC cohort, p < 0.001), but there was no significant difference in terms of periurethral tears (1.9% in both cohorts, p = 1). Episiotomy rates in the OSE and SEC cohorts were 1.4% and 0.4%, respectively (p = 0.017).
For upper limb trauma in newborns, the clavicular fractures rate was 0.55% in the OSE cohort and 0.17% in the SEC cohort (p = 0.2) (Table 4). No humeral fracture was diagnosed in both cohorts. Few newborns had an APGAR score of less than 7 at 5 min of life in either the selective episiotomy cohort alone (0.4%) and the selective episiotomy cohort associated with the Couder’s maneuver (0.3%), with no statistically significant difference (p = 0.7).
Discussion
This study performed before/after the introduction of a perineal protection policy illustrates the benefit of using the Couder’s maneuver combined with a selective use of episiotomy in protecting and preventing perineal tears during spontaneous term vaginal deliveries in nulliparous women. The Couder’s maneuver is not well described in the current literature.
The present study follows the practice study conducted in our center by Eckman et al. in 2007 which reported no increase in the rate of severe perineal tears with an episiotomy rate of 3.4% [7]. Subsequently, in 2013, Mottet et al. demonstrated, in a prospective comparative study in 199 nulliparous patients, a significant decrease in the rate of second-degree perineal tears due to the use of Couder’s maneuver [3]. In our series, Couder’s maneuver was performed in more than half of the deliveries (59%) in the OSE cohort. We have been teaching this maneuver since 2016 to all midwives and obstetricians. The period 2009–2010 was chosen for the first cohort rather than the year preceding the SEC cohort to avoid any bias related to the progressive implementation of Couder’s maneuver. We observed a new distribution of perineal tears related to this change in practices acquired for almost 3 years: a significant decrease by 8% in the rate of second-degree perineal tears accompanied by an increase by 8% in the number of intact perinea. These results can be explained by a decrease in the distension of the posterior perineum during the fetal head release as well as during the shoulder release. During a vaginal delivery, the release of the fetal head is the riskiest period for the perineum with a very important musculotendinous stretch, which can be multiplied by a factor of three [6].
From an anatomical point of view, the study led by Chantarasorn et al. showed an increase in mobility of the perineal body and the anorectal junction during vaginal deliveries [15]. During expulsion, the levator ani muscle can be damaged, and nerve damage often occurs [4]. Willer et al. found that this type of perineal trauma occurs in 80% of primiparous women [1]. It can cause many symptoms, such as anal or urinary incontinence, dyspareunia, and pelvic pain, and sometimes a significant impact on quality of life [1].
To protect the perineum and reduce the risk of obstetrical anal sphincter injuries, the French College of Gynaecologists and Obstetricians recommends manual control of the delivery of the cephalic presentation with a posterior perineal support [6]. In our maternity unit, the expulsion of the fetal head is progressive and manually controlled [16]. It is possible that delivery of the posterior shoulder could aggravate perineal tears or lead to an appearance of a perineal tear on a weakened perineum by fetal head release. For this reason, we teach and perform Couder’s maneuver, which reduces the diameter from the bi-acromial diameter to the acromio-thoracic diameter [3]. The tension on the posterior perineum is then reduced during shoulder release. Thus, Couder’s maneuver could reduce the impact of the shoulder delivery on the perineal body and on the levator ani muscle. In our study, the combination of a selective episiotomy policy and Couder’s maneuver could reduce the rate of second-degree perineal tears by a factor of 1.3.
Various techniques to protect the perineum during fetal expulsion have been reported in the literature, including in Cochrane reviews [2]. According to Aasheim, Ritgen's maneuver can reduce the number of first-degree perineal tears (RR = 0.32 IC at 95%[0.14; 0.69]) but it can induce an increase in the rate of second-degree perineal tears (RR = 3.25 IC 95%[1.73; 6.09]) [2]. During this maneuver, the fetal chin is lift anteriorly using fingers of one hand placed between the anus and the coccyx whereas the other hand controls the pace of the expulsion of the fetal.
Moreover, the study on perineal hyaluronic acid injection during the second stage of labor did not show any efficacy to reduce perineal trauma [17]. The prospective study conducted by Mottet et al. in 199 primiparous women was the first study to show a significant decrease in second-degree perineal tears: 8.9% of patients in the "Couder’s maneuver" group had second-degree perineal tears, and 29.6% in the control group had perineal tears (p < 0.001) [3].
In our study, the episiotomy rate was significantly lower in the SEC cohort than in the OSE cohort (1.43% versus 0.43%, respectively in the OSE and SEC cohorts with p = 0.017). In addition, the episiotomy rate, which was initially very low in our center according to the study by Eckman study (3.4% in 2007) is currently less than 1% [7]. This decreasing rate shows an improvement of our practices. Also, it may be due to the emergence of a new generation of midwives and obstetricians trained to perform episiotomies only when necessary.
Also, our study found a significant increase in the rate of intact perineum (55.4% in the OSE group compared to 62.4% in the SEC group, p < 0.001). Considering the discrepancy between the two groups, the combination of Couder’s maneuver with a selective use of episiotomies may have reduced the rate of second-degree perineal tears, increasing the number of intact perinea in primiparous patients during vaginal deliveries.
Various studies in the literature have reported an increase in the rate of intact perineum when an episiotomy was used restrictively. Ginod et al. found a significant decrease in the rate of second-degree perineal tears (13.5% in the non-episiotomy cohort versus 20.5% in the episiotomy cohort, p < 0.001) and a significant increase in the rate of first degree perineal lesions (42.1% in the non-episiotomy cohort versus 17.6% in the episiotomy cohort, p < 0.001). Moreover, the study did not show any increase in the number of the third- or fourth-degree perineal tears (0.73% and 0.14%, respectively, in the cohort without episiotomy versus 0.66 and 0.14%, respectively, in the cohort with episiotomies) [9]. Based on a meta-analysis conducted by Qian et al., selective episiotomies reduced the number of severe perineal lesions by 30% in 5977 patients who had vaginal deliveries whatever the parity [18]. In our study, there was no significant difference in the rate of first- and third-degree perineal tears (0.33% in the first cohort versus 0.51% in the second, p = 0.7). No fourth-degree perineal lesions were identified. Our low rate of episiotomy and third- and fourth-degree perineal tears may suggest the existence of unknown OASIS. In case of clinical doubt after vaginal delivery, a bi-manual perineal exam is performed. The use of ultrasound to identify an unknown OASIS after vaginal delivery is performed at a distance from birth if the patient reports functional signs suggesting this hypothesis. However, interest regarding this procedure in current practice remains limited. Indeed, only 5.6% of unknown OASIS are diagnosed by immediate postpartum ultrasound [19].
During anterior fetal shoulder release by Couder’s maneuver, the anterior perineum is placed under tension, and there is a high risk of labia minora tears. However, our study showed a significant reduction in the rate of labia minora tears (48.5% in the OSE cohort versus 36% in the SEC cohort, p < 0.0001). It seems that anterior perineum tears are generated by the fetal head and not by Couder’s maneuver. This result also takes into account our changing practices regarding fetal head release. In the first cohort, the OSE cohort, the cephalic pole release was performed according to the Ritgen’s maneuver. Hanging the chin increases the deflection around the pubic symphysis and the anterior perineum. In the SEC cohort, fetal head release was controlled with a posterior perineal support. The crowning of the baby’s head was manually controlled to maintain the flexion and the posterior perineum supported manually [16].
For newborns, no serious fractures have been described since the implementation of the Couder’s maneuver. For each delivery, there is a risk of a spontaneous clavicle fracture [11]. In our study, the fractures were exclusively clavicle fractures without a statistically significant difference in the rate of the fractures between the two groups (0.55% in the OSE cohort versus 0.17% in the SEC cohort, p = 0.2). Fractures do not seem to be linked to Couder’s maneuver. However, the risk of humeral fracture with the Couder’s maneuver exists mainly in untrained teams. It seems essential to benefit from complete training, whether through theoretical teaching, video learning, and simulation training before systematically performing Couder’s maneuver [20].
The strengths of this study are its originality and its large number of patients included in each cohort. To our knowledge, no study in the literature accurately describes Couder’s maneuver, and no work has reported any beneficial results of the maneuver in preventing perineal tears. The main limitation of this study are its monocentric and retrospective aspects. Thus, the study population is limited to nulliparous women giving birth after 37 weeks by vaginal delivery to a child with a cephalic presentation. This population is a low-risk population.
Instrument-assisted deliveries were voluntarily excluded to eliminate a confusion of bias associated with the use of an instrument, including vacuum extractors, forceps or spatulas. Hulot et al. studied the impact of Couder’s maneuver during vacuum-assisted vaginal delivery on perineal tears. They showed a significant decrease in the rate of second-degree perineal tears (42.4% in the vacuum-assisted without Couder’s maneuver cohort versus 15% in the vacuum-assisted combined with Couder’s maneuver cohort, p < 0.001) and a significant increase in the rate of intact perineum (34.1% versus 54.7%, p < 0.001) [21].
Birthing professionals could underestimate perineal tears evaluation either by simple ignorance or by concern for the outcome. There may have a measurement bias.
Conclusion
The prevention of perineal tears should not be limited to the control of the fetal head delivery. Shoulder delivery also remains a situation with a risk of perineal tears. Our study, which was conducted in line with the recommendations for clinical practice from the French College of Gynaecologists and Obstetricians, supports the interest of a selective policy of episiotomies associated with the use of Couder’s maneuver during vaginal deliveries. This evolution of practices may lead to a significant reduction in the rate of second-degree perineal tears by 8% and an increase in the rate of intact perineum by 8%, without an increase of obstetrical anal sphincter injuries. Couder’s maneuver should be taught to all midwives to avoid, as much as possible, perineal muscle tears responsible for urinary and anal incontinence, dyspareunia and pelvic pain, which may affect the quality of life.
References
Willer H, Aabakke AJ, Krebs L (2014) The effect of primary delivery of the anterior compared with the posterior shoulder on perineal trauma: a study protocol for a randomized controlled trial. Trials 15:291
Aasheim V, Nilsen ABV, Reinar LM, Lukasse M (2017) Perineal techniques during the second stage of labour for reducing perineal trauma. Cochrane Database Syst Rev 6:CD006672
Mottet N, Bonneaud M, Eckman-Lacroix A, Ramanah R, Riethmuller D (2017) Active delivery of the anterior arm and incidence of second-degree perineal tears: a clinical practice evaluation. BMC Pregnancy Childbirth 17:141
Bortolini MaT, Drutz HP, Lovatsis D, Alarab M (2010) Vaginal delivery and pelvic floor dysfunction: current evidence and implications for future research. Int Urogynecol J 21:1025–1030
Rathfisch G, Dikencik BK, Kizilkaya Beji N, Comert N, Tekirdag AI, Kadioglu A (2010) Effects of perineal trauma on postpartum sexual function. J Adv Nurs 66:2640–2649
Ducarme G, Pizzoferrato AC, de Tayrac R, Schantz C, Thubert T, Le Ray C et al (2018) Perineal prevention and protection in obstetrics: CNGOF clinical practice guidelines. J Gynecol Obstet Hum Reprod 48:455–460
Eckman A, Ramanah R, Gannard E, Clement MC, Collet G, Courtois L et al (2010) Evaluating a policy of restrictive episiotomy before and after practice guidelines by the French College of Obstetricians and Gynecologists. J Gynecol Obstet Biol Reprod (Paris) 39:37–42
Chehab M, Courjon M, Eckman-Lacroix A, Ramanah R, Maillet R, Riethmuller D (2014) Impact of a major decrease in the use of episiotomy on perineal tears in a level III maternity ward. J Gynecol Obstet Biol Reprod (Paris) 43:463–469
Ginod P, Khallouk B, Benzenine E, Desplanches T, Dub T, Schmutz E et al (2016) Assessment of restrictive episiotomy use and impact on perineal tears in the Burgundy’s Perinatal Network. J Gynecol Obstet Biol Reprod (Paris) 45:1165–1171
Aquino CI, Saccone G, Troisi J, Guida M, Zullo F, Berghella V (2019) Is Ritgen’s maneuver associated with decreased perineal lacerations and pain at delivery? J Matern-Fetal Neonatal Med Off J Eur Assoc Perinat Med Fed Asia Ocean Perinat Soc Int Soc Perinat Obstet. https://doi.org/10.1080/14767058.2019.1568984
Schaal JP, Riethmuller D, Maillet R, Uzan M (2002) Expulsions des présentations céphaliques. Mécanique Tech. Obstétricales. Sauramps Medical, pp 269–288
Schaal JP, Riethmuller D, Maillet R, Uzan M (2002) Dystocie des épaules : manoeuvres. Mécanique Tech. Obstétricales. Sauramps Medical, pp 529–536
Royal College of Obstetricians and Gynaecologists. Third- and Fourth-degree Perineal Tears, Management (Green-top Guideline No. 29). R Coll Obstet Gynaecol 2015
Sultan AH (1999) Obstetric perineal injury and anal incontinence. Clin Risk 5:193–196
Chantarasorn V, Shek KL, Dietz HP (2012) Mobility of the perineal body and anorectal junction before and after childbirth. Int Urogynecol J 23:729–733
Riethmuller D, Ramanah R, Mottet N (2018) Fetal expulsion: which interventions for perineal prevention? CNGOF Perineal Prevention and Protection in Obstetrics Guidelines. Gynécologie Obstétrique Fertil Sénologie 46:937–947
Zhou F, Wang XD, Li J, Huang GQ, Gao BX (2014) Hyaluronidase for reducing perineal trauma. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD010441.pub2
Jiang H, Qian X, Carroli G, Garner P (2017) Selective versus routine use of episiotomy for vaginal birth. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD000081.pub3
Thubert T, Cardaillac C, Fritel X, Winer N, Dochez V (2018) Definition, epidemiology and risk factors of obstetric anal sphincter injuries: CNGOF Perineal Prevention and Protection in Obstetrics Guidelines. Gynecol Obstet Fertil Senol 46:913–921
Naidu M, Sultan AH, Thakar R (2017) Reducing obstetric anal sphincter injuries using perineal support: our preliminary experience. Int Urogynecology J 28:381–389
Hulot G, Ramanah R, Riethmuller D, Mottet N (2019) The impact of active delivery of the anterior arm during vacuum-assisted vaginal delivery on perineal tears: a clinical practice evaluation. J Matern Fetal Neonatal Med. https://doi.org/10.1080/14767058.2019.1571573
Author information
Authors and Affiliations
Contributions
ABM, AEL and DR had the idea for the original cohort study and, with PLF, ML, RR and NM carried out the design of the study. PLF collected the data. PLF, ABM, ML and NM analysed/interpreted the data and produced the first draft. PLF and ML carried out statistical analysis. All authors read, revised and approved the submitted version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The author declares that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 52780 kb)



Rights and permissions
About this article
Cite this article
Forey, PL., Lallemant, M., Bourtembourg-Matras, A. et al. Impact of a selective use of episiotomy combined with Couder’s maneuver for the perineal protection. Arch Gynecol Obstet 302, 77–83 (2020). https://doi.org/10.1007/s00404-020-05572-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05572-9