Abstract
Purpose
To investigate the real-life epidemiology of mental disorders during pregnancy and their impact on birth outcome in an unselected low-risk population in Germany.
Methods
Claims data of the Techniker Krankenkasse (TK) were analyzed as part of a retrospective observational study over a one-year period from 01/2008 to 12/2008 including 38,174 pregnant women. ICD-10 codes were clustered into four diagnostic groups: depression, anxiety disorders, somatoform/dissociative disorders and acute stress reactions. The relationship between mental disorders, birth mode and infant weight was tested using chi-squared tests and multivariate logistic regression. Main outcome measures included the prevalence of mental disorders during pregnancy, performed cesarean sections and infants born underweight.
Results
N = 16,639 cases with at least one diagnosis from the four mental disorder diagnostic groups were identified: 9.3% cases of depression, 16.9% cases with an anxiety disorder, 24.2% cases with a somatoform/dissociative disorder, and 11.7% cases of acute stress reactions. Women diagnosed with a mental disorder were more likely to deliver their child by cesarean section ([depression: OR =1.26 (95% CI 1.14–1.39); anxiety: OR 1.11 (95% CI 1.02–1.19); somatoform disorders: OR 1.12 (95% CI 1.05–1.20); acute stress reactions: OR 1.17 (95% CI 1.07–1.28)]. Furthermore, infants of women diagnosed with an ICD-10 code for depression during pregnancy were more likely to be underweight and/or delivered preterm [OR =1.34 (95% CI 1.06–1.69)].
Conclusions
We observed substantially high prevalence rates of mental disorders during pregnancy which urgently warrant more awareness for validated screening and adequate treatment options.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pregnancy and puerperium are times of particular vulnerability, as many women exhibit symptoms of emotional distress during this period. Since hormonal changes increase the lifetime risk for affective disorders, the risk of depression is naturally higher in women during the childbearing years [1]. Furthermore, women can be affected by affective disorders in the perinatal period with no definite causal link to pregnancy and birth. These are referred to as perinatal mood disorders and comprise of depression, anxiety disorders, somatoform/ dissociative disorders or reactions to severe traumatic stresses and adjustment disorders.
Previous studies have focused mostly on maternal depression [2, 3, 4]. According to a systematic literature review, antenatal depression affects approximately 17% of women with the highest prevalence in the second and third trimesters of pregnancy [2]. Postpartum depression is a common but often overlooked diagnosis that affects approximately 10–15% of women in the postpartum period [3]. In comparison to classical depressive symptoms, a postpartum depression is characterized by emotional instability and insensitivity, or obsessive thoughts toward the newborn baby. These episodes begin within 4 weeks postpartum and may last up to one year [5]. Risk factors that have been identified include a previous history of depression, anger experience and expression, a lack of social support and a low socioeconomic status, stressful life events or pregnancy complications [6,7,8,9,10].
When a depressive episode is already present during pregnancy, it has been identified as a potential risk factor for subsequent postpartum depressive episodes and adverse perinatal outcomes. The literature suggests that there is an association between untreated depression or anxiety during pregnancy, and increased rates of preterm birth, low birth weight, infant growth impairment and behavioral disorders during childhood [11,12,13,14]. In spite of negative long-term effects for mother and offspring, studies showed that up to 86% of pregnant women suffering from mental disorders were not treated adequately due to the fear of possible teratogenic effects [15]. Moreover, the risk of relapse during pregnancy increases when drugs are discontinued [16,17,18,19,20].
Other psychiatric comorbidities have been less well studied. Maternal anxiety disorders have also become the focus of attention during the past few years [21], but other conditions, such as somatoform disorders, were not considered in previous research and consequently, only very little is known on prevalence rates and the potential impact on pregnancy.
Regarding the mode of delivery, cesarean section rates are on the rise worldwide: cesarean sections have become increasingly common in both developed and developing countries over the last decades [22, 23]. The causes of this increase often remain hidden and vary across countries and regions. In Germany, the percentage of cesarean deliveries has doubled in the last 25 years from 15.3% in 1991 to 30.5% in 2016 [24]. Substantial variation in cesarean section rates between the former eastern and western parts of Germany has also been observed [25].
The decision to perform a cesarean section is mainly based on the question of what is best for the mother and child. Therefore, the indications can be categorized into medically indicated or elective cesarean sections [22, 26, 27]. While the former indications are divided into absolute and relative indications, the latter are performed solely at the wish of the mother without a medical indication. In total, absolute indications are responsible for less than 10% of all deliveries by cesarean section in Germany [28, 29]. Thus, they are frequently performed for a relative indication in about 90% of the cases.
Due to improved surgical techniques, regional anesthesia and prevention of infections, the cesarean sections have lost its fright in the meantime [30, 31]. Yet, as with any surgery, cesarean sections are associated with short- and long-term complications for both mother and child. Apart from acute intraoperative risks, several complications are described for the postpartum period [32, 33] or subsequent pregnancies including placental anomalies, uterine rupture [34, 35] or risk of infertility [36,37,38,39]. Regarding neonatal outcomes, there is evidence for increased risks of bronchial asthma, type 1 diabetes mellitus or allergic rhinitis for babies delivered by elective cesarean section [40,41,42,43,44].
A number of factors have been discussed recently to explain the increasing cesarean section rates in Europe and worldwide. Late motherhood and changing risk profiles appear to have a substantial impact on rising rates [45,46,47,48,49]. According to the German Federal Statistical Office, the proportion of women giving birth at the age of 35 years or older ranges at over 20% [24]. Moreover, the prevalence of maternal obesity and gestational diabetes has strongly risen over the last decades leading to further possible sequelae [50,51,52,53].
Women with psychiatric comorbidities during pregnancy care more likely to deliver their baby by cesarean section, although in most cases clear medical indications are lacking [54]. It is argued that psychological distress may affect maternal confidence for delivery and hinder the progress of labor. Thus, pregnant women suffering from psychiatric disorders appear to have a lower pain threshold contributing to an increased frequency of cesarean delivery [54]. Regarding the increasing cesarean rates worldwide, a potential relationship between psychological distress and mode of delivery is of particular interest [55].
In fact, the consensus surrounding the indications for cesarean section has changed recently [56]. Psychological factors such as fear of vaginal birth, previous traumatic births, and other psychosomatic or psychiatric reasons are increasingly considered when deciding about the right mode of delivery.
Therefore, the primary aim of this study was to analyze reliable epidemiological data on the prevalence of mental disorders during pregnancy and their association to birth outcomes in Germany in a large unselected low-risk cohort.
Methods
Study design and population
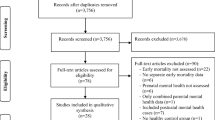
This report is part of a retrospective observational study performed by TK which aimed to investigate the medical care situation of women and their children prior to, during and after birth. The lager study focused on an analysis of the most prevalent secondary diagnoses associated with pregnancy and their influence on birth outcome and the offspring. The study was approved by the Federal Insurance Office of Germany (Bundesversicherungsamt) and is based on anonymized claims data of a cohort of female insurees who gave birth in 2008 and their children. The analyzes in this report were conducted on a subsample of 38.174 mothers, corresponding to the number of women who were insured at least four quarters before and seven quarters after the quarter of giving birth and whose data could be matched with the data of their child/children. As the children do not necessarily have the same insurance as their mothers, some were lost to follow-up. The matching rate was more than 80% of mothers and the matched sample sufficiently corresponded to the whole population in terms of age, cesarean section, and low birth weight (see Table 1).
Study variables
Mental disorders
Diagnoses from in-patient and out-patient data of our cohort of pregnant women were used to identify mental disorders one year prior to the quarter of delivery. Billing relevant coding in primary care as well as in specialist settings were taken as the basis for this claims data source. They were encoded by the International Statistical Classification or Diseases and Related Health Problems (ICD-10 German Modification). The Diagnoses according to ICD-10 were summarized in 4 groups: Depression, anxiety, somatoform disorders and acute stress reactions. Cases of depression were identified by ICD-10 codes F32–F33. Anxiety disorders were defined as ICD-10 codes F40–F41 and somatoform/dissociative disorders as ICD-10 Codes F44–F45, F48.1 and F68.0. ICD-10 codes F43 and F62 defined acute stress reactions. Therefore, we focused on the most prevalent mental disorders. There are other mental health disorders, which are important in maternal mental health, such as eating disorders, psychosis, drug/alcohol misuse disorders, and personality disorders. As they were coded in only a very small minority of women, we did not perform further analyzes with these groups.
Mode of delivery and birth weight
For hospital births, the mode of delivery was identified via G-DRG (German Diagnosis Related Groups System). G-DRGs are used in billing and contain information on patients' diagnoses and procedures performed during their hospital visit. In the G-DRG System of 2008 12 G-DRGs encoded births with a clear distinction between vaginal birth (G-DRGs O02A, O02B, O60A-O60D) and cesarean section (G-DRGS O01A-O01F). As cesarean sections are only performed in hospitals, outpatient and home births were defined as vaginal deliveries.
The G-DRG system does not systematically distinguish between pre-term and term deliveries. Owing to the lack of information, we decided to use the ICD-10 Codes P07 (preterm deliveries or birth weight below 2500 g) and P08.0 (birth weight above 4500 g) in hospital claims data as a proxy for gestational time of delivery. Reported birth weight of 2499 g and lower was defined as underweight, whereas more than 4500 g defined an overweight baby.
Statistical methods
All analyzes were performed using SAS version 9.3 (SAS Institute, Cary, NC, USA). Diagnostic data were examined regarding prevalence rates of mental disorders in association with mode of delivery and birth weight. First, the differences in the prevalence of mental disorders by birth mode and weight were tested using chi-squared tests. In the second step, adjusted odds ratios for the likelihood of cesarean section as well as low birth weight were calculated using multivariate logistic regression for each of the four mental disorder diagnostic groups. All models were controlled for age of the mother and residence at birth (East Germany vs. West Germany). As preterm delivery and cesarean section were shown to be highly correlated, odds ratios for cesarean section were additionally adjusted for birth weight and vice versa. Due to the explorative character of the study, all p values need to be interpreted descriptively.
Results
Prevalence of mental disorders
Among 38,174 pregnancies in 2008, there were 9.3% cases of depression, 16.9% cases with a diagnosis of an anxiety disorder, 24.2% cases with a somatoform/dissociative disorder, and 11.7% cases of acute stress reactions. The prevalence rates of mental disorders four quarters prior to delivery and sample characteristics are shown in Table 2.
Mode of delivery and birth weight
Women diagnosed with a mental disorder from one of the four diagnostic groups were more likely to deliver their child by cesarean section [depression: OR =1.26 (95% CI 1.14–1.39); anxiety: OR 1.11 (95% CI 1.02–1.19); somatoform disorders: OR 1.12 (95% CI 1.05–1.20); acute stress reactions: OR 1.17 (95% CI 1.07–1.28)]. Pregnant women suffering from any form of depression had the highest risk to deliver by cesarean section (OR 1.257) (see Fig. 1).
In the next step, the association between having a diagnosis of one of the four mental disorder diagnostic groups and giving birth to an underweight infant was examined. Altogether, there were 36,632 cases of infants with a normal birth weight (95.96%), and 1164 cases (3.05%) of infants coded with the ICD-10 code P07 (preterm deliveries or birth weight below 2500 g). In all, 378 infants were born overweight (0.99%). After performing the regression analysis, women who had a diagnosis of depression or acute stress reaction in at least one of the 4 quarters prior to delivery were significantly more likely to deliver an underweight infant or to deliver preterm with the highest Odds Ratio for the depression group [OR =1.337 (95% CI 1.06–1.69)] (see Table 3).
Discussion
So far, no epidemiological data for mental disorders during pregnancy have been provided by any database or registry. e hereby present claims data from more than 38,000 mother–child pairs and therefore an epidemiological profile of mental disorders during pregnancy in Germany for the first time. In the year 2008, 16,639 women with at least one diagnosis from the four mental disorder diagnostic groups during pregnancy were identified. In summary, we found 9.3% cases of depression, 16.9% cases with a diagnosis of anxiety disorder, 24.2% cases of somatoform/dissociative disorders and 11.7% cases of acute stress reactions.
Some of the prevalence rates confirm those reported in previous studies. Bennett et al. extracted prevalence rates for depression during pregnancy of 7.4%, 12.8%, and 12.0% for the first, second, and third trimesters, respectively [4]. Underwood et al. found an average rate of antenatal depression across several studies of 17% for prenatal and 13% for postnatal depression [2]. For perinatal anxiety, prevalence rates of depression were usually higher than the estimated depression rates at around 15% for prenatal and 11.1% for postnatal anxiety disorders, which is perfectly in line with our results [57, 58].
Considering other mental disorders, data on prevalence rates are sparse or simply do not exist. Regarding acute stress reactions in general, the authors found no available source that provide a prevalence rate during pregnancy. As we have found that 11.7% of patients were diagnosed with such a disorder, this result emphasizes the importance of our study as a first source for a general prevalence rate during pregnancy. When concentrating on sub-diagnosis in this group, post-traumatic stress disorder (PTSD) was most prevalent. Previous literature on PTSD has also shown very different prevalence rates of between 3.3% in community samples and 18.95% in high-risk samples [59]. These very different prevalence rates could be interpreted as being in line with our results, as our prevalence rate of 11.7% could symbolize the middle of these two extremes, which would reflect the unselected character of the low-risk population.
Furthermore, somatoform disorders have also been only sparsely studied during pregnancy. As one of the only studies, Sydsjö et al. found a prevalence rate of 5.9% in a sample of women who actively requested a cesarean section [60]. Hence, our data showed a surprisingly high prevalence of cases of somatoform or dissociative disorders (24.2%), which was not expected. This could be partly explained through the fact that this diagnostic group contained hypochondriacal disorders (ICD-10 F45.2), which is the diagnosis that could be coded for high pregnancy-or delivery-related anxiety. Another study, examining primary care settings in Germany in not-pregnant patients found a comparable prevalence of 28.5% of somatoform disorders [61]. The accumulation of SFD was higher in female patients than in males (RR 1.7), in particular when the number of children were > 1 (RR 1.8). The female–male difference was more marked in persistent somatoform pain disorder (RR 2.1) and unspecific somatization disorder (RR 5.0). Therefore, not only depression and anxiety, but also the diagnostic group of somatoform disorders during pregnancy should be the subject of future studies.
Considering birth outcome, our results showed that women diagnosed with any mental disorder from one of the four diagnostic groups were significantly more likely to deliver their child by cesarean section. Studies on the mode of delivery in association with psychiatric comorbidity are, again, sparse. Our findings are partly comparable to the findings of Sydsjö et al. [60]. Using the Swedish Birth Registry, they observed in a sample of 64,000 women that women who actively requested a cesarean section had a significantly higher psychiatric comorbidity than other women (10 versus 3.5%, p < 0.001). The authors concluded that this finding points to the need for psychological support for these women as well as the need to screen and treat psychiatric illness during pregnancy. In another study, the same study group found that psychiatric disorders after childbirth were also more common in women giving birth by cesarean section upon maternal request when compared to other women (11.2% vs 5.5%, p < 0.001). Additionally, an elective cesarean section increased the risk of psychiatric disorders after childbirth (OR 1.5, 95% CI 1.2–1.9). Hence, these results support the thesis that women who give birth by an elective cesarean section upon maternal request more often suffer from psychiatric disorders both before and after delivery. This indicates that these women represent a vulnerable group requiring special attention from obstetricians and general health-care providers and that this vulnerability should be taken into account when deciding on the mode of delivery.
As our results cannot show any causal direction, two interpretations are possible at this point. On the one hand, similar to the studies mentioned above, women with psychiatric comorbidity might request cesarean sections more actively than their healthy controls. On the other hand, health-care professionals might not know how to handle this specific patient group, advising more often cesarean sections, and therefore increasing the cesarean section rate. Future research should comprise the patients’ and the doctors’ motivation in this patient group.
Additionally, as another key result of our study, psychiatric comorbidity can have an impact on the offspring. Infants of women diagnosed with an ICD-10 code for depression during pregnancy were significantly more likely to be underweight and/or delivered preterm, as coded by the ICD-10. The literature concerning this specific association is controversial, however. Many studies examined the association between prenatal depression and preterm birth or low infant birth weight, explained through a pathway of cortisol activation, but they did not show a consistent picture. A systematic review and meta-analysis including 23 studies demonstrated that untreated depression during pregnancy was associated with significantly increased risks of preterm birth (odds ratio [OR], 1.56; 95% CI, 1.25–1.94) and low birth weight (OR, 1.96; 95% CI, 1.24–3.10) with a trend toward higher risks for exposure to more severe depression [62]. Grote et al. presented somewhat different results in their meta-analysis: They also found that women with depression during pregnancy were at increased risk for preterm birth and low birth weight, although the magnitude of the effect varied as a function of depression measurement, country location, and socioeconomic status [63].
The choice of whether to prescribe a psychotropic drug during pregnancy to prevent relapse or fetal exposure to maternal psychiatric illness is a difficult one. As mentioned above, untreated mental disorders during pregnancy may lead to adverse outcomes for mother and child. One the4 other hand, pregnant women who take psychopharmacological drugs have an increased risk of pregnancy complications such as abnormal bleeding during pregnancy, miscarriage, prematurity, preeclampsia, low birth weight, gestational diabetes and hypertension [15, 64,65,66]. Beyond that, negative side effects of psychotropic drugs on the offspring may include toxicity, withdrawal symptoms for the fetus, morphologic teratogenicity and breastfeeding risks [67,68,69,70].
Concerning this issue, our study showed that the use of psychotropic drugs was above average for all diagnostic groups of mental disorders. In summary, the risks stemming from psychopharmacological drug use during pregnancy must be balanced against the risks and long-term consequences of an untreated maternal mental disorder.
In conclusion, maternal depression and sometimes anxiety during pregnancy have begun to be recognized as factors that may adversely alter pregnancy outcomes [71]. However, so far, regarding the situation in Germany, clinical routine is far from being adapted to this patient group, as there is neither routine screening nor any special obstetric counseling. Representing one of the largest study samples that has ever been analyzed, our results emphasize the urgent need to adapt standard care.
Strengths and limitations
The key strength of our study is the large population-based database with comprehensive longitudinal data in a low-risk population. As we used claims data, we minimized the problem of selection bias among study participants. To date, there has been a gap in real-life data on mental disorders during pregnancy in Germany, and in studies globally. As such a database also implies several potential limitations, some aspects of our data have to be considered with caution. As billing-relevant coding was taken as the basis for this claims data source, we assumed correct codes for the diagnosis of all four mental disorder groups in primary care as well as in specialist settings. However, incomplete or incorrect coding cannot be ruled out completely. Owing to the large size of the TK birth cohort, covering nearly 10% of the German population in 2008, we assumed that our findings are sufficiently valid. In particular, diagnoses of mental disorders are not easily made and therefore, doctors frequently hesitate to code such a diagnosis. However, even if we assume that only half of the diagnoses were coded correctly, the numbers would still be impressive. Another limitation of claims data is that the scope of patients is limited to the insured patients only. As the TK is one of the largest German health insurance providers, covering more than 10% of the population, their members are representative for the country with a slight tendency towards more skilled professions requiring a higher education and to male insurants with a gender ratio of 1.04 (male:female) compared with 0.96 in the general population [72].
Conclusion
These data provide an important epidemiological profile of mental disorders during pregnancy in Germany. Claims data have the ability to complement data from research studies to generate a more complete and accurate view of people’s health problems. The tremendously high prevalence rates of mental disorders urgently warrant more awareness and a validated and systematic screening, which does not exist at the moment. The elevated risk of having a cesarean section in this group of patients indicates that these women are a vulnerable group requiring special attention from obstetricians and general health-care providers and that this vulnerability should be taken into account when deciding on the mode of delivery. Furthermore, pregnant women diagnosed with depression have a higher risk of giving birth preterm or having a child weighing less than 2500 g.
Antenatal depression should, thus, be identified through screening and should be treated. Hence, our data show that in the absence of national registries, health insurance data can provide a valuable instrument for epidemiological studies, and thus have the potential to improve the quality of standard care.
References
Gawlik S, Waldeier L, Muller M, Szabo A, Sohn C, Reck C (2013) Subclinical depressive symptoms during pregnancy and birth outcome–a pilot study in a healthy German sample. Arch Womens Ment Health 16(2):93–100. https://doi.org/10.1007/s00737-012-0320-0
Underwood L, Waldie K, D'Souza S, Peterson ER, Morton S (2016) A review of longitudinal studies on antenatal and postnatal depression. Arch Womens Ment Health 19(5):711–720. https://doi.org/10.1007/s00737-016-0629-1
Becker M, Weinberger T, Chandy A, Schmukler S (2016) Depression during pregnancy and postpartum. Curr Psychiatry Rep 18(3):32. https://doi.org/10.1007/s11920-016-0664-7
Bennett HA, Einarson A, Taddio A, Koren G, Einarson TR (2004) Prevalence of depression during pregnancy: systematic review. Obstet Gynecol 103(4):698–709. https://doi.org/10.1097/01.AOG.0000116689.75396.5f
Techniker Krankenkasse (2016) Geburtenreport - Eine Routinedatenanalyse zu Kaiserschnitt und Frühgeburt.
Lancaster CA, Gold KJ, Flynn HA, Yoo H, Marcus SM, Davis MM (2010) Risk factors for depressive symptoms during pregnancy: a systematic review. Am J Obstet Gynecol 202(1):5–14. https://doi.org/10.1016/j.ajog.2009.09.007
Martini J, Petzoldt J, Einsle F, Beesdo-Baum K, Hofler M, Wittchen HU (2015) Risk factors and course patterns of anxiety and depressive disorders during pregnancy and after delivery: a prospective-longitudinal study. (1573-2517 (Electronic))
Shakeel N, Eberhard-Gran M, Sletner L, Slinning K, Martinsen EW, Holme I, Jenum AK (2015) A prospective cohort study of depression in pregnancy, prevalence and risk factors in a multi-ethnic population. (1471-2393 (Electronic)). doi:D - NLM: PMC4310137 EDAT- 2015/01/27 06:00 MHDA- 2016/01/07 06:00 CRDT- 2015/01/25 06:00 PHST- 2014/05/07 [received] PHST- 2014/12/09 [accepted] AID - 10.1186/s12884-014-0420-0 [doi] AID - s12884-014-0420-0 [pii] PST - epublish
O'Hara MW, McCabe JE (2013) Postpartum depression: current status and future directions. Ann Rev Clin Psychol 9:379–407. https://doi.org/10.1146/annurev-clinpsy-050212-185612
Bruno A, Lagana AS, Leonardi V, Greco D, Merlino M, Vitale SG, Triolo O, Zoccali RA, Muscatello MRA (2018) Inside-out: the role of anger experience and expression in the development of postpartum mood disorders. J Maternal-Fetal Neonatal Med 31(22):3033–3038. https://doi.org/10.1080/14767058.2017.1362554
Szegda K, Markenson G, Bertone-Johnson ER, Chasan-Taber L (2014) Depression during pregnancy: a risk factor for adverse neonatal outcomes? A critical review of the literature. J Maternal Fetal Neonatal Med 27(9):960–967. https://doi.org/10.3109/14767058.2013.845157
Yonkers KA, Smith MV, Forray A, Epperson CN, Costello D, Lin H, Belanger K (2014) Pregnant women with posttraumatic stress disorder and risk of preterm birth. JAMA Psychiatry 71(8):897–904. https://doi.org/10.1001/jamapsychiatry.2014.558
Broekman BF, Chan Yh Fau - Chong Y-S, Chong Ys Fau - Kwek K, Kwek K Fau - Cohen SS, Cohen Ss Fau - Haley CL, Haley Cl Fau - Chen H, Chen H Fau - Chee C, Chee C Fau - Rifkin-Graboi A, Rifkin-Graboi A Fau - Gluckman PD, Gluckman Pd Fau - Meaney MJ, Meaney Mj Fau - Saw S-M, Saw SM (2014) The influence of anxiety and depressive symptoms during pregnancy on birth size. (1365-3016 (Electronic))
Grigoriadis S, VonderPorten Eh Fau - Mamisashvili L, Mamisashvili L Fau - Tomlinson G, Tomlinson G Fau - Dennis C-L, Dennis Cl Fau - Koren G, Koren G Fau - Steiner M, Steiner M Fau - Mousmanis P, Mousmanis P Fau - Cheung A, Cheung A Fau - Radford K, Radford K Fau - Martinovic J, Martinovic J Fau - Ross LE, Ross LE (2013) The impact of maternal depression during pregnancy on perinatal outcomes: a systematic review and meta-analysis. (1555-2101 (Electronic))
Vitale SG, Lagana AS, Muscatello MR, La Rosa VL, Curro V, Pandolfo G, Zoccali RA, Bruno A (2016) Psychopharmacotherapy in pregnancy and breastfeeding. Obstet Gynecol Surv 71(12):721–733. https://doi.org/10.1097/ogx.0000000000000369
Barnes TR (2011) Evidence-based guidelines for the pharmacological treatment of schizophrenia: recommendations from the British Association for Psychopharmacology. J Psychopharmacol Oxford Engl 25(5):567–620. https://doi.org/10.1177/0269881110391123
Gilbert PL, Harris MJ, McAdams LA, Jeste DV (1995) Neuroleptic withdrawal in schizophrenic patients. A review of the literature. Arch Gener Psychiatry 52 (3):173−188
Einarson A, Selby P, Koren G (2001) Discontinuing antidepressants and benzodiazepines upon becoming pregnant. Beware of the risks of abrupt discontinuation. Can Family Phys Med de famille Can 47:489–490
Viguera AC, Nonacs R, Cohen LS, Tondo L, Murray A, Baldessarini RJ (2000) Risk of recurrence of bipolar disorder in pregnant and nonpregnant women after discontinuing lithium maintenance. Am J Psychiatry 157(2):179–184. https://doi.org/10.1176/appi.ajp.157.2.179
Larsen ER, Saric K (2017) Pregnancy and bipolar disorder: the risk of recurrence when discontinuing treatment with mood stabilisers: a systematic review. Acta Neuropsychiatrica 29(5):259–266. https://doi.org/10.1017/neu.2016.60
Reck C, Zimmer K, Dubber S, Zipser B, Schlehe B, Gawlik S (2013) The influence of general anxiety and childbirth-specific anxiety on birth outcome. Arch Womens Ment Health 16(5):363–369. https://doi.org/10.1007/s00737-013-0344-0
Mylonas I, Friese K (2015) Indications for and risks of elective cesarean section. Dtsch Arztebl Int 112(29–30):489–495. https://doi.org/10.3238/arztebl.2015.0489
Betran AP, Torloni MR, Zhang JJ, Gulmezoglu AM (2016) WHO statement on caesarean section rates. BJOG 123(5):667–670. https://doi.org/10.1111/1471-0528.13526
Bundesamt Statistisches, (Destatis), (2017) Mehr Krankenhausentbindungen 2016 bei niedrigerer Kaiserschnittrate. Statistisches Bundesamt, Wiesbaden
Mikolajczyk RT, Schmedt N Fau - Zhang J, Zhang J Fau - Lindemann C, Lindemann C Fau - Langner I, Langner I Fau - Garbe E, Garbe E Regional variation in caesarean deliveries in Germany and its causes. (1471-2393 (Electronic)). doi:D - NLM: PMC3652783 EDAT- 2013/05/03 06:00 MHDA- 2013/12/16 06:00 CRDT- 2013/05/03 06:00 PHST- 2012/12/24 [received] PHST- 2013/04/24 [accepted] AID - 1471-2393-13-99 [pii] AID - 10.1186/1471-2393-13-99 [doi] PST - epublish
National Institute for Health and Clinical Excellence (2011) Caesarean section---NICE clinical guideline 132. 2nd edition
Deutsche Gesellschaft für Gynäkologie und Geburtshilfe (2010) Absolute und relative Indikationen zur Sectio caesarea (AWMF 015/054 (S1)) [derzeit in Überarbeitung]. https://www.dggg.de/fileadmin/documents/leitlinien/archiviert/federfuehrend/015054_Absolute_und_relative_Indikationen_zur_Sectio_caesarea/015054_2010.pdf. Accessed Aug 2010
Kolip P, Nolting H-D, Zich K (2012) Faktenchek Gesundheit Kaiserschnitt: Kaiserschnittgeburten - Entwicklung und regionale Verteilung. Gütersloh
AQUA (2015) Bundesauswertung zum Erfassungsjahr, (2014) 16/1 - Geburtshilfe Basisauswertung. Insitut für angewandte Qualitätsförderung und Forschung im Gesundheitswesen, Göttingen
Smaill FM, Grivell RM (2014) Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section. Cochrane Database Syst Rev 10:Cd007482. doi:https://doi.org/10.1002/14651858.CD007482.pub3
Bowring J, Fraser N, Vause S, Heazell AE (2006) Is regional anaesthesia better than general anaesthesia for caesarean section? J Obstet Gynaecol 26(5):433–434. https://doi.org/10.1080/01443610600720345
Karlstrom A, Lindgren H, Hildingsson I (2013) Maternal and infant outcome after caesarean section without recorded medical indication: findings from a Swedish case-control study. Bjog 120 (4):479-486. doi:https://doi.org/10.1111/1471-0528.12129. (discussion 486)
Arikan I, Barut A, Harma M, Harma IM, Gezer S, Ulubasoglu H (2012) Cesarean section with relative indications versus spontaneous vaginal delivery: short-term outcomes of maternofetal health. Clin Exp Obstet Gynecol 39(3):288–292
Riddell CA, Kaufman JS, Hutcheon JA, Strumpf EC, Teunissen PW, Abenhaim HA (2014) Effect of uterine rupture on a hospital's future rate of vaginal birth after cesarean delivery. Obstet Gynecol 124(6):1175–1181. https://doi.org/10.1097/aog.0000000000000545
Smith D, Stringer E, Vladutiu CJ, Zink AH, Strauss R (2015) Risk of uterine rupture among women attempting vaginal birth after cesarean with an unknown uterine scar. Am J Obstet Gynecol 213(1):80.e81–85. https://doi.org/10.1016/j.ajog.2015.01.056
Walfisch A, Beloosesky R, Shrim A, Hallak M (2014) Adhesion prevention after cesarean delivery: evidence, and lack of it. Am J Obstet Gynecol 211(5):446–452. https://doi.org/10.1016/j.ajog.2014.05.027
Lyell DJ (2011) Adhesions and perioperative complications of repeat cesarean delivery. Am J Obstet Gynecol 205(6 Suppl):S11–18. https://doi.org/10.1016/j.ajog.2011.09.029
Evers EC, McDermott KC, Blomquist JL, Handa VL (2014) Mode of delivery and subsequent fertility. Hum Reprod Oxford Eng 29(11):2569–2574. https://doi.org/10.1093/humrep/deu197
Gurol-Urganci I, Bou-Antoun S, Lim CP, Cromwell DA, Mahmood TA, Templeton A, van der Meulen JH (2013) Impact of Caesarean section on subsequent fertility: a systematic review and meta-analysis. Hum Reprod Oxford Engl 28(7):1943–1952. https://doi.org/10.1093/humrep/det130
Thavagnanam S, Fleming J, Bromley A, Shields MD, Cardwell CR (2008) A meta-analysis of the association between Caesarean section and childhood asthma. Clin Exp Allergy 38(4):629–633. https://doi.org/10.1111/j.1365-2222.2007.02780.x
Bager P, Wohlfahrt J, Westergaard T (2008) Caesarean delivery and risk of atopy and allergic disease: meta-analyses. Clin Exp Allergy 38(4):634–642. https://doi.org/10.1111/j.1365-2222.2008.02939.x
Papathoma E, Triga M, Fouzas S, Dimitriou G (2016) Cesarean section delivery and development of food allergy and atopic dermatitis in early childhood. Pediatric Allergy Immunol 27(4):419–424. https://doi.org/10.1111/pai.12552
Brandao HV, Vieira GO, de Oliveira Vieira T, Camargos PA, de Souza Teles CA, Guimaraes AC, Cruz AA, Cruz CMS (2016) Increased risk of allergic rhinitis among children delivered by cesarean section: a cross-sectional study nested in a birth cohort. BMC Pediatrics 16:57. https://doi.org/10.1186/s12887-016-0594-x
Cardwell CR, Stene LC, Joner G, Cinek O, Svensson J, Goldacre MJ, Parslow RC, Pozzilli P, Brigis G, Stoyanov D, Urbonaite B, Sipetic S, Schober E, Ionescu-Tirgoviste C, Devoti G, de Beaufort CE, Buschard K, Patterson CC (2008) Caesarean section is associated with an increased risk of childhood-onset type 1 diabetes mellitus: a meta-analysis of observational studies. Diabetologia 51(5):726–735. https://doi.org/10.1007/s00125-008-0941-z
Franz MB, Husslein PW (2010) Obstetrical management of the older gravida. Women's Health Lond Engl 6(3):463–468. https://doi.org/10.2217/whe.10.26
Guihard P, Blondel B (2001) Trends in risk factors for caesarean sections in France between 1981 and 1995: lessons for reducing the rates in the future. BJOG 108(1):48–55
Huang L, Sauve R, Birkett N, Fergusson D, van Walraven C (2008) Maternal age and risk of stillbirth: a systematic review. CMAJ Can Med Assoc J 178 (2):165-172. doi:10.1503/cmaj.070150
Cleary-Goldman J, Malone FD, Vidaver J, Ball RH, Nyberg DA, Comstock CH, Saade GR, Eddleman KA, Klugman S, Dugoff L, Timor-Tritsch IE, Craigo SD, Carr SR, Wolfe HM, Bianchi DW, D'Alton M (2005) Impact of maternal age on obstetric outcome. Obstet Gynecol 105(5 Pt 1):983–990. https://doi.org/10.1097/01.aog.0000158118.75532.51
Luke B, Brown MB (2007) Elevated risks of pregnancy complications and adverse outcomes with increasing maternal age. Hum Reprod Oxford Engl 22(5):1264–1272. https://doi.org/10.1093/humrep/del522
Voigt M, Zygmunt M, Henrich W, Straube S, Carstensen M, Briese V (2008) Analysis of subgroup of pregnant women in Germany. Geburtshilfe Frauenheilkd 68(08):794–800
Ehrenberg HM, Durnwald CP, Catalano P, Mercer BM (2004) The influence of obesity and diabetes on the risk of cesarean delivery. Am J Obstet Gynecol 191(3):969–974. https://doi.org/10.1016/j.ajog.2004.06.057
Gorgal R, Goncalves E, Barros M, Namora G, Magalhaes A, Rodrigues T, Montenegro N (2012) Gestational diabetes mellitus: a risk factor for non-elective cesarean section. J Obstet Gynaecol Res 38(1):154–159. https://doi.org/10.1111/j.1447-0756.2011.01659.x
Al-Qahtani S, Heath A, Quenby S, Dawood F, Floyd R, Burdyga T, Wray S (2012) Diabetes is associated with impairment of uterine contractility and high Caesarean section rate. Diabetologia 55(2):489–498. https://doi.org/10.1007/s00125-011-2371-6
Bayrampour H, Salmon C, Vinturache A, Tough S (2015) Effect of depressive and anxiety symptoms during pregnancy on risk of obstetric interventions. (1447-0756 (Electronic))
Kottmel A, Hoesli I, Traub R, Urech C, Huang D, Leeners B, Tschudin S (2012) Maternal request: a reason for rising rates of cesarean section? Arch Gynecol Obstet 286(1):93–98. https://doi.org/10.1007/s00404-012-2273-y
Stjernholm YV, Petersson K, Eneroth E (2010) Changed indications for cesarean sections. Acta Obstet Gynecol Scand 89(1):49–53. https://doi.org/10.3109/00016340903418777
Howard LM, Ryan EG, Trevillion K, Anderson F, Bick D, Bye A, Byford S, O'Connor S, Sands P, Demilew J, Milgrom J, Pickles A (2018) Accuracy of the Whooley questions and the Edinburgh Postnatal Depression Scale in identifying depression and other mental disorders in early pregnancy. Br J Psychiatry 212(1):50–56. https://doi.org/10.1192/bjp.2017.9
Reck C, Struben K, Backenstrass M, Stefenelli U, Reinig K, Fuchs T, Sohn C, Mundt C (2008) Prevalence, onset and comorbidity of postpartum anxiety and depressive disorders. Acta Psychiatr Scand 118(6):459–468. https://doi.org/10.1111/j.1600-0447.2008.01264.x
Yildiz PD, Ayers S, Phillips L (2017) The prevalence of posttraumatic stress disorder in pregnancy and after birth: a systematic review and meta-analysis. J Affect Disord 208:634–645. https://doi.org/10.1016/j.jad.2016.10.009
Sydsjo G, Moller L, Lilliecreutz C, Bladh M, Andolf E, Josefsson A (2015) Psychiatric illness in women requesting Caesarean section. BJOG 122(3):351–358. https://doi.org/10.1111/1471-0528.12714
Schoepf D, Heun R, Weiffenbach O, Herrmann S, Maier W (2003) The 4-week prevalence of somatoform disorders and associated psychosocial impairment. Der Nervenarzt 74(3):245–251. https://doi.org/10.1007/s00115-001-1241-8
Jarde A, Morais M, Kingston D, Giallo R, MacQueen GM, Giglia L, Beyene J, Wang Y, McDonald SD (2016) Neonatal outcomes in women with untreated antenatal depression compared with women without depression: a systematic review and meta-analysis. JAMA Psychiatry 73(8):826–837. https://doi.org/10.1001/jamapsychiatry.2016.0934
Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ (2010) A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry 67(10):1012–1024. https://doi.org/10.1001/archgenpsychiatry.2010.111
Andersen JT, Andersen NL, Horwitz H, Poulsen HE, Jimenez-Solem E (2014) Exposure to selective serotonin reuptake inhibitors in early pregnancy and the risk of miscarriage. Obstet Gynecol 124(4):655–661. https://doi.org/10.1097/aog.0000000000000447
Kjaersgaard MI, Parner ET, Vestergaard M, Sorensen MJ, Olsen J, Christensen J, Bech BH, Pedersen LH (2013) Prenatal antidepressant exposure and risk of spontaneous abortion - a population-based study. PLoS ONE 8(8):e72095. https://doi.org/10.1371/journal.pone.0072095
Palmsten K, Setoguchi S, Margulis AV, Patrick AR, Hernandez-Diaz S (2012) Elevated risk of preeclampsia in pregnant women with depression: depression or antidepressants? Am J Epidemiol 175(10):988–997. https://doi.org/10.1093/aje/kwr394
Kieviet N, Dolman KM, Honig A (2013) The use of psychotropic medication during pregnancy: how about the newborn? Neuropsychiatric disease and treatment 9:1257–1266. https://doi.org/10.2147/NDT.S36394
Coughlin CG, Blackwell KA, Bartley C, Hay M, Yonkers KA, Bloch MH (2015) Obstetric and neonatal outcomes after antipsychotic medication exposure in pregnancy. Obstet Gynecol 125(5):1224–1235. https://doi.org/10.1097/aog.0000000000000759
Veiby G, Daltveit AK, Engelsen BA, Gilhus NE (2014) Fetal growth restriction and birth defects with newer and older antiepileptic drugs during pregnancy. J Neurol 261(3):579–588. https://doi.org/10.1007/s00415-013-7239-x
Chisolm MS, Payne JL (2016) Management of psychotropic drugs during pregnancy. BMJ 352:h5918. https://doi.org/10.1136/bmj.h5918
Alder J, Fink N, Bitzer J, Hosli I, Holzgreve W (2007) Depression and anxiety during pregnancy: a risk factor for obstetric, fetal and neonatal outcome? A critical review of the literature. J Maternal Fetal Neonatal Med 20(3):189–209. https://doi.org/10.1080/14767050701209560
Meyer G, Neumann K, Badenhoop K, Linder R (2014) Increasing prevalence of Addison's disease in German females: health insurance data 2008–2012. Eur J Endocrinol 170(3):367–373. https://doi.org/10.1530/eje-13-0756
Acknowledgements
Techniker Krankenkasse kindly provided data for the analyzes.
Funding
This work was supported by the Institute of Women’s Health, Tübingen, Germany. They had no role in the design and conduct of the study; in the collection, analysis, the interpretation of the data; or in the preparation, review, or approval of the manuscript.
Author information
Authors and Affiliations
Contributions
SW, MG: study concept, interpretation of data, manuscript writing and editing. AL, AG, MS: study concept and design, data analysis, manuscript editing. MF: data analysis, manuscript writing. CS, MW: manuscript writing and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the Federal Insurance Office of Germany (Bundesversicherungsamt, Reference Number IT 5 - 8269 - 70/2014, approved on 16 January 2014).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wallwiener, S., Goetz, M., Lanfer, A. et al. Epidemiology of mental disorders during pregnancy and link to birth outcome: a large-scale retrospective observational database study including 38,000 pregnancies. Arch Gynecol Obstet 299, 755–763 (2019). https://doi.org/10.1007/s00404-019-05075-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-019-05075-2