Abstract
Purpose
To improve the outcome of fetuses with gastrochisis several studies evaluated prenatal predictors. But there are different guidelines established and therefore the prenatal care is not standardized. With our study we wanted to evaluate the outcome of fetuses with gastroschisis after modification of prenatal management strategies at the Department of Obstetrics and Gynecology of the University Hospital Münster.
Methods
In this explorative retrospective study of 39 fetuses with gastroschisis, we compare the clinical outcome between two management groups. In the first group (group 1, n = 14) prenatal indication for delivery was confirmed by a subjective evaluation of the small bowel diameter and the wall thickness without established cut-off values for these parameters. In the second group (group 2, n = 25) certain limits for the small bowel diameter (25 mm) and the wall thickness (2.5 mm) were used for fetal surveillance.
Results
Noticeable differences between the two groups regarding birth weight, weight centile, arterial pH, small bowel diameter, wall thickness, adverse bowel condition and re-operations could not be observed. In group 2, delivery was earlier (p = 0.011), and a lower rate of prenatal complications was observed (p = 0.016).
Conclusion
To avoid adverse prenatal complications we recommend the observation of fetuses with gastroschisis by sonographic monitoring of the small bowel diameter and the wall thickness.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Gastroschisis is a congenital defect of the abdominal wall with a herniation of intestinal contents. This wall defect is usually located on the right side of the umbilicus. The rate of incidence for gastroschisis has increased considerably in the past years, occurring in one in every 2000–5000 births [1].
A definitive cause for gastroschisis has not been found yet, however some risk factors that can increase the likelihood of incidence are known: young maternal age, a low BMI of the mother, consumption of vasoactive substances, as well as smoking are associated with a higher risk of gastroschisis [2–4].
There are different prenatal management strategies for fetuses with gastroschisis. Growth scan, umbilical artery Doppler ultrasound, cardiotocography and bowel measurements are methods to observe pregnancy. Fetuses with gastroschisis have a relevant risk for intrauterine fetal death.
Prenatal management is discussed controversially. Some studies reported that there is no correlation between bowel dilatation and neonatal outcome [5, 6]. On the other hand studies observed the opposite. Crawford et al. [7] found that bowel dilatation may be an indicator of either prenatal or intrapartum fetal distress. The study of Heinig et al. [8] reported that dilatation of the small bowel more than 25 mm in the third trimester of pregnancy was associated with an increased risk of short-term prenatal complications such as fetal distress or intrauterine fetal death.
The current study deals with diagnosis and outcome of fetuses with gastroschisis. The study was designed as a follow-up assessment after changing the prenatal management strategy of fetuses with gastroschisis as a consequence of the results of the publication of Heinig et al. [8].
The aim of the study was to compare the outcomes of fetuses with gastroschisis before and after the modification of prenatal management strategies.
Methods and materials
We performed an explorative, retrospective study of pregnant women with fetuses with prenatal diagnosed gastroschisis. We included all prenatal cases between October 2001 and January 2013 presented at the Department of Obstetrics and Gynecology, University Hospital of Münster. Cases without delivery in our hospital were excluded. All examination data were obtained from our electronic clinic database. The study was designed according to the Declaration of Helsinki and was approved by our institutional ethical review board.
The sample group of 39 affected cases was split into two groups. Group 1 consisted of 14 cases diagnosed between October of 2001 and September of 2005, group 2 consisted of 25 cases diagnosed between December of 2005 and January of 2013. Group 1 represented the cases of the study by Heinig et al. [8]. The findings in his study suggest an increased risk for complications at birth such as intrauterine fetal death or fetal distress if dilation greater than 25 mm or a wall thickness of more than 2.5 mm in the small intestine are present. On the basis of these findings, in group 2 the indication for urgent delivery at the same day was made.
We measured the same variables as Heinig et al. [8] to observe the condition of the intra- and extra abdominal bowel and to compare the two different management strategies. Therefore, the wall thickness of the small bowel was measured from outer wall to outer wall of the thickest part. The mean thickness was used if the bowel wall showed different thicknesses. The maximum bowel diameter was defined by the measurement from outer wall to outer wall of an extruded bowel loop at the most dilated segment (Fig. 1).
To compare the two groups the measurement data of the last presentation before delivery were recorded. All fetuses have been delivered by cesarean section. This is part of our hospital management guidelines. The fetuses were examined from 24th week of gestation in a 3 week interval by ultrasound. To assess fetal wellbeing, the fetal growth, the condition of the intra- and extra abdominal bowel, the fetal heart rate and the amniotic fluid volume were observed. Ultrasound intervals were reduced in case of abnormalities. Starting at the 30th week of gestation, weekly ultrasound assessments were performed. The gestational age was determined based on the results of early ultrasound screening. If no early data were available the last menstrual period date was used for calculation.
After delivery the newborns were observed in the neonatal intensive care unit. Depending on the bowel condition of the newborn, surgical intervention was performed, such as primary closure or “silo bag” procedure with a secondary closure. The results of the postnatal period have been taken from the neonatal clinical data base. The variable “re-operation” is defined as a recurrent surgical intervention in relation to the bowel condition over a 6 month period. The bowel condition was described as adverse if edema or a livid coloration were observed.
Statistical analysis
The two study groups were compared calculating absolute and relative frequencies, medians, and inter quartile ranges, where appropriate. Moreover, differences between the groups were assessed by Fisher’s exact test for binary variables and the Mann–Whitney U test for metric variables. Inferential statistics were intended to be exploratory (hypotheses generating), not confirmatory, so that neither a global significance level nor local levels were controlled. Thus, p values are to be interpreted in Fisher’s sense, as a measure of plausibility of the respective null hypothesis, and we denote small p values as noticeable instead of significant. Statistical analyses were performed using R, version 3.1.2. [21].
Results
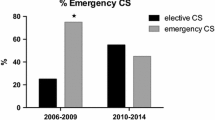
Thirty-nine cases of gastroschisis were included, 14 cases in group 1 and 25 cases in group 2. In both groups all fetuses were delivered by cesarean section. In the first group there was one emergency cesarean section because of fetal distress. No emergency cesarean section was observed in the second group. In all included cases no additional malformations or polyhydramnios were presented.
Table 1: baseline characteristics and outcomes present the baseline characteristics and outcomes of the two study groups. Differences between the groups could not be observed regarding the arterial pH (p = 0.747), the external bowel diameter (p = 0.202), the wall thickness of the small bowel (p = 0.464) and the frequency of re-operations (p = 0.686). However, noticeable differences could be observed regarding the gestational age of delivery (median group 1: 253 days, median group 2: 242 days, p = 0.011), the birth weight (median group 1: 2613 g, median group 2: 2230 g, p = 0.051), and the frequency of prenatal complications (group 1: 3 out of 14, group 2: 0 out of 25, p = 0.040). The results also suggest a possible difference between the two groups regarding the weight centile (median group 1: 45, median group 2: 24, p = 0.110) and the frequency of adverse bowel conditions (group 1: 3 out of 14, group 2: 1 out of 25, p = 0.123).
In group 1 three newborns showed adverse bowel conditions. In two cases, edema and a livid coloration of the bowel was noticed, and in the third case jejunal atresia was found. Three children in group 1 had reoperations because of bowel complications, two of them because of bowel obstruction, and one for extensive necrosis of residual small bowel. In group 2 one newborn had adverse bowel conditions. In this case the bowel showed edema and was inflammatorily affected. Reoperations due to bowel complications were necessary in four cases. Two of them needed surgery due to an ileus and two newborns needed ileostoma revision operation.
Discussion
To our knowledge, this is the first study that observes an improved outcome of fetuses with gastroschisis after modification of the prenatal management strategies by changing the sonographic observation parameters in the same center.
Various attempts have been made to find a prenatal predictor for fetuses with gastroschisis to improve their outcome. The fetuses are particularly at risk to suffer an intrauterine death and therefore prenatal diagnosis of gastroschisis is important. Over the time amniotic fluid has a toxic effect on the bowel [9]. Antenatal ultrasound is used to predict the bowel condition and adverse outcome. Sonographic markers and timing of delivery are still discussed controversially.
Heinig et al. [8] described that a dilatation of the small bowel with more than 25 mm or a wall thickness of the small bowel more than 2.5 mm can be predictors of prenatal complications and outcome. In the current study these certain limits were used for fetal surveillance and counseling. Fetuses with more than 25 mm dilatation of the small bowel or 2.5 mm wall thickness were delivered by cesarean section.
Several other studies found a positive correlation between dilatation of the bowel and neonatal mortality and morbidity [10–12]. Lato et al. [13] described that a fetal bowel dilatation of more than 10 mm before 31th week of gestation had the highest predictive value for postnatal bowel complications. They observed that a bowel dilatation of more than 10 mm was associated with a longer hospital stay due to ileus, stenosis or wound infection. Kuvela et al. [14] suggested that intra-abdominal bowel dilatation is an ultrasound marker to predict gastroschisis with severe perinatal complications. Several other studies found no association between bowel dilatation and adverse outcome [5, 6, 15–17]. The results of Davis et al. [5] indicated that the thickness of the bowel does not predict the bowel condition at birth or the fetal outcome. In their study low birth weight, prematurity and small defect size were associated with worse outcomes and a survival rate of 89 %. In contrast, all of our patients survived using our modified prenatal management strategy. In the study of Durfee et al. [15] the prenatal bowel dilatation could not predict fetal outcome. Furthermore, Japaraj et al. [6] described that a dilatation of the small bowel with more than 17 mm was not associated with an adverse neonatal outcome. Overcash et al. [17] stated that prenatal predictors like IUGR, oligohydramions or bowel dilatation could not predict adverse neonatal outcome. In contrast, Heinig et al. [8] reported that a dilatation of more than 25 mm allows to identify fetuses with an increased risk of fetal distress. High sensitivity and specificity in predicting adverse obstetric complications were observed in their study.
In our study, after modification our prenatal management strategies, none of the fetuses had any prenatal complications. Because of weekly ultrasound examinations, starting at the 30th week of gestation, it was possible to detect suspect dilatation of the small bowel early enough to avoid prenatal complications. Although six fetuses of group 2 had a bowel dilatation of more than 25 mm, severe complications could be avoided by immediate and early enough delivery.
Not only the abdominal wall defect but also associated bowel complications are responsible for severe postnatal problems. Some of these complications are for example intestinal atresia, volvulus, perforation or necrotic segments. This influences the outcome of the neonates, too. In group 2 of our study only one of 25 newborns with gastroschisis had bowel complications after delivery. This low number of complications might be a result of our current management strategy, because the fetuses with a suspect bowel dilatation were promptly delivered by cesarean section. Noticeably is that other studies reported a wide range of complication rates (14–58 %) which might be a result of different management strategies. This includes the prenatal observation with or without sonographic monitoring or with the use of different fixed time points for delivery [5, 6, 15, 17–19]. Mesas Burgos et al. described in their study a better outcome of fetuses with gastroschisis if they were born at 35 completed gestational weeks by caesarian section. Fetuses born after 37 weeks had a higher rate of complications [20].
In our study, the birth weights of the newborns were noticeably different between the two groups. This is due to earlier delivery in group 2. However, although the fetuses were born earlier, the rates of prenatal complications and adverse bowel conditions were lower.
In accordance with our guidelines all fetuses were born by cesarean section. Some studies reported that the mode of delivery is not associated with the outcome of the newborn with gastroschisis. Davis et al. [5] said that the mode of delivery did not affect the outcome. In this study low birth weight, prematurity and small defect size were associated with worse outcome. Overcash et al. [17] found out that there was no noticeable difference in outcomes between vaginal and cesarean section.
The results of the current study indicate that small bowel dilatation can be a prenatal marker of postnatal outcome. The challenge of gastroschisis is to avoid prenatal complications such as fetal distress, intrauterine fetal death and unnecessary preterm delivery. With high resolution ultrasound devices and observation by a specialist it is possible to detect fetuses with gastroschisis early in pregnancy. The main result of our study is that after modification our prenatal management strategies no fetus died. Thus, our study provides evidence to suggest that small bowel dilatation of more than 25 mm or wall thickness more than 2.5 mm are predictors for severe complications.
There are some limitations to our study. First, we observed single center results with a average number of cases. Therefore, prospective multicenter studies with larger number of cases are needed to confirm our results. Second, this is a retrospective cohort study with the inherent possibility of selection bias and unknown confounders.
Nevertheless, the current study is the first which evaluates the outcome of fetuses with gastroschisis after modification of prenatal management strategies in a single perinatal center. We found indications that adverse perinatal events can be avoided by using the small bowel diameter and the wall thickness as markers for optimal timing of delivery.
Conclusion
We recommend a prenatal monitoring of the small bowel diameter and the wall thickness for fetuses with gastroschisis for timing of delivery.
References
Brown N, Nardi M, Greer RM, Petersen S, Thomas J, Gardener G et al (2014) Prenatal extra-abdominal bowel dilatation is a risk factor for intrapartum fetal compromise for fetuses with gastroschisis. Prenat Diagn. doi:10.1002/pd.4535 (Epub ahead of print)
Loane M, Dolk H, Bradbury I, EUROCAT Working Group (2007) Increasing prevalence of gastroschisis in Europe 1980–2002: a phenomenon restricted to younger mothers? Paediatr Perinat Epidemiol 21:363–369
Rasmussen SA, Frias JL (2008) Non-genetic risk factors for gastroschisis. Am J Med Genet C Semin Med Genet 15:199–212
Torfs CP, Velie EM, Oechsli FW, Bateson TF, Curry CJR (1994) A population based study of gastroschisis: demographic, pregnancy, and lifestyle risk factors. Teratology 50:44–53
Davis RP, Treadwell MC, Drongowski RA, Teitelbaum DH, Mychaliska GB (2009) Risk stratification in gastroschisis: can prenatal evaluation or early postnatal factors predict outcome? Pediatr Surg Int 25:319–325
Japaraj RP, Hockey R, Chan FY (2003) Gastroschisis: can prenatal sonography predict neonatal outcome? Ultrasound Obest Gynecol 21:329–333
Crawford RAF, Ryan G, Wright VM, Rodeck CH (1992) The importance of serial biophysical assessment of fetal wellbeing in gastroschisis. BJOG 99:899–902
Heinig J, Müller V, Schmitz R, Lohse K, Klockenbusch W, Steinhard J (2008) Sonographic assessment of the extra-abdominal fetal small bowel in gastroschisis: a retrospective longitudinal study in relation to prenatal complications. Prenat Diagn 28:109–114
Langer JC, Bell JG, Castillo RO, Crombleholme TM, Longaker MT, Duncan BW et al (1990) Etiology of intestinal damage in gastroschisis 2. Timing and reversibility of histological change, mucosal function, and contractility. J Pediatr Surg 25:1122–1126
Langer J, Khanna J, Caco C, Dykes EH, Nicolaides KH (1993) Prenatal diagnosis of gastroschisis: development of objective sonographic criteria for predicting outcome. Obstet Gynecol 81:53–54
Adra A, Landy H, Nahmias J, Gomez-Marin O (1996) The fetus with gastroschisis: impact of route of delivery and prenatal ultrasonography. Am J Obstet 174:540–546
Piper H, Jaksic (2006) The impact of prenatal bowel dilation on clinical outcomes in neonates with gastroschisis. J Pediatr Surg 41:897–900
Lato K, Poellmann M, Knippel AJ, Bizjak G, Stressig R, Hammer R et al (2013) Fetal gastroschisis: a comparison of second vs third-trimester bowel dilatation for predicting bowel atresia and neonatal outcomes. Ultraschall in Med 34(2):157–161
Kuleva M, Khen-Dunlop N, Dumez Y, Ville Y, Salomon LJ (2012) Is complex gastroschisis predictable by prenatal ultrasound?. BJOG 119:102–109
Durfee SM, Benson CB, Adams SR, Ecker J, House M, Jennings R et al (2013) Postnatal outcome of fetuses with the prenatal diagnosis of gastroschisis. J Ultrasound Med 32:407–412
Overton TG, Pierce MR, Gao H, Kurinczuk JJ, Spark P, Draper ES et al (2012) Antenatal management and outcome of gastroschisis in the UK. Prenat Diagn 32:1256–1262
Overcash RT, DeUgarte DA, Stephenson ML, Gutkin RM, Norton ME, Parmar S et al (2014) Factors associated with gastroschisis outcomes. Obstet Gynecol 124(3):551–557
Lepigeon K, Van Mieghem T, Vasseur Maurer S, Giannoni E, Baud D (2014) Gastroschisis—what should be told to parents? Prenat Diagn 34(4):316–326
Barseghyan K, Aghajanian P, Miller AD (2012) The prevalence of preterm births in pregnancies complicated with fetal gastroschisis. Arch Gynecol Obstet 286:889–892
Mesas Burgos C, Svenningsson A, Hammarqvist Vejde J, Granholm T, Connor P (2015) Outcomes in infants with prenatally diagnosed gastroschisis and planned preterm delivery. Pediatr Surg Int 31:1047–1053
R Core Team (2014) A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. www.R-project.org
Acknowledgments
None.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Bauseler, A., Funke, K., Möllers, M. et al. Outcome of fetuses with gastroschisis after modification of prenatal management strategies. Arch Gynecol Obstet 294, 239–243 (2016). https://doi.org/10.1007/s00404-015-3961-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-015-3961-1