Abstract
Purpose
To evaluate blood flow Doppler velocimetry during the first and second stages of active labor.
Methods
A prospective observational study was performed. Patients at term (37–42 weeks gestation), with normal fetal heart rate tracing patterns (categorized as category I) were examined during the first and second stages of labor. The sonographic parameters that were measured included the blood flow resistance of the maternal uterine artery (UtA) and umbilical artery (UA). Wilcoxon-matched pair test was used for the comparison of flows between the first and the second stages of labor.
Results
UtA and UA Doppler velocimetry measurements were obtained from 31 parturients. The left (LT) and right (RT) UtA pulsatility index (PI) was lower in the second stage of labor as compared with the first stage. However, only the LT side reached a statistically significant difference (0.88 ± 0.32 and 0.73 ± 0.18; P = 0.005). Compared with the first stage of labor, UA PI was significantly higher during the second stage of labor (0.72 ± 0.17 vs. 0.84 ± 0.33; respectively, P = 0.05).
Conclusion
Significant blood flow resistance changes in maternal as well as in fetal blood vessels occur during the second stage as compared with the first stage of active labor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The challenge of modern obstetrics is to provide a safe delivery. Since the invention of fetal tocometry, different techniques have been attempted to prevent fetal compromise. Non-invasive modalities for fetal evaluation include fetal oxygen saturation and blood flow measurements in maternal and fetal vessels.
During pregnancy, increased uteroplacental blood flow is related to trophoblast invasion of spiral arteries [1, 2]. There are only few studies regarding the utility of Doppler examination during labor. In one study, a mean reduction of uterine artery blood flow velocity of 40–60 % was reported, for a maximal intrauterine pressure of approximately 60 mmHg [3]. Diastolic flow decreased to zero, when intrauterine pressure was 80 mmHg, but the systolic blood flow was evident up to an intrauterine pressure of 130 mmHg [4].
UA blood flow velocity was evaluated as a screening test for intrapartum fetal distress on admission to the delivery room [5]. A 12-fold increase in the rate of emergency cesarean sections for fetal distress among women with a systolic/diastolic (S/D) ratio ≥3.0 was noted [5]. The authors concluded that umbilical artery blood velocity waveform analysis may be used to screen for fetal distress. On the contrary, in a later review, umbilical artery Doppler velocimetry was described as a poor predictor for adverse perinatal outcomes [6].
Very few studies have evaluated the changes in fetal cerebral vascularization during labor. Middle cerebral artery (MCA) Doppler velocimetry showed a significantly lower pulsatility index (PI) in the presence of reduced oxygen saturation during the first stage of labor [7]. A previous study investigated MCA Doppler velocimetry measurements taken less than 24 h before a planned cesarean section (CS) for various indications. In this study, redistribution of fetal circulation was neither related to umbilical cord blood gases nor to Apgar scores [8]. In another study by Siristatidis et al. [9] MCA Doppler velocimetry showed significantly lower PI with hypoxia.
To the best of our knowledge, no previous studies have compared blood flows between the first and second stages of labor. The objectives of the present study were to evaluate blood flow velocimetry in the uterine artery (UtA), the umbilical artery (UA) and the MCA during both the first and second stages of active labor.
Materials and methods
A prospective observational study was designed to evaluate blood flow velocimetry during active labor. Parturients in active labor at term (37–42 weeks gestation) with a singleton pregnancy in the vertex presentation were included in the study.
Fetal heart rate tracing pattern categories were defined, according to the American College of Obstetricians and Gynecologists (ACOG) criteria [10]. Only patients with fetal heart rate tracing patterns categorized as category I according to the ACOG [10] were included in the study. Patients with multiple gestations, intrauterine growth restriction, hypertensive disorders, fetal malformations, and malpresentations were excluded from the study.
The local ethics institutional review board approved the study; all patients received a detailed explanation concerning the research and all have signed an informed consent form.
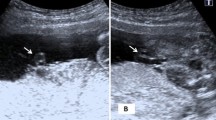
All patients were examined during the first and second stages of labor (at 4–5 cm dilatation and again at 10 cm dilatation). Ultrasound examinations were performed using a transabdominal approach. Each patient has been examined both in the first and the second stages of labor by one of the examiners (JB or PS). Doppler ultrasonographic studies were carried out with Aloka 3500 SSD ultrasound machine. UA Doppler waveforms were obtained from a free umbilical cord loop. UA and MCA flow velocimetry were obtained when fetal movements were absent. Measurements were not obtained during contractions. All measurements were performed using an insonation angle of less than 60°. Measurements were taken only when at least a minimum of three repetitive waveforms were documented. The sonographic parameters that were measured included the blood flow PI of the maternal UtA, fetal MCA and UA. If the patient elected to have an epidural, the sonographic measurements were taken only after the epidural was performed. Maternal age, birth weight, gestational age, parity and gravidity were recorded.
Statistical analysis was performed using GraphPad Prism 5.0 software (GraphPad Prism, Pugh computers, Aberystwyth, UK). Wilcoxon-matched pair test for the comparison of the two matched groups was used. A P value of ≤0.05 was considered statistically significant.
Results
Uterine artery and UA Doppler velocimetry measurements were obtained from 31 patients. However, measurements of the MCA blood flow during the second stage of labor was possible in only three patients due to low position of the fetal head, patient movements during labor and technical sonographic difficulties. Even a trial of transvaginal approach failed to receive a satisfactory sonographic measurement due to fetal head position that impaired an appropriate axial view. The clinical maternal and fetal characteristics are presented in Table 1.
Blood flow Doppler velocimetry PI in maternal and fetal vessels are presented in Table 2. A statistically significant difference was found in the LT UtA PI between the first and second stages of labor (0.88 ± 0.32 and 0.73 ± 0.18; P = 0.005). The RT UtA PI was also lower during the second stage of labor as compared with the first stage. However, this change was not statistically significant (0.88 ± 0.25 and 0.81 ± 0.16; P = 0.19). Compared with the first stage of labor, UA PI was significantly higher during the second stage of labor (0.72 ± 0.17 vs. 0.84 ± 0.33; respectively, P = 0.05).
No adverse neonatal outcomes were noted. All neonatal 5-min Apgar scores were 10 and only one post labor fetal pH was lower than 7.2 (pH = 7.17). Seventy one percent have received epidural anesthesia.
Discussion
In this study, we have focused on the UA and UtA to better understand the blood flow patterns during normal labor. A previous study has demonstrated that during active labor, the UtA flow changes with uterine contractions during active labor [3]. Accordingly, in the present study, we attempted to avoid the effect of uterine contractions on blood flow measurements. Therefore, we performed all study measurements during the intervals between contractions. This interval was confirmed by the patient’s clinical state and was proved by fetal tocometry.
During the second stage of labor, UA Doppler velocimetry PI was significantly higher during the second as compared with the first stage of labor. This change is in accordance with a previous report that found that in the presence of reduced oxygen saturation during the first stage of labor, UA PI showed mildly higher resistance indices (0.98 ± 0.14 vs. 1.28 ± 0.50, p = 0.01) [9]. A possible explanation is a reduced fetal perfusion in the second stage of labor due to maternal intense pushing, or due to a higher frequency of uterine contractions, that can reduce fetal oxygenation that may in turn cause increased blood flow resistance.
Interestingly, the mean UA Doppler velocity PI index during the first stage of labor in our study was lower than previously found by Siristatidis et al. (0.72 vs. 0.98) [9]. This could be attributed to the fact that measurements of the UA Doppler were performed in different parts of the umbilical cord. In the present study, the UA Doppler velocimetry was only measured in a free loop, while in the study of Siristatidis et al. [9]. The umbilical artery PI was measured in the fetal end of the cord.
Blood flow differences were noted between the left and right uterine arteries. A reduction in the resistance between the first and second stages of labor was noted in the right and the left UtA. However, only in the left uterine artery, the PI was significantly lower during the second stage of labor as compared to the first stage. This reduction in the PI between the two stages of labor could be explained by an effort to compensate fetal reduced oxygenation by supplying higher perfusion to the placenta.
The uniqueness of this study is the measurements of UtA and UA throughout labor. To the best of our knowledge, this is the first study that followed UtA and UA PI also during the second stage of labor. This study provides clinically important data regarding normal blood flows during normal deliveries. However, this study is not without limitations. One weakness is that the relatively small number of participants prevented us from performing powerful subgroup analysis.
In our study, 29 % of the patients delivered without epidural analgesia. A recent study had demonstrated an elevated UtA PI after epidural anesthesia during the first stage of labor, but no change in the UA PI was noted [11]. The authors did not differentiate the measurements between the RT and LT UtA. In another study that did differ between RT and LT UtAs before and after epidural anesthesia, there was a significant reduction in UtA Doppler velocities but the RI was not significantly different [12]. In our study, 71 % of patients had epidural anesthesia. In these patients, measurements were taken shortly after the epidural analgesia was performed. The differences between the first and second stages of labor in patients under epidural anesthesia were still significant in the LT UtA but not on the RT side.
Placentation causes remodeling of maternal spiral arteries; this may alter uterine blood flows [13]. Knowledge of the sites of origin could explain, at least in part, differences between the flow patterns in the LT and RT UtAs. The placental location (LT vs. RT) is normally noticed in the second trimester. In the third trimester, the placenta grows and it becomes more difficult to notice the placental site of origin. Because our study was performed during the late third trimester, we could not differentiate between the placental sites of origin. Moreover, it is unlikely that the side of placentation has influenced the changes that were found, since the compared measurements were carried out from the same side during both the first and the second stages of delivery.
In conclusion, in the second stage of labor there are significant blood flow resistance changes in maternal as well as in fetal blood vessels compared to the first stage of labor.
References
Groom KM, North RA, Stone PR et al (2009) Patterns of change in uterine artery Doppler studies between 20 and 24 weeks of gestation and pregnancy outcomes. Obstet Gynecol 113:332–338
Burton GJ, Woods AW, Jauniaux E, Kingdom JC (2009) Rheological and physiological consequences of conversion of the maternal spiral arteries for uteroplacental blood flow during human pregnancy. Placenta 30:473–482
Li H, Gudmundsson S, Olofsson P (2004) Clinical significance of uterine artery blood flow velocity waveforms during provoked uterine contractions in high-risk pregnancy. Ultrasound Obstet Gynecol 24:429–434
Kurjak A, Dudenhausen JW, Kos M et al (1996) Doppler information pertaining to the intrapartum period. J Perinat Med 24:271–276
Somerset DA, Murrills AJ, Wheeler T (1993) Screening for fetal distress in labour using the umbilical artery blood velocity waveform. Br J Obstet Gynaecol 100:55–59
Farrell T, Chien PF, Gordon A (1999) Intrapartum umbilical artery Doppler velocimetry as a predictor of adverse perinatal outcome: a systematic review. Br J Obstet Gynaecol 106:783–792
Kassanos D, Siristatidis C, Vitoratos N, Salamalekis E, Creatsas G (2003) The clinical significance of Doppler findings in fetal middle cerebral artery during labor. Eur J Obstet Gynecol Reprod Biol 109:45–50
Cheema R, Dubiel M, Gudmundsson S (2009) Signs of fetal brain sparing are not related to umbilical cord blood gases at birth. Early Hum Dev 85:467–470
Siristatidis C, Salamalekis E, Kassanos D, Loghis C, Creatsas G (2004) Evaluation of fetal intrapartum hypoxia by middle cerebral and umbilical artery Doppler velocimetry with simultaneous cardiotocography and pulse oximetry. Arch Gynecol Obstet 270:265–270
American College of Obstetricians and Gynecologists (2009) ACOG practice bulletin No. 106: intrapartum fetal heart rate monitoring: nomenclature, interpretation, and general management principles. Obstet Gynecol 114:192–202
Selim MF, Elnabtity AM, Hasan AM (2012) Comparative evaluation of epidural bupivacaine—dexmedetomidine and bupivacaine-fentanyl on Doppler velocimetry of uterine and umbilical arteries during labor. J Prenat Med 6:47–54
Valentin M, Ducarme G, Ceccaldi PF, Bougeois B, Luton D (2012) Uterine artery, umbilical, and fetal cerebral Doppler velocities after epidural analgesia during labor. Int J Gynaecol Obstet 118:145–148
Redman CW, Sargent IL (2005) Latest advances in understanding preeclampsia. Science 308:1592–1594
Conflict of interest
The authors report no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baron, J., Shwarzman, P., Sheiner, E. et al. Blood flow Doppler velocimetry measured during active labor. Arch Gynecol Obstet 291, 837–840 (2015). https://doi.org/10.1007/s00404-014-3489-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-014-3489-9