Abstract
Doppler is the mainstay of the diagnosis and management of high-risk pregnancies, as fetal arterial and venous Doppler parameters indicate the likelihood of the fetus being healthy, hypoxic, or acidaemic. Despite studies showing the relationship between Doppler parameters and fetal outcome, there are little data from randomized or high-grade evidence to inform how Doppler findings should inform practice. Meta-analysis shows that performing umbilical artery Doppler in high-risk pregnancies reduces perinatal morbidity and mortality, though it remains unclear as to why. In early fetal growth restriction, the only appropriately powered randomized study has shown a benefit in survivor neurodevelopmental outcome in those delivered on the basis of late changes of the ductus venosus and/or cardiotocography. Randomized studies to delineate the value of middle cerebral artery Doppler in guiding delivery timing are underway and are yet to be reported.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Umbilical
- Middle cerebral artery
- Ductus venosus
- Cardiotocography
- A-wave
- PI
- Perinatal
- Mortality
- Morbidity
- Cochrane
- TRUFFLE
- CTG
26.1 Introduction
Doppler technology has spread progressively with advances in ultrasound machines’ performance, operators’ training, and better understanding of the physiopathology of the feto-placental circulation in pathologies such as fetal growth restriction, hypertensive disorders in pregnancy, and twin pregnancies among others. For example, the cascade of Doppler changes in early fetal growth restriction, caused by uteroplacental insufficiency, and its association with an adverse perinatal outcome is now well-known [1,2,3]. The identification of hypoxia and acidemia constitutes the rationale for using Doppler ultrasound as one of the main tools for fetal well-being assessment and management in fetal growth restriction [4, 5]. Similarly, the management of monochorionic twin pregnancy [6] or fetal anemia [7] is unthinkable without Doppler ultrasound assessment of specific vascular domains. Although not universally adopted, Doppler of the uterine arteries, first applied in the mid-trimester [8, 9], represents one of the main components of first-trimester screening of preterm pre-eclampsia and fetal growth restriction [10, 11]. Hence, the application of Doppler ultrasound in high-risk pregnancies has become a standard clinical practice worldwide.
On the other hand, multiple Doppler interrogations of vascular districts may also cause false-positive findings, consequent unnecessary interventions, and potential adverse outcomes such as prematurity and patient and physician anxiety. Last but not least, for some widespread Doppler ultrasound applications, such as the assessment of the middle cerebral artery in fetal growth restriction, there is no high-quality evidence for its value, leading to variable clinical practice and management.
In this chapter, we will summarize the evidence from randomized clinical trials on Doppler velocimetry in high-risk pregnancies with a particular focus on fetal growth restriction and the effect of its application on maternal and fetal outcomes.
26.2 Trials of Umbilical Artery Doppler in High-Risk Pregnancies
26.2.1 Evidence from Randomized Studies
The Cochrane Systematic Review and meta-analysis on randomized and quasi-randomized controlled trials on fetal and umbilical Doppler ultrasound in high-risk pregnancies [12] reported 18 studies that compared the use of umbilical artery Doppler with no-Doppler (or Doppler not revealed to clinicians). In 14 studies, umbilical artery Doppler was used in addition to the standard fetal monitoring strategy [13,14,15,16,17,18,19,20,21,22,23,24,25,26], whereas in 4 studies, umbilical artery Doppler was evaluated compared to cardiotocography [27,28,29,30]. Table 26.1 shows the characteristics of the included studies in this meta-analysis. It should be noted that two of the included studies evaluated the Doppler of the umbilical and uteroplacental arteries [19, 26]: one evaluated the Doppler of the umbilical artery and aorta [21] and the other evaluated the middle cerebral to umbilical artery velocity flow systolic/diastolic ratio [23].
The pooled data of the use of umbilical artery Doppler ultrasound in high-risk pregnancies showed fewer perinatal deaths (risk ratio (RR) 0.71, 95% confidence interval (CI) 0.52–0.98, 16 studies, 10,225 babies, 1.2% versus 1.7% number needed to treat (NNT) 203, 95% CI 103–4352, evidence graded as moderate) [12]. The findings for stillbirths and neonatal deaths were similar, showing fewer adverse outcomes in the Doppler group, although these did not reach statistical significance (stillbirth: RR 0.65, 95% CI 0.41–1.04, 15 studies, 9560 babies, evidence graded as low; neonatal deaths: RR 0.81, 95% CI 0.53–1.24, 8167 babies, 13 studies) [12]. Only three studies reported relevant neonatal morbidity data [19, 22, 26]. However, the heterogeneity was high and the quality of evidence extremely low, making the analysis uncertain [12].
Moreover, the use of umbilical artery Doppler was associated with fewer inductions of labor and fewer cesarean sections (induction of labor: RR 0.89, 95% CI 0.80–0.99, 10 studies, 5633 women, evidence graded as moderate; cesarean section: RR 0.90, 95% CI 0.84–0.97, 14 studies, 7918 women, evidence graded as moderate) [12]. Data for serious neonatal morbidity could not be pooled due to high heterogeneity between the studies. Finally, although not a pre-specified outcome, there were fewer antenatal admissions in the Doppler group (RR 0.72, 95% CI 0.60–0.88, 839 women, 2 studies) [12].
Four trials [27,28,29,30] compared the umbilical artery Doppler assessment with cardiotocography assessment. However, for this comparison, there was insufficient evidence to detect a significant difference in perinatal mortality.
In summary, as presented in Table 26.2, these data suggest that the use of umbilical artery Doppler ultrasound, with or without cardiotocography, in high-risk pregnancies reduces the risk of perinatal deaths and reduces obstetric interventions compared to no-Doppler [12].
However, it has to be acknowledged that this meta-analysis included all pregnancies defined to be at a higher risk of fetal compromise, such as fetal growth restriction, post-term pregnancies, multiple pregnancies, previous pregnancy loss, women with hypertension, women with diabetes or other maternal pathologies. When a subgroup analysis was performed (i.e., only singleton or multiple or only small for gestational age or fetal growth restriction), there was no evidence of the treatment effect. There are five randomized controlled trials that assessed Doppler in the umbilical artery versus no-Doppler ultrasound in women with suspected small-for-gestational-age/growth-restricted fetuses [18, 20, 24, 27, 28]; only one study assessed the role of Doppler ultrasound in the umbilical artery versus no-Doppler ultrasound in pregnancies complicated by hypertension or pre-eclampsia [24] and only one study assessed the role of Doppler ultrasound in the umbilical artery versus no-Doppler ultrasound in women with previous pregnancy loss [22]. There were no significant differences in terms of perinatal mortality in the treatment group versus that in the no-treatment group (small-for-gestational-age/fetal growth restriction group: RR 0.72, 95% CI 0.38–1.35, 1292 women, 5 studies; hypertensive disorders in pregnancy group: RR 3.57, 95% CI 0.42–30.73, 89 women, 1 study; previous pregnancy loss group: RR 0.26, 95% CI 0.03–2.17, 53 women, 1 study).
The lack of evidence in subgroup analysis might be due to several factors such as a small number of included cases, publication bias, and heterogeneity of the included studies. It is noteworthy that all studies were published more than 20 years ago, the reason being the fact that at present not performing umbilical artery Doppler in high-risk pregnancies would now be considered as unethical. Finally, the fact that the majority of the studies were performed in the 1990s, before the international agreement on how to report clinical trials [31], makes quality assessment of the older studies imprecise, and very few studies are graded as high-quality by today’s standards.
The next question might be whether there is a specific group of high-risk pregnancies that benefits most from umbilical artery Doppler assessment. In order to answer this question, Westergaard et al. [32] performed a meta-analysis dividing the studies into “well-defined studies,” i.e., studies that included pregnancies complicated by fetal growth restriction and/or hypertensive disorders in pregnancy, and “general risk studies,” i.e., studies that included a variety of high-risk pregnancies. There were no statistically significant differences for perinatal mortality in both groups (well-defined studies: odds ratio (OR) 0.66, 95% CI 0.36–1.22; general risk studies: OR 0.68, 95% CI 0.43–1.08). However, an international experts’ audit on perinatal deaths concluded that the use of Doppler in “well-defined studies” potentially might have prevented some. In the same group, there was a significant reduction in antenatal admissions, induction of labor, elective deliveries (induction and cesarean sections), and overall cesarean sections (OR 0.56, 95% CI 0.43–0.72; OR 0.78, 95% CI 0.63–0.96; OR 0.73, 95% CI 0.61–0.88 and OR 0.78, 95% CI 0.65–0.94, respectively). In conclusion, this meta-analysis suggests that pregnancies complicated by fetal growth restriction and/or hypertensive disorders in pregnancy would benefit most from umbilical artery Doppler assessment [32].
There are no randomized controlled trials on the umbilical artery in high-risk pregnancies, which evaluated long-term infant outcomes.
26.2.2 Implication for Practice
The findings from the first systematic review and meta-analysis of randomized controlled trials on fetal and umbilical artery Doppler in high-risk pregnancies [33, 34], and subsequent updates [12, 35, 36], showed an improvement in perinatal outcomes and a reduction in operative deliveries. This led to the introduction of umbilical artery Doppler assessment in the management of high-risk pregnancies like fetal growth restriction [37]. The data from the meta-analysis of randomized trials suggest that the availability of umbilical artery Doppler in high-risk pregnancies allows for better timing of delivery to reduce the perinatal mortality and emergency cesarean sections, indicating a better identification of compromised babies before or during labor. This seems particularly true for cases with underlying placental insufficiency, such as fetal growth restriction and hypertensive disorders in pregnancy [32].
As a diagnostic test, umbilical artery Doppler is of importance for the diagnosis of fetal growth restriction and the distinction from small-for-gestational-age fetuses [38, 39], especially at the earlier gestational age epochs. However, it is still not completely clear which intervention, and when, should follow an abnormal umbilical artery Doppler finding in fetal growth restriction, with this being a crucial point in influencing the outcome. In fact, there are no randomized controlled clinical trials on delivery timing in fetal growth restriction based on umbilical artery Doppler. The same applies to the findings of absent or reverse end-diastolic flow in the umbilical artery. The latter findings reflect a more severe placental compromise [40] and are associated with higher perinatal morbidity and mortality [41]. However, there are no randomized controlled trials to support the optimum management protocol in these cases.
26.3 Trials of Ductus Venosus Doppler in High-Risk Pregnancies
26.3.1 Evidence from Randomized Studies
Abnormalities of the ductus venosus waveform are reported to be a good predictor of a perinatal outcome in early fetal growth restriction [1, 2, 42]. The alterations in ductus venosus flow, especially absent or reversed A-wave, represent late changes in the biophysical cascade of events in early fetal growth restriction, together with alterations of short-term variation and biophysical profile, preceding fetal acidemia, and intrauterine fetal demise [1,2,3]. It is believed that these changes in the ductal waveform are caused by progressive dilatation of the isthmus in an attempt to increase the blood flow toward the heart and to compensate for hypoxia [43, 44]. Thus, from the beginning, it has been clear that the assessment of the ductus venosus in early fetal growth restriction plays a crucial role. However, balancing delivery timing with prematurity is also of critical importance for perinatal and long-term outcomes [45,46,47]. This raises the question regarding the best biophysical tool and delivery timing in these fetuses.
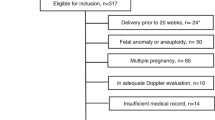
The only randomized controlled trial that compared different biophysical tools in delivery decision-making in early fetal growth restriction is the TRUFFLE (TRial of Umbilical Fetal FLow in Europe) study [48, 49]. This trial involved 20 European centers and compared 3 interventional arms, early and late ductus venosus changes and short-term variation at computerized cardiotocography, as a trigger for delivery in singleton pregnancies with fetal growth restriction between 26 and 32 weeks of gestation in 503 women [49]. Fetal growth restriction was defined as an abdominal circumference below the tenth centile and an umbilical artery pulsatility index above the 95th centile. The three randomization interventional arms were as follows:
-
1.
Early changes in the ductus venosus, defined as a pulsatility index above the 95th centile
-
2.
Late changes in the ductus venosus, defined as absent or reverse A-wave
-
3.
Reduced short-term variation, below 3.5 ms between 26+0 and 28+6 weeks of gestation and below 4 ms between 29+0 and 31+6 gestational weeks
There was a cardiotocography “safety net” for all three arms representing an absolute indication for delivery represented by:
-
Spontaneous, repeated, persistent unprovoked decelerations in all three arms
-
Short-term variation below 2.6 ms at 26+0–28+6 weeks and below 3 ms at 29+0–31+6 weeks in ductus venosus arms
The short-term variation “safety net” was deliberately set at a level below that of the cardiotocography arm (arm 3); hence, changes needed to be more extreme in the two ductus venosus groups. In addition, maternal conditions represented an indication for delivery in any group and at any gestational week. Figure 26.1 is the schematic representation of TRUFFLE randomization interventional arms and safety net.
The primary outcome of the TRUFFLE study was a 2-year survival without neurological impairment. The proportion among survivors without neurodevelopmental impairment at 2 years was 85% in the short-term variation group and 91% and 95% in early and late ductus venosus groups, respectively. A significant proportion of babies delivered in the late changes ductus venosus group was due to the short-term variation safety net criteria. Moreover, in the same group, there was a statistically non-significant increase in perinatal and infant mortality rate.
Overall, the results from the TRUFFLE study provided evidence that the timing of delivery based on ductus venosus Doppler measurement in conjunction with short-term variation “safety net” improves long-term (2-year neurodevelopmental) infant outcome in survivors [49]. Despite the fact that data from the TRUFFLE study showed better than assumed results in terms of survival without neurological impairment (overall, 82% of children), the gestational age at study entry and delivery and birth weight were strongly related to an adverse outcome as shown in Fig. 26.2.
Proportion of neonates without severe morbidity (white bars), with severe morbidity (light gray bars), neonatal death (dark gray bars), and fetal death (black bars) according to a) gestational age at inclusion and b) gestational age at delivery. Severe morbidity was defined as bronchopulmonary dysplasia, severe germinal matrix cerebral hemorrhage grade III or IV, cystic periventricular leukomalacia of more than grade I, proven neonatal sepsis or necrotizing enterocolitis (from Lees et al. [49] and Bilardo et al. [50])
26.3.2 Implication for Practice
Besides providing evidence for the best delivery trigger and timing in early fetal growth restriction between 26 and 32 weeks of gestation, as shown in the flowchart of the recommended protocol (Fig. 26.3) [50], the TRUFFLE study provided other important information with implications for practice. The study clearly demonstrated that when a specific protocol is uniformly applied and pregnancies are managed by expert multidisciplinary obstetric and neonatal teams, then the outcomes are better than might be expected from contemporary data. Nearly three-quarters of women developed hypertensive disorders in pregnancy, implying the need for strict blood pressure monitoring in these women. The onset of maternal hypertension had an impact on the interval from inclusion to delivery, much shorter in women who had pre-eclampsia at inclusion (median 4 days, interquartile range (IQR) 2–10) than in those that did not (median 12 days, IQR 5–20) [48]. Finally, data presented in Fig. 26.2 might be helpful in counseling parents regarding morbidity, mortality, and adverse long-term outcomes at diagnosis and at delivery according to gestational age.
Flowchart of the TRUFFLE protocol (from Bilardo et al. [50])
It is important to highlight that outcomes similar to that of the TRUFFLE trial can be replicated only in fetal growth restriction from 26 to 32 weeks, using the monitoring strategy and delivery decision-making based on ductus venosus Doppler in conjunction with the assessment of short-term variation obtained by computerized cardiotocography.
26.4 Trials of Middle Cerebral Artery Doppler or its Ratio to the Umbilical Artery in High-Risk Pregnancies
26.4.1 Evidence from Randomized Studies
The fetal response to hypoxemia is the redistribution of the blood flow to vital organs such as the brain, heart, and adrenal glands [5]. Thus, the so-called brain-sparing effect, or cerebral redistribution, represents a fetal adaptation to reduced oxygen availability. This observation might be relevant especially in late fetal growth restriction where alterations of the umbilical artery and ductus venosus districts are rare and fail to identify the majority of late fetal growth-restricted fetuses [51].
Several studies have found an association between cerebral redistribution with a poorer perinatal outcome, including stillbirth [52], a higher risk of cesarean delivery [53,54,55], and an increased risk of abnormal neurodevelopment at birth [56] and at 2 years of age [57]. These data are also supported by systematic reviews [58,59,60] and meta-analyses [61, 62].
To our knowledge, the only randomized study that evaluated the impact of cerebral redistribution on a perinatal outcome in patients at high risk was the study by Ott et al [23] In this study, the addition of the middle cerebral to umbilical artery systolic/diastolic velocity waveform ratio to the modified biophysical profile was evaluated. The study included a heterogeneous group of pregnancies considered to be at a higher risk (risk of uteroplacental insufficiency, post-dates, maternal diabetes, fluid abnormalities, and others). Overall, there were no statistically significant differences in the perinatal outcome. However, when only a subgroup of fetuses at a risk of uteroplacental insufficiency was considered, a significant difference in the cesarean section rate for fetal distress was observed, with fewer cesarean sections in the intervention group (1/63, 1.6%) than in the control group (6/56, 10.7%, p = 0.04) [23].
There are no randomized controlled trials on the application of middle cerebral artery Doppler and its impact on long-term outcomes in high-risk pregnancies, including fetal growth restriction. This makes the quality of the evidence, on which the application of middle cerebral artery Doppler is based, extremely low, mainly based on retrospective or prospective observational data or secondary analysis of primary studies. Thus, the application of middle cerebral artery Doppler and its ratio in high-risk pregnancies, particularly in fetal growth restriction, based on high-quality studies and strong evidence is still missing, leaving it as an unresolved question. The difficulty in interpreting these studies pertains to whether abnormal cerebral Doppler is in itself injurious to fetal outcome and neurodevelopment or whether it is simply a marker of hypoxia and it is hypoxia itself that is damaging or alternatively that these Doppler changes lead to iatrogenic delivery and prematurity.
26.4.2 Implication for Practice
There is no international consensus as to the timing of delivery in late fetal growth restriction (somewhat arbitrarily defined as after 32 weeks) due to the lack of interventional management randomized trials based on Doppler indices or other biophysical tools. In fact, the national guidelines for the management of late fetal growth restriction are highly variable [63], and, hence, management is mainly based on expert opinion [64, 65].
The secondary analysis of the TRUFFLE study showed a weak association between the low middle cerebral artery pulsatility index and adverse short-term neonatal outcome and between the low middle cerebral artery pulsatility index and high umbilical-cerebral (but not cerebral-placental) ratio with 2-year adverse neurodevelopmental outcome [66]. However, the gestational age at delivery and birth weight had the most pronounced impact on these outcomes (Fig. 26.4). These data suggest that middle cerebral artery Doppler might be used to guide monitoring before 32 weeks of gestation, but there is no evidence that it should be used to determine delivery timing [67].
Secondary analysis of the TRUFFLE study: odds ratios with 95% confidence intervals for neonatal and 2-year infant outcome (from Stampalija et al. [66]). The upper panel (a) represents the odds ratios for neonatal outcome (survival until the first discharge home without severe morbidity), and the lower panel (b) represents the odds ratios for the 2-year infant outcome (survival without neurological impairment at 2 years) of the z-scores of the middle cerebral artery (MCA) pulsatility index, umbilical-cerebral ratio (UCR), and cerebroplacental ratio (CPR) at inclusion (first) and within 1 week before delivery (last), adjusted for birth weight, p50 ratio, and gestational age. The odds ratios of the adjusting parameters are shown below the horizontal line. DV p95: early changes in the ductus venosus (DV-PI>95th percentile); DV no A: late changes in the ductus venosus (no or reverse A-wave flow)
A recent secondary analysis of the PORTO study (Perinatal Ireland Multicenter Observational Prospective Observational Trial to Optimize Pediatric Health in Fetal Growth Restriction) has shown that fetuses with growth restriction across all gestational age epochs and with an abnormal cerebro-placental ratio (<1) had a significantly poorer neurological outcome at 3 years [68]. The authors conclude that the study “further substantiates the benefit of routine assessment of cerebroplacental ratio in fetal growth restricted pregnancies and for counseling parents regarding the long-term outcome of affected infants.” When assessing an adverse short- or long-term outcome, both the severity of growth restriction and gestational age at delivery should be taken into account while representing an independent risk factor for the adverse outcome. It still remains to be elucidated whether cerebral redistribution is an independent risk factor for an adverse outcome or it “only” reflects the severity of growth restriction.
The TRUFFLE-2 feasibility study explored the association between cerebral redistribution and outcome in late preterm (32+0–36+6 weeks of gestation) pregnancies at a risk of fetal growth restriction [69]. In this large multi-center (33 European centers) prospective cohort study of 862 women, infants with composite adverse outcome were delivered at a lower gestational age (36 versus 38 weeks) with a lower birth weight (1900 g versus 2540 g). However, the first observation of cerebral redistribution after inclusion, defined as the middle cerebral artery pulsatility index below the fifth centile and specific umbilicoplacental ratio z-score thresholds (1.5 at 32–33 weeks and 1.0 at 34–36 weeks, respectively), had the highest relative risk of a composite adverse outcome (RR 2.1; 95% CI 1.5–3.2 and RR 2.1; 95% CI 1.4–3.1, respectively). This effect was independent of gestational age below 36 weeks of gestation, as shown in Tables 26.3 and 26.4. These data would support an association between cerebral redistribution and adverse outcome, but like other un-blinded observational studies, the weakness is that there might be a treatment paradox. Finally, the association does not imply causality. Thus, a randomized trial is required to answer the uncertainties regarding delivery timing in late fetal growth restriction in relation to cerebral blood flow redistribution.
26.5 Implications for Research
The type and frequency of monitoring after the identification of abnormal umbilical artery Doppler in fetal growth restriction is still not clear, or, at least, it has not been tested by randomized controlled trials. There is no doubt that umbilical artery assessment is of crucial importance to identify fetal growth restriction, especially early-onset, due to placental insufficiency. However, the best delivery timing and impact on short- and long-term outcomes, in the presence of absent or reverse end-diastolic flow or increased pulsatility index in the umbilical artery, from 32 weeks, has not been appropriately evaluated in randomized controlled trials.
Despite emerging awareness that there might be an association between cerebral blood flow redistribution and adverse perinatal outcome, in the absence of randomized controlled trials, it is still not clear whether the assessment and delivery decision based on Doppler evaluation of cerebral blood flow redistribution is beneficial in terms of short- and long-term neurodevelopmental outcomes and which is the optimal gestational age to deliver (beside the optimal Doppler parameter and threshold).
Key Messages
The available evidence from randomized controlled trials suggests:
-
Umbilical artery assessment improves perinatal outcome in high-risk pregnancies, particularly in pregnancies at risk of placental insufficiency.
-
In early fetal growth restriction (26–32 weeks), the best outcome at 2 years is obtained by timing the decision for delivery on combined monitoring by the ductus venosus and short-term variation obtained by computerized cardiotocography.
-
In late fetal growth restriction (after 32 weeks), there is little or no evidence to inform the frequency of Doppler evaluation and the timing of delivery based on umbilical artery and/or middle cerebral artery assessment.
References
Ferrazzi E, Bozzo M, Rigano S, Bellotti M, Morabito A, Pardi G, Battaglia FC, Galan HL. Temporal sequence of abnormal Doppler changes in the peripheral and central circulatory systems of the severely growth-restricted fetus. Ultrasound Obstet Gynecol. 2002;19:140–6.
Baschat AA, Gembruch U, Harman CR. The sequence of changes in Doppler and biophysical parameters as severe fetal growth restriction worsens. Ultrasound Obstet Gynecol. 2001;18:571–7.
Hecher K, Bilardo CM, Stigter RH, Ville Y, Hackeloer BJ, Kok HJ, Senat MV, Visser GH. Monitoring of fetuses with intrauterine growth restriction: a longitudinal study. Ultrasound Obstet Gynecol. 2001;18:564–70.
Hecher K, Snijders R, Campbell S, Nicolaides K. Fetal venous, intracardiac, and arterial blood flow measurements in intrauterine growth retardation: relationship with fetal blood gases. Am J Obstet Gynecol. 1995;173:10–5.
Richardson BS, Bocking AD. Metabolic and circulatory adaptations to chronic hypoxia in the fetus. Comp Biochem Physiol A Mol Integr Physiol. 1998;119:717–23.
Khalil A, Rodgers M, Baschat A, Bhide A, Gratacos E, Hecher K, Kilby MD, Lewi L, Nicolaides KH, Oepkes D, Raine-Fenning N, Reed K, Salomon LJ, Sotiriadis A, Thilaganathan B, Ville Y. ISUOG practice guidelines: role of ultrasound in twin pregnancy. Ultrasound Obstet Gynecol. 2016;47:247–63.
Mari G, Norton ME, Stone J, Berghella V, Sciscione A, Tate D, Schenone MH. Society for Maternal-Fetal Medicine (SMFM) clinical guideline #8: the fetus at risk for anemia: diagnosis and management. Am J Obstet Gynecol. 2015;212:697–710.
Albaiges G, Missfelder-Lobos H, Lees C, Parra M, Nicolaides KH. One-stage screening for pregnancy complications by color Doppler assessment of the uterine arteries at 23 weeks’ gestation. Obstet Gynecol. 2000;96:559–64.
Papageorghiou AT, Yu CK, Bindra R, Pandis G, Nicolaides KH, Fetal Medicine Foundation Second Trimester Screening Group. Multicenter screening for pre-eclampsia and fetal growth restriction by transvaginal uterine artery Doppler at 23 weeks of gestation. Ultrasound Obstet Gynecol. 2001;18:441–9.
Sotiriadis A, Hernandez-Andrade E, da Silva CF, Ghi T, Glanc P, Khalil A, Martins WP, Odibo AO, Papageorghiou AT, Salomon LJ, Thilaganathan B, ISUOG CSC Pre-eclampsia Task Force. ISUOG practice guidelines 2019: role of ultrasound in screening and follow-up of pre-eclampsia. UOG. 2019;53:7–22.
Tan MY, Wright D, Syngelaki A, Akolekar R, Cicero S, Janga D, Singh M, Greco E, Wright A, Maclagan K, Poon LC, Nicolaides KH. Comparison of diagnostic accuracy of early screening for pre-eclampsia by NICE guidelines and a method combining maternal factors and biomarkers: results of SPREE. Ultrasound Obstet Gynecol. 2018;51:743–50.
Alfirevic Z, Stampalija T, Dowswell T. Fetal and umbilical Doppler ultrasound in high-risk pregnancies. Cochrane Database Syst Rev. 2017;6:CD007529.
Biljan M, Haddad N, McVey K, Williams J. Efficiency of continuous-wave Doppler in screening high risk pregnancies in a district general hospital (a prospective randomized study on 674 singleton pregnancies). Proceedings of 26th British Congress of Obstetrics and Gynaecology; 1992 July7–10; Manchester, UK.
Burke G, Stuart B, Crowley P, Ni Scanaill S, Drumm J. Does Doppler ultrasound alter the management of high-risk pregnancy? Care concern and cure in perinatal medicine. 13th European Congress of Perinatal Medicine; 1992 May; Amsterdam, The Netherlands. Parthenon; 1992. pp. 597–604.
De Rochambeau B, Jabbour N, Mellier G. Umbilical Doppler velocimetry in prolonged pregnancies [La velocimetrie Doppler ombilicale dans les grossesses prolongees]. Revue Francaise de Gynecologie et d Obstetrique. 1992;87(5):289–94.
Giles W, Bisits A, O’Callaghan S, Gill A, DAMP Study Group. The Doppler assessment in multiple pregnancy randomised controlled trial of ultrasound biometry versus umbilical artery Doppler ultrasound and biometry in twin pregnancy. BJOG. 2003;110(6):593–7.
Johnstone FD, Prescott R, Hoskins P, Greer IA, McGlew T, Compton M. The effect of introduction of umbilical Doppler recordings to obstetric practice. Br J Obstet Gynaecol. 1993;100:733–41.
Neales K. (St. Mary’s Hospital, Manchester, UK). [personal communication]. Letter to: Z Alfirevic (Department of Women’s and Children’s Health, The University of Liverpool, Liverpool, UK) 24 January 1994; Vol. Located at: Cochrane Office, Department of Women’s and Children’s Health, The University of Liverpool, Liverpool, UK.
Newnham JP, O’Dea MRA, Reid KP, Diepeveen DA. Doppler flow velocity waveform analysis in high risk pregnancies: a randomized controlled trial. Br J Obstet Gynaecol. 1991;98:956–63.
Nienhuis SJ, Vles JS, Gerver WJ, Hoogland HJ. Doppler ultrasonography in suspected intrauterine growth retardation: a randomized clinical trial. Ultrasound Obstet Gynecol. 1997;9(1):6–13.
Nimrod C, Yee J, Hopkins C, Pierce P, Lange I, Fick G, et al. The utility of pulsed Doppler studies in the evaluation of postdate pregnancies. J Matern Fetal Invest. 1992;1:127.
Norman K, Pattinson RC, Carstens E. Doppler velocimetry in recurrent pregnancy loss: is there a role? Proceedings of 11th Conference on Priorities in Perinatal Care in South Africa; 1992 March; Caledon, South Africa; 1992. pp. 71–74.
Ott WJ, Mora G, Arias F, Sunderji S, Sheldon G. Comparison of the modified biophysical profile to a new biophysical profile incorporating the middle cerebral artery to umbilical artery velocity flow systolic/diastolic ratio. Am J Obstet Gynecol. 1998;178(6):1346–53.
Pattinson RC, Norman K, Odendaal HJ. The role of Doppler velocimetry in the management of high risk pregnancies. Br J Obstet Gynaecol. 1994;101:114–20.
Trudinger BJ, Cook CM, Giles WB, Connelly AJ, Thompson RS. Umbilical artery flow velocity waveforms in high-risk pregnancy: randomised controlled trial. Lancet. 1987;1:188–90.
Tyrrell SN, Lilford RJ, MacDonald HN, Nelson EJ, Porter J, Gupta JK. Randomized comparison of routine vs highly selective use of Doppler ultrasound and biophysical scoring to investigate high risk pregnancies. Br J Obstet Gynaecol. 1990;97:909–16.
Almstrom H, Axelsson O, Cnattingius S, Ekman G, Maesel A, Ulmsten U, Armstrom K, Marsal K. Comparison of umbilical artery velocimetry and cardiotocography for surveillance of small-for-gestational-age fetuses. Lancet. 1992;340:936–40.
Haley J, Tuffnell DJ, Johnson N. Randomised controlled trial of cardiotocography versus umbilical artery Doppler in the management of small for gestational age fetuses. Br J Obstet Gynaecol. 1997;104(4):431–5.
Hofmeyr GJ, Pattinson R, Buckley D, Jennings J, Redman CWG. Umbilical artery resistance index as a screening test for fetal well-being. II. Randomized feasibility study. Obstet Gynecol. 1991;78:359–62.
Williams KP, Farquharson DF, Bebbington M, Dansereau J, Galerneau F, Wilson RD, Shaw D, Kent N. Screening for fetal wellbeing in a high-risk pregnant population comparing the non-stress test with umbilical artery Doppler velocimetry: a randomized controlled clinical trial. Am J Obstet Gynecol. 2003;188(5):1366–71.
Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Lancet. 2001;357(9263):1191–4.
Westergaard HB, Langhoff-Roos J, Lingman G, Marsal K, Kreiner S. A critical appraisal of the use of umbilical artery Doppler ultrasound in high-risk pregnancies: use of meta-analyses in evidence-based obstetrics. Ultrasound Obstet Gynecol. 2001;17:466–76.
Alfirevic Z, Neilson JP. Doppler ultrasonography in high risk pregnancies: systematic review with meta-analysis. Am J Obstet Gynecol. 1995;172:379–87.
Neilson JP, Alfirevic Z. Doppler ultrasound for fetal assessment in high risk pregnancies. Cochrane Database Syst Rev. 1995;(1). https://doi.org/10.1002/14651858.CD000073.
Alfirevic Z, Stampalija T, Gyte GML. Fetal and umbilical Doppler ultrasound in high-risk pregnancies. Cochrane Database Syst Rev. 2010;(1). https://doi.org/10.1002/14651858.CD007529.pub2.
Alfirevic Z, Stampalija T, Gyte GML. Fetal and umbilical Doppler ultrasound in high-risk pregnancies. Cochrane Database Syst Rev. 2013;(11). https://doi.org/10.1002/14651858.CD007529.pub3.
Royal College of Obstetrics & Gynecologists (RCOG). Green-top guideline no.31. The investigation and management of the small-for-gestational-age fetus. 2013.
Gordijn SJ, Beune IM, Thilaganathan B, Papageorghiou A, Baschat AA, Baker PN, Silver RM, Wynia K, Ganzevoort W. Consensus definition for placental fetal growth restriction: a Delphi procedure. Ultrasound Obstet Gynecol. 2016;48(3):333–9.
Unterscheider J, Daly S, Geary MP, Kennelly MM, McAuliffe FM, O’Donoghue K, Hunter A, Morrison JJ, Burke G, Dicker P, Tully EC, Malone FD. Optimizing the definition of intrauterine growth restriction: the multicenter prospective PORTO study. Am J Obstet Gynecol. 2013;208(4):290–2.
Burton GJ, Woods AW, Jauniaux E, Kingdom JC. Rheological and physiological consequences of conversion of the maternal spiral arteries for uteroplacental blood flow during human pregnancy. Placenta. 2009;30(6):473–82.
Kurkinen-Räty M, Kivelä A, Jouppila P. The clinical significance of an absent end-diastolic velocity in the umbilical artery detected before the 34th week of pregnancy. Acta Obstet Gynecol Scand. 1997;76(5):398–404.
Bilardo CM, Wolf H, Stigter RH, Ville Y, Baez E, Visser GHA, Hecher K. Relationship between monitoring parameters and outcome in severe, early intrauterine growth restriction. Ultrasound Obstet Gynecol. 2004;23:119–25.
Kiserud T, Kessler J, Ebbing C, Rasmussen S. Ductus venosus shunting in growth-restricted fetuses and the effect of umbilical circulatory compromise. Ultrasound Obstet Gynecol. 2006;28(2):143–9.
Ferrazzi E, Lees C, Acharya G. The controversial role of the ductus venosus in hypoxic human fetuses. Acta Obstet Gynecol Scand. 2019;98(7):823–9.
Raju TN, Mercer BM, Burchfield DJ, Joseph GFJ. Periviable birth: executive summary of a joint workshop by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, American Academy of Pediatrics, and American College of Obstetricians and Gynecologists. Obstet Gynecol. 2014;123(5):1083–96.
EXPRESS Group. Incidence of and risk factors for neonatal morbidity after active perinatal care: extremely preterm infants study in Sweden (EXPRESS). Acta Paediatr. 2010;99(7):978–92.
Baschat AA, Cosmi E, Bilardo CM, Wolf H, Berg C, Rigano S, Germer U, Moyano D, Turan S, Hartung J, Bhide A, Müller T, Bower S, Nicolaides KH, Thilaganathan B, Gembruch U, Ferrazzi E, Hecher K, Galan HL, Harman CR. Predictors of neonatal outcome in early-onset placental dysfunction. Obstet Gynecol. 2007;109(2 Pt 1):253–61.
Lees C, Marlow N, Arabin B, Bilardo CM, Brezinka C, Derks JB, Duvekot J, Frusca T, Diemert A, Ferrazzi E, Ganzevoort W, Hecher K, Martinelli P, Ostermayer E, Papageorghiou AT, Schlembach D, Schneider KT, Thilaganathan B, Todros T, van Wassenaer-Leemhuis A, Valcamonico A, Visser GH, Wolf H, TRUFFLE Group. Perinatal morbidity and mortality in early-onset fetal growth restriction: cohort outcomes of the trial of randomized umbilical and fetal flow in Europe (TRUFFLE). Ultrasound Obstet Gynecol. 2013;42(4):400–8.
Lees CC, Marlow N, van Wassenaer-Leemhuis A, Arabin B, Bilardo CM, Brezinka C, Calvert S, Derks JB, Diemert A, Duvekot JJ, Ferrazzi E, Frusca T, Ganzevoort W, Hecher K, Martinelli P, Ostermayer E, Papageorghiou AT, Schlembach D, Schneider KT, Thilaganathan B, Todros T, Valcamonico A, Visser GH, Wolf H, TRUFFLE Study Group. 2 year neurodevelopmental and intermediate perinatal outcomes in infants with very preterm fetal growth restriction (TRUFFLE): a randomised trial. Lancet. 2015;385(9983):2162–72.
Bilardo CM, Hecher K, GHA V, Papageorghiou AT, Marlow N, Thilaganathan B, Van Wassenaer-Leemhuis A, Todros T, Marsal K, Frusca T, Arabin B, Brezinka C, Derks JB, Diemert A, Duvekot JJ, Ferrazzi E, Ganzevoort W, Martinelli P, Ostermayer E, Schlembach D, Valensise H, Thornton J, Wolf H, Lees C, TRUFFLE Group. Severe fetal growth restriction at 26-32 weeks: key messages from the TRUFFLE study. Ultrasound Obstet Gynecol. 2017;50(3):285–90.
Savchev S, Figueras F, Sanz-Cortes M, Cruz-Lemini M, Triunfo S, Botet F, Gratacos E. Evaluation of an optimal gestational age cut-off for the definition of early- and late-onset fetal growth restriction. Fetal Diagn Ther. 2014;36(2):99–105.
Crimmins S, Desai A, Block-Abraham D, Berg C, Gembruch U, Baschat AA. A comparison of Doppler and biophysical findings between liveborn and stillborn growth-restricted fetuses. Am J Obstet Gynecol. 2014;211(6):669.e1–669.e10.
Cruz-Martínez R, Figueras F, Hernandez-Andrade E, Oros D, Gratacos E. Fetal brain Doppler to predict cesarean delivery for nonreassuring fetal status in term small-for-gestational-age fetuses. Obstet Gynecol. 2011;117(3):618–26.
Severi FM, Bocchi C, Visentin A, Falco P, Cobellis L, Florio P, Zagonari S, Pilu G. Uterine and fetal cerebral Doppler predict the outcome of third-trimester small-for-gestational age fetuses with normal umbilical artery Doppler. Ultrasound Obstet Gynecol. 2002;19(3):225–8.
Hershkovitz R, Kingdom JC, Geary M, Rodeck CH. Fetal cerebral blood flow redistribution in late gestation: identification of compromise in small fetuses with normal umbilical artery Doppler. Ultrasound Obstet Gynecol. 2000;15(3):209–12.
Oros D, Figueras F, Cruz-Martinez R, Padilla N, Meler E, Hernandez-Andrade E, Gratacos E. Middle versus anterior cerebral artery Doppler for the prediction of perinatal outcome and neonatal neurobehavior in term small-for-gestational-age fetuses with normal umbilical artery Doppler. Ultrasound Obstet Gynecol. 2010;35(4):456–61.
Eixarch E, Meler E, Iraola A, Illa M, Crispi F, Hernandez-Andrade E, Gratacos E, Figueras F. Neurodevelopmental outcome in 2-year-old infants who were small-for-gestational age term fetuses with cerebral blood flow redistribution. Ultrasound Obstet Gynecol. 2008;32(7):894–9.
Meher S, Hernandez-Andrade E, Basheer SN, Lees C. Impact of cerebral redistribution on neurodevelopmental outcome in small-for-gestational-age or growth-restricted babies: a systematic review. Ultrasound Obstet Gynecol. 2015;46(4):398–404.
Hernandez-Andrade E, Stampalija T, Figueras F. Cerebral blood flow studies in the diagnosis and management of intrauterine growth restriction. Curr Opin Obstet Gynecol. 2013;25(2):138–44.
DeVore GR. The importance of the cerebroplacental ratio in the evaluation of fetal well-being in SGA and AGA fetuses. Am J Obstet Gynecol. 2015;213(1):5–15.
Vollgraff Heidweiller-Schreurs CA, De Boer MA, Heymans MW, Schoonmade LJ, Bossuyt PMM, Mol BWJ, De Groot CJM, Bax CJ. Prognostic accuracy of cerebroplacental ratio and middle cerebral artery Doppler for adverse perinatal outcome: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2018;51(3):313–22.
Conde-Agudelo A, Villar J, Kennedy SH, Papageorghiou AT. Predictive accuracy of cerebroplacental ratio for adverse perinatal and neurodevelopmental outcomes in suspected fetal growth restriction: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2018;52(4):430–41.
McCowan LM, Figueras F, Anderson NH. Evidence-based national guidelines for the management of suspected fetal growth restriction: comparison, consensus, and controversy. Am J Obstet Gynecol. 2018;218(2S):S855–68.
Figueras F, Gratacos E. An integrated approach to fetal growth restriction. Best Pract Res Clin Obstet Gynaecol. 2017;38:48–58.
Baschat AA. Planning management and delivery of the growth-restricted fetus. Best Pract Res Clin Obstet Gynaecol. 2018;49:53–65.
Stampalija T, Arabin B, Wolf H, Bilardo CM, Lees C, TRUFFLE Investigators. Is middle cerebral artery Doppler related to neonatal and 2-year infant outcome in early fetal growth restriction? Am J Obstet Gynecol. 2017;216(5):521.e1–521.e13.
Stampalija T, Arabin B, Wolf H, Bilardo CM, Lees C. An abnormal cerebroplacental ratio (CPR) is predictive of early childhood delayed neurodevelopment in the setting of fetal growth restriction. Am J Obstet Gynecol. 2019;221(3):273.e1–9. Epub ahead of print.
Monteith C, Flood K, Pinnamaneni R, Levine TA, Alderdice FA, Unterscheider J, McAuliffe FM, Dicker P, Tully EC, Malone FD, Foran A. An abnormal cerebroplacental ratio (CPR) is predictive of early childhood delayed neurodevelopment in the setting of fetal growth restriction. Am J Obstet Gynecol. 2019;221(3):273.e1–9.
Stampalija T, Thorton J, Marlow N, Napolitano R, Bhide A, et al.; TRUFFLE-2 Group. Fetal cerebral Doppler changes and outcome in late preterm growth restriction: a prospective cohort study. Ultrasound Obstet Gynecol. 2020;56(2):173–181.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Lees, C.C., Stampalija, T. (2023). Fetal Doppler Velocimetry in High-Risk Pregnancies: Randomized Clinical Trials. In: Maulik, D., Lees, C.C. (eds) Doppler Ultrasound in Obstetrics and Gynecology. Springer, Cham. https://doi.org/10.1007/978-3-031-06189-9_26
Download citation
DOI: https://doi.org/10.1007/978-3-031-06189-9_26
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-06188-2
Online ISBN: 978-3-031-06189-9
eBook Packages: MedicineMedicine (R0)