Abstract
Introduction.
Hyperemesis gravidarum (HG) is associated with higher levels of serum β-hCG levels and hyperthyroidism. Interleukin-6 (IL-6), a pro-inflammatory cytokine, is reported to enhance secretion of β-hCG from trophoblastic cell line.
Methods.
We measured serum levels of IL-6, thyroid hormones and β-hCG of hyperemetic patients and gestational age-matched controls to search for a difference between the two groups.
Results.
There was a significant difference in β-hCG (p=0.028), though IL-6 levels were higher in the hyperemetic group, it did not reach a significant level. Interleukin-6 positively correlated with β-hCG (r=0.38 and p=0.13).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Interleukin-6 (IL-6), a cytokine involved in inflammation, cell growth and differentiation, and immune responses, is produced primarily by activated monocyte/macrophages and T lymphocytes. Trophoblast-derived cytokines, IL-6 and IL-1 were reported to be capable of inducing trophoblasts to secrete human chorionic gonadotropin (hCG) through a different pathway used by a GnRH analogue [9, 12, 16]. In addition, trophoblast appears to be the major source of IL-6 in in vitro models [7].
Hyperemesis gravidarum (HG) is defined as vomiting sufficiently pernicious to produce weight loss, dehydration, electrolyte abnormalities, and affects 1–20 per 1,000 pregnant women [3]. Immunologic factors such as immune globulins, complement 3, complement 4 and lymphocyte counts were found to be significantly higher in HG, which might assign a role to immunologic activity [8]. If thyrotoxicosis accompanies hyperemesis, mean serum β-hCG, IgG and IgM levels rise to a higher extent. These factors may exaggerate the stimulatory effect of β-hCG. Therefore we decided to detect serum levels of total and free thyroid hormones, thyroid stimulating hormone (TSH), total β-hCG, and IL-6 levels in patients with HG and compare the results with gestational age-matched controls.
Materials and methods
The study was approved by the local ethical committee of the university hospital. We hospitalised 10 first trimester primigravida with HG (group H). Mean gestational age was 8.7±0.7 weeks. They were told about the research project and informed consents were obtained. They had nausea and vomiting at least four times a day, lost appetite and could not tolerate oral nutrition. Three of the patients had electrolyte abnormalities, 7 had ketonuria. Before beginning the therapy, blood was withdrawn, serum was separated and kept at −70°C. To serve as the control group, 10 healthy, gestational age-matched pregnant women were asked to give blood samples at their routine visits (group C), serum was separated and kept at −70°C. Mean gestational age was 10.1±0.9 weeks. Patients with a chronic disease or multiple pregnancy were not included in the study.
After collection of all samples, serum levels of total and free thyroid hormones, TSH and total β-hCG were measured by using ACS:180 Automated Chemiluminescence Systems (Bayer, NY, USA). Interleukin-6 was measured by using an IL ELISA kit from Diaclone company (Diaclone, France). Analytic sensitivity was 2 pg/ml and intra-assay coefficient of variation was 3.86% for 28.7 pg/ml.
Mann-Whitney-U and Pearson's correlation analysis were used for statistical analysis, p<0.05 was accepted as significant. All data are expressed as mean ± SEM.
Results
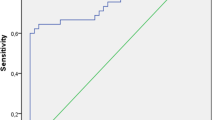
Demographic data of the patients are seen in Table 1. There was no difference regarding the age and gestational age. Hormone and IL results are seen in Table 2. Mean serum β-hCG (127,606±11,555 vs. 76,169±11,984; p=0.028) level in group H was significantly higher than group C. Though IL-6 was higher in group H, (5.6±0.9 vs. 3.2±0.3; p=0.20) it did not reach a significant level. There was no significant difference in the thyroid profile. A moderate positive correlation between IL-6 and β-hCG (r=0.36 and p=0.12) is seen in Fig. 1.
Discussion
Interleukin-6 levels in the sera of pregnant women at all trimesters showed no difference from those in non-pregnant women at any stage of the menstrual cycle [10]. When IL-6 was detected in culture of conception products from both first trimester and term groups, term villi were found to produce higher amount compared with the first trimester, which revealed that IL-6 production by the placenta was developmental stage-specific [1]. In another study, IL-6 concentration was significantly higher in the coelomic fluid than in the amniotic fluid and positively correlated with gestational age [6]. Immunostaining for IL-6 was present in both syncytiotrophoblast and extra-villous trophoblast, and IL-6 was significantly higher in decidual than in placental tissues. The authors concluded that trophoblast-derived IL-6 was the major source for this cytokine. During the first trimester, IL-6 could play a role not only in tissue remodelling associated with placentation, but also in the hematopoetic function of the secondary yolk sac and also in the generation of new vessels in placental villous tissue.
On the contrary to the previous reports, in one study, IL-6 did not change the cytotrophoblastic secretion of total hCG, but induced a dose-dependent stimulation of leptin secretion and increased the activity, but not the immunoreactivity, of the matrix metalloproteinases MMP-9 and MMP-2 which were involved in trophoblastic invasion during implantation [11]. These results indicate that IL-6 could be considered as an endometrio-trophoblastic regulator of cytotrophoblastic gelatinases.
As IL-6 could induce trophoblast to secrete hCG, and HG is a syndrome with higher production of hCG and thyroid hormones, we measured the thyroid profile and IL-6 to see if they differed from normal first trimester pregnant patients. Though IL-6 levels were somewhat higher than control group, it did not reach a significant level probably due to small sample size. But IL-6 and hCG had a positive correlation, which might make us consider that higher hCG levels could be due to induction caused by IL-6.
Steroids can be used in persistent vomiting of HG refractory to conventional therapy [14, 15]. The drug is considered to exert its effect through the chemoreceptor trigger zone located in the brain stem. Probably the steroids can lower IL levels and reduce inflammatory response of the patients. Immunologic activity seen in patients with HG [8], and dramatic response to short course of steroid therapy may be the clues to accept HG as an inflammatory response of pregnancy.
We did not find a difference in the thyroid profile between the two groups. Both total and free forms of the hormones were similar. Transient hyperthyroidism has been reported in about 60% of patients with HG [4], and the increase in thyroid hormones are attributable to either higher hCG concentrations, to hCG-hypersensitive thyrotropin receptors of an overactive thyroid [13], or probable secretion of a variant of hCG with increased thyroid-stimulating activity [5]. Besides the overactivity of the thyroid due to these several mechanisms, elevated levels of reverse T3, an inactive product converted from T4, has been reported [2]. All patients with HG need not to have hyperthyroidism, and increase in reverse T3 may reflect the slowing of the patients' metabolism against relatively low food intake. Though our patients had significantly higher hCG levels than the control group, they did not have thyrotoxicosis. Maybe hCG was not high enough to stimulate the thyroid, or the glands of the patients were not highly sensitive to the hCG.
In conclusion, IL-6 levels could rise in patients with HG and this could lead to higher levels of hCG seen in these patients. Dramatic response to steroid therapy could be mediated through the anti-inflammatory action of the drug as well as affecting the chemoreceptor trigger zone.
References
Agarwal R, Loganath A, Roy AC, Wong YC, Lindoff C, Ng SC (2000) Increased expression of interleukin 6 in term compared to the first trimester human placental villi. Horm Metab Res 332:164–168
Asakura H, Watanabe S, Sekiguchi A, Power GC, Araki T (2000) Severity of hyperemesis gravidarum correlates with serum levels of reverse T3. Arch Gynecol Obstet 264:57–62
Fairweather DVI, Loraine JA (1968) Nausea and vomiting in pregnancy. Am J Obstet Gynecol 102:135–173
Goodwin TM, Montero M, Mestman JH (1992) Transient hyperthyroidism and hyperemesis gravidarum: clinical aspects. Am J Obstet Gynecol 167:648–652
Hershman JM (1999) Human chorionic gonadotropin and the thyroid: hyperemesis gravidarum and trophoblastic tumors. Thyroid 9:653–657
Jauniaux E, Gulbis B, Schandene L, Collette J, Hustin J (1996) Distribution of interleukin-6 in maternal and embryonic tissues during the first trimester. Mol Hum Reprod 2:239–243
Kameda T, Matsuzaki N, Sawai K, Okada T, Saji F, Matsuda T, Hirano T, Kishimoto T, Tanizawa O (1990) Production of interleukin-6 by normal human trophoblast. Placenta 11:205–213
Leylek OA, Tayaksi M, Ercelsan T, Dokmetas S (1999) Immunologic and biochemical factors in hyperemesis gravidarum with or without hyperthyroxinemia. Gynecol Obstet Invest 47:229–234
Masuhiro K, Matsuzaki N, Nishino E, Taniguchi T, Kameda T, Li Y, Saji F, Tanizawa O (1991) Trophoblast-derived interleukin-1 (IL-1) stimulates the release of human chorionic gonadotropin by activating IL-6 and IL-6-receptor system in the first trimester human trophoblasts. J Clin Endocrinol Metab 72:594–601
Matsuzaki N, Neki R, Sawai K, Shimoya K, Okada T, Sakata M, Saji F, Koishihara Y, Ida N (1995) Soluble interleukin-6 (IL-6) receptor in the sera of pregnant women forms a complex with IL-6 and augments human chorionic gonadotropin production by normal human trophoblasts through binding to the IL-6 signal transducer. J Clin Endocrinol Metab 80:2912–2917
Meisser A, Cameo P, Islami D, Campana A, Bischof P (1999) Effects of interleukin-6 (IL-6) on cytotrophoblastic cells. Mol Hum Reprod 5:1055–1058
Nishino E, Matsuzaki N, Masuhiro K, Kameda T, Taniguchi T, Takagi T, Saji F, Tanizawa O (1990) Trophoblast-derived interleukin-6 (IL-6) regulates human chorionic gonadotropin release through IL-6 receptor on human trophoblasts. J Clin Endocrinol Metab 71:436–441
Rodien P, Bremont C, Sanson M-LR et al (1998) Familial gestational hyperthyroidism caused by a mutant thyrotropin receptor hypersensitive to human chorionic gonadotropin. N Engl J Med 339:1823–1826
Safari HR, Fassett MJ, Souter IC, Alsulyman OM, Goodwin TM (1998) The efficacy of methylprednisolone in the treatment of hyperemesis gravidarum: a randomized, double-blind, controlled study. Am J Obstet Gynecol 179:921–924
Taylor R (1996) Successful management of hyperemesis gravidarum using steroid therapy. QJM 89:103–107
Yanushpolsky EH, Ozturk M, Polgar K, Berkowitz RS, Hill JA (1993) The effects of cytokines on human chorionic gonadotropin (hCG) production by a trophoblast cell line. J Reprod Immunol 25:235–247
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kuscu, N.K., Yildirim, Y., Koyuncu, F. et al. Interleukin-6 levels in hyperemesis gravidarum. Arch Gynecol Obstet 269, 13–15 (2003). https://doi.org/10.1007/s00404-002-0412-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-002-0412-6