Abstract
Ceruminous carcinomas of the external auditory canal (EAC), encompassing adenoid cystic carcinoma (ACC), ceruminous adenocarcinoma (CA), and mucoepidermoid carcinoma (MEC), are extremely rare with little known regarding the influence of demographics, tumor characteristics, and treatment on survival. This study aimed to summarize existent data and describe prognostic factors affecting survival in ceruminous carcinoma. Cases of ceruminous carcinoma of the EAC in the Surveillance, Epidemiology, and End Results (SEER) database were analyzed to provide demographic, cancer-related, and treatment data and assess their influence on disease-specific and overall survival. A literature review was also performed. No significant difference in overall survival (OS) existed for localized versus regional disease, tumor type, or use of radiation therapy. In those with ACC, distant disease had a lower OS compared to regional disease. On review of the literature, local recurrence was a common finding with a low risk for nodal metastasis in ACC and CA. In conclusion, local recurrence was common despite aggressive surgical intervention (± radiation therapy); overall survival was unaffected by radiation therapy, tumor type, or local versus regional disease; and more cases of MEC are needed for analysis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A small proportion (~ 0.2%) of head and neck cancers occur in the external auditory canal (EAC) [25, 39, 46, 49]. The majority of these tumors are squamous cell carcinoma (~ 70%), with basal cell carcinoma, melanoma, Merkel cell carcinoma, lymphoma, angiosarcoma, and ceruminous neoplasms comprising the remainder [21].
Ceruminous neoplasms arise from distinct, modified apocrine glands known as ceruminous glands [14]. Each person has 1000–2000 ceruminous glands confined to the skin of the outer third of the EAC. Tumors of these glands are exceedingly rare and account for < 0.001–2.4% of neoplasms in this location [14, 21, 39, 46]. The World Health Organization (WHO) separates ceruminous tumors of the EAC into benign adenomas and malignant adenocarcinomas [49]. The adenocarcinomas are further distinguished, based on histologic features, into ceruminous adenocarcinoma (CA), adenoid cystic carcinoma (ACC), and mucoepidermoid carcinoma (MEC). Importantly, ACC and MEC originating in the EAC are histologically indistinguishable from a primary salivary gland ACC or MEC. As such, to make a definitive diagnosis of a primary ceruminous gland neoplasm, extension of these tumors to adjacent salivary glands (i.e., parotid gland) must be excluded via preoperative imaging or intraoperatively [3].
ACC is the most common ceruminous gland malignancy of the EAC. The second most common is CA, with MEC being the least frequently reported [14, 39, 49]. Despite limited data, the malignant behavior of ceruminous carcinomas is well-documented with a propensity for local recurrence and metastatic potential [14]. As such, aggressive surgical resection with or without adjuvant radiation is advocated to ensure tumor removal [49, 57]. However, even with aggressive therapy, recurrences are common, and death can occur from metastasis and/or progression of loco-regional disease [14, 21, 57]. The degree to which these treatments influence survival remains largely unexplored and the rarity of ACC, CA, and MEC limits the available clinical, treatment, and prognostic data. The purpose of this study is to utilize population-based cancer data to describe patient demographics, assess prognostic utility of staging data, and examine the influence of various treatment modalities on overall survival for ceruminous carcinomas of the EAC. In addition, a review of the literature was performed to contextualize results from this study with historical cases.
Materials and methods
Patient cohort
This retrospective cohort study utilized the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) program, which draws from 21 population-based cancer registries to provide information on approximately 34.6% of the United States population. Patients included were diagnosed with CA, ACC, or MEC (World Health Organization’s International Classification of Disease for Oncology, 3rd edition: ICD-O-3 code 8420/3 [CA], 8200/3 [ACC], and 8430/3 [MEC]) of the external ear (C44.2) within the SEER database between 1975 and 2017. Ceruminous carcinomas occurring outside the external ear were excluded. Follow-up data were collected on available patients until 2017. All patient diagnoses were biopsy-proven and did not include patients who received clinical, radiographic, or posthumous diagnoses. Since SEER data are publicly available and de-identified, this study was exempt from institutional review board approval by The Ohio State University Human Research Protection Program.
Study variables and definitions
The following categorical variables were constructed: age (< 45, 45–55, 55–65, 65–75, 75–85, and > 85), race (White, African American, Native American/Native Alaskan, Asian, and other/unknown), ethnicity (Spanish–Hispanic–Latino or Non-Spanish–Hispanic–Latino), and treatment type (surgery only, radiation therapy only, chemotherapy only, or combinations thereof). Survivorship was categorized as either overall survival (OS) or disease-specific death (DSD). Follow-up time frames were collected as continuous variables in months. For missing data, the available case method was utilized.
The SEER Summary and Historic staging variables were used to classify tumors as localized, regional, and distant stage. Due to discrepancies between Summary and Historic staging variables, SEER Summary staging was prioritized if both Summary and Historic variables were present. Local stage is defined as a malignancy limited to the organ of origin. Regional stage is defined as a malignancy that either (1) extends beyond the organ of origin directly into surrounding tissue, (2) involves a regional lymph node via the lymphatic system, or (3) demonstrates both direct extension and lymphatic spread beyond the site of origin. Distant stage is defined as tumors involving a distant organ or lymph node by noncontiguous metastases or by direct extension. For unstaged tumors, information is insufficient to assign staging.
Statistical analysis
Dichotomous and categorical variables were defined with proportions. Continuous variables were described with means, standard deviations, and ranges. Age-adjusted incidence rates, rate ratios, and trends were analyzed based on the year 2000 U.S. standard population. For incidence calculations, a 16-year study period (2000–2016) was chosen with data drawn from 18 available SEER registry groupings. Rates were calculated as new cases per year per 1,000,000 persons. Kaplan–Meier (KM) curves were used to describe time-to-event data with overall survival as the outcome variable. A log-rank test was used to complete pairwise-comparison of KM curves. The Cox proportional hazards model, adjusted for age, gender, race and ethnicity, SEER summary stage, and primary treatment, was used to model overall survival given the infrequency of disease-specific death. The proportional hazards assumption was evaluated with a Schoenfeld residuals test. A two-sided p value of less than 0.05 was considered statistically significant. Statistical analyses were performed on Stata 15.1 (College Station, TX), aside from incidence calculations performed on SEER*Stat 8.3.6.1 (Calverton, MD).
Literature review method
The PubMed database was searched using the following terms: (cerum* OR cylindroma OR adenoid cystic carcinoma OR ceruminous adenocarcinoma OR mucoepidermoid carcinoma) AND (ear OR external auditory canal). Cylindroma was included as a search term since previous sources used cylindroma as a synonym for ACC [54]. Eligible articles were published in English and contained human cases. Articles with parotid gland involvement were excluded since the primary site of origin cannot be distinguished. References of each article were searched for relevant cases. Case reports were included due to the low number of case series, cohort studies, and literature reviews. Recorded variables from each article included the number of cases; treatment(s); the presence of local recurrence, nodal metastases, and/or distant metastasis; DSD; OS; and follow-up duration.
Results
Cohort description
The SEER cohort comprised of 135 individuals diagnosed with ceruminous carcinoma. Table 1 provides a summary of the demographic, therapeutic, and survival characteristics. Age-adjusted incidence rates were analyzed using rate ratios with white as the referent group for race and male as the referent group for gender. During the incidence study period (2000–2016), a total of 93 cases of ceruminous carcinomas occurred with an age-adjusted incidence of 0.064 (95% CI 0.051–0.078) cases per year per 1,000,000 persons. The incidence of ceruminous carcinoma decreased over the study period with an annual percent change of − 3.8% (95% CI − 7.705–0.196). In general, ceruminous carcinoma tended to affect female patients to a greater degree (~ 1.5:1 ratio), but this was not statistically significant. Similarly, there were no significant differences in incidence between races both as a whole and between tumor subtypes.
A total of 98 cases of ACC were identified. The age-adjusted incidence was 0.047 (95% CI 0.037–0.060) cases per year per 1,000,000 persons, based on 69 cases during the incidence study period. A similar distribution occurred among the age groups studied with a small peak in incidence in the 5th decade of life. Regional disease was noted in 30 cases, and of these, 24 had further lymph node evaluation with only 1/24 demonstrating metastatic lymph node involvement. Surgical intervention (n = 59, 78%) and radiation therapy (n = 48, 63%) were most commonly included as part of the primary treatment modality. Twelve patients (12%) died as a result of their tumor and fifty-six patients (57%) were alive at the conclusion of the study period.
A total of 33 patients with CA were identified. The age-adjusted incidence was 0.015 (95% CI 0.010–0.023) cases per year per 1,000,000 persons, based on 22 cases during the incidence study period. Males and females had similar age-adjusted incidence rates and the majority of patients were 55–75 years of age (n = 17, 51%). Treatment data were available for 67% of patients and surgical intervention was the most commonly reported (n = 20/22, 91%). Radiation therapy was frequently utilized with over half of the cohort (n = 12, 55%) receiving radiation with or without surgery. Survival characteristics showed 2 patients died from their disease (6%) and 19 (58%) were alive at the conclusion of the study period.
A total of four patients with MEC of the EAC were identified. One patient was found to have distant disease at diagnosis. One patient died as a result of their tumor and one (25%) was alive at the conclusion of the study.
Survival characteristics
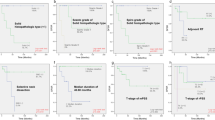
A log-rank test of the KM curves for the ACC cohort found regional tumor stage had a higher OS compared to distant tumor stage (p < 0.001). However, when comparing localized versus regional stage for ACC, log-rank testing of the survival curves demonstrated no significant difference in survival (p = 0.510). For the CA cohort, there was no difference in OS between localized and regional tumor stage (p = 0.589). Due to an insufficient number of patients, distant tumor stage for the CA cohort was not included in the analyses.
When comparing OS between the two most common tumor subtypes, ACC and CA, the KM curves demonstrated no statistical difference (p = 0.963) (Fig. 1). Additionally, when treatment groups were dichotomized into radiation versus no radiation, comparison between treatment groups demonstrated no difference in survival for either ACC (p = 0.614) (Fig. 2) or CA (p = 0.255) (Fig. 3). Quantitative survival analysis of MEC is limited by the small sample size.
On univariable and multivariable analysis, patients with distant disease in the ACC cohort were at increased risk of death compared to those with localized disease (univariable: HR = 7.64; 95% CI 2.65–22.06; p < 0.01) (multivariable: HR = 16.63; 95% CI 2.80–98.92; p = 0.002). However, gender, race/ethnicity, regional disease, and primary treatment modality did not significantly affect survival (Table 2). Of note, Schoenfeld residual testing supported the proportional hazards assumption (p = 0.964). Due to an insufficient number of patients, multivariable and univariable analysis of the CA and MEC cohorts were not included in the analyses.
Literature review
A total of 52 articles were included for review and summarized in Table 3. ACC was reported most frequently (n = 199) followed by CA (n = 45) and then MEC (n = 8). Most cases had surgical intervention either as the only treatment or in combination with radiation. Radiation monotherapy and adjuvant chemotherapy were not frequently reported. Additionally, local recurrence was common for each cohort (42% ACC, 49% CA, 38% MEC); however, nodal metastasis rates were low for CA (0%) and ACC (4%) despite higher distant metastasis rates (13% CA, 24% ACC). Of the 8 MEC cases, 2 (29%) had nodal metastasis and 1 (14%) had distant metastasis. Regarding survivorship, CA had the highest DSD rate (27%) and the lowest OS rate (56%) compared to ACC (DSD 18%, OS 74%) and MEC (DSD 14%, OS 86%).
Discussion
Comparable to previous studies, this analysis found ACC was the most frequently reported ceruminous neoplasm [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57]. Published data regarding gender predilection for ceruminous carcinomas are mixed, with studies showing ACC more prevalent among females, equal gender distribution for CA, and MEC favoring males [34,35,36,37,38, 44, 46]. However, this study found there were no statistically significant gender preferences in the subtypes of ceruminous carcinoma. Additionally, no racial predilection was observed for ceruminous carcinoma and its subtypes. Consistent with previous reports, this analysis shows ceruminous carcinoma primarily affects adults in their 5th–7th decade of life [14, 39, 46].
An important finding from this study is the lack of a statistical difference in OS between CA and ACC (p = 0.963). This is in contrast to a previous report noting an improved OS for ACC compared to CA (mean survival of 100 months and 56 months, respectively) [14]. As shown in Fig. 1, the two cancers demonstrated comparable survival curves with similar mean follow-up times (111 months for ACC, 107 months for CA).
Given its risk of local recurrence and metastasis, adjuvant radiation therapy remains a common treatment modality for ceruminous carcinoma. However, objective evidence that radiation therapy improves outcomes is lacking. In a similar SEER investigation on CA, the authors noted that patients receiving adjuvant radiation therapy had shorter survival times [46]. Conversely, as demonstrated in Fig. 3 of this investigation, radiation therapy had no significant impact on survival time for CA (Fig. 2 also demonstrates no impact in ACC). There is a separation of the KM curves when the number at risk is low (the right-hand side of the curve); however, given the low numbers included in the risk set at this point, no conclusions can be made about survivorship. Of note, given the relative lack of specific staging and patient-level data available in SEER, patient and tumor characteristics that may confound this relationship remain.
Previously reported DSD rates trended higher for ACC (18%; 95% CI 13–23) and CA (27%; 95% CI 14–40) (Table 3) when compared to the present findings (12% ACC [95% CI 5–19], 6% CA [95% CI − 2–14]) (Table 1), though in each case confidence intervals do cross. Considerable variation in DSD for MEC is to be expected given its rarity. In contrast, overall survival rates for ACC and MEC were lower in the present study relative to previously published values (Table 3). This may be partially explained by the longer mean follow-up periods for patients in SEER leading to higher observed death rates. Interestingly, previously reported treatment strategies also differ from SEER data. In most subtypes in SEER, surgical monotherapy was employed for a minority of patients and radiation, as either monotherapy or in combination, was frequently utilized. This may reflect an emerging trend in treatment strategies given ceruminous carcinoma’s propensity for locally aggressive and metastatic behavior.
Despite increasingly aggressive treatment measures, high local recurrence rates remains a persistent issue (42% ACC, 49% CA, 38% MEC) (Table 3). The malignant potential of ceruminous carcinoma is well known. However, recent studies have demonstrated that metastatic involvement tends to be distant with rare reports of lymph node involvement (Table 3) [14, 23, 32]. These assertions are supported by the SEER data demonstrating only 1 ACC patient with regional lymph node involvement (of 24 with lymph node evaluation). This finding provides interesting insight into the unique malignant behavior of ACC (± other ceruminous carcinomas) and may provide an explanation for the non-impact of adjuvant radiation therapy on overall survival.
Limitations
Certain variables (e.g., clinical presentation, local recurrence, restaging) are not recorded within SEER and, therefore, preclude observing disease progression and monitoring treatment response. Low sample sizes limit the power of this study. Additionally, SEER uses a primary skin site of the external ear which is not specific for the EAC. Finally, some cases of ceruminous carcinoma may have been primary parotid gland tumors with extension to the EAC and misclassified as a primary external ear neoplasm.
Conclusion
Ceruminous carcinomas of the EAC are exceedingly rare tumors with high local recurrence rates and metastatic potential. Outcomes-based data on optimal treatment strategies are limited by tumor infrequency, and surgical intervention, with or without radiation therapy, remains the mainstay of treatment. In the present study, radiation therapy did not improve overall survival for ACC and CA. Survival appears unaffected by many variables except distant tumor stage. Future studies are needed to further elucidate the malignant behavior of ceruminous carcinomas and evaluate the utility of lymph node evaluation.
Availability of data and material
Data for this study are openly available in the Surveillance, Epidemiology, and End Results (SEER) database or by inquiry to the corresponding author.
Code availability
Not applicable.
References
Althaus SR, Ross JAT (1970) Cerumen Gland Neoplasia. Arch Otolaryngol 92(1):40–42
Arshad MH, Khalid U, Ghaffar S (2009) Adenoid cystic carcinoma of the external auditory canal. J Coll Phys Surg Pak 19(11):726–728
Bared A, Dave SP, Garcia M, Angeli SI (2007) Mucoepidermoid carcinoma of the external auditory canal (EAC). Acta Otolaryngol 127(3):280–284
Batsakis JG, Hardy GC, Hishiyama RH (1967) Ceruminous Gland Tumors. Arch Otolaryngol 86(1):66–69
Bilici S, Onur F, Sünter AV et al (2016) Ceruminous adenocarcinoma of external auditory canal: a case report. J Int Adv Otol 12(3):341–344
Brugler G (1992) Tumors presenting as aural polyps: a report of four cases. Pathology 24(4):315–319
Brunner H (1953) Basal cell carcinoma of the external auditory canal and middle ear. AMA Arch Otolaryngol 58(6):665–676
Cankar V, Crowley H (1964) Tumors of ceruminous glands. Cancer 17(1):67–75
Carvalho CP, Barcellos AN, Teixeira DC et al (2008) Adenoid cystic carcinoma of the external auditory canal. Brazil J Otorhinolaryngol 74(5):794–796
Chang C-H, Shu M-T, Lee J-C et al (2009) Treatments and outcomes of malignant tumors of external auditory canal. Am J Otolaryngol 30(1):44–48
Chung JH, Lee SH, Park CW, Tae K (2012) Mucoepidermoid carcinoma in the external auditory canal: a case report. Cancer Res Treat 44(4):275–278
Conlin PA, Mira JL, Graham SC et al (2002) Ceruminous gland adenoid cystic carcinoma with contralateral metastasis to the brain. Arch Path Lab Med 126(1):87–89
Coyas A, Adamopoulos G (1966) Cylindroma of the ear. J Laryngol Otol 80(8):860–862
Crain N, Nelson BL, Barnes EL, Thompson LDR (2009) Ceruminous gland carcinomas: a clinicopathologic and immunophenotypic study of 17 cases. Head Neck Pathol 3(1):1–17
Dalmaso M, Lippi L (1985) Adenoid cystic carcinoma of the head and neck: a clinical study of 37 cases. Laryngoscope 95(2):177–181
Dehner LP, Chen KTK (1980) Primary tumors of the external and middle ear: benign and malignant glandular neoplasms. Arch Otolaryngol 106(1):13–19
De Lucia A, Gambardella T, Carra P, Motta G (2004) A case of highly aggressive adenoid cystic carcinoma of the external auditory canal. Acta Otorhinolaryngol Ital 24(6):354–356
Dong F, Gidley PW, Ho T et al (2008) Adenoid cystic carcinoma of the external auditory canal. Laryngoscope 118(9):1591–1596
Fligiel Z, Kaneko M (1975) Extramammary Paget’s disease of the external ear canal in association with ceruminous gland carcinoma. A case report. Cancer 36(3):1072–1076
Goldman NC (1992) Adenoid cystic carcinoma of the external auditory canal. Otolaryngol Head Neck Surg 106(2):214–215
Green RW, Megwalu UC (2016) Adenoid cystic carcinoma of the external ear: a population based study. Am J Otolaryngol 37(4):346–350
Grossman A, Mathews WH, Gravanis MB (1964) Ceruminal adenoma of the middle ear and external ear canal. Laryngoscope 74(2):241–244
Gu F-M, Chi F-L, Dai C-F et al (2013) Surgical outcomes of 43 cases with adenoid cystic carcinoma of the external auditory canal. Am J Otolaryngol 34(5):394–398
Hageman MJ, Becker AE (1974) Intracranial invasion of a ceruminous gland tumor: follow-up of 12 years. Arch Otolaryngol 100(5):395–397
Hicks GW (1983) Tumors arising from the glandular structures of the external auditory canal. Laryngoscope 93(3):326–340
Iqbal A, Newman P (1998) Ceruminous gland neoplasia. Br J Plast Surg 51(4):317–320
Johnstone JM, Lennox B, Watson AJ (1957) Five cases of hidradenoma of the external auditory meatus: so-called ceruminoma. J Pathol 73(2):421–427
Juby HB (1957) Tumours of the ceruminous glands—so called ceruminoma. J Laryngol Otol 71(12):832–837
Kim CW, Rho Y-S, Cho SJ et al (2008) A case of ceruminous adenocarcinoma of the external auditory canal presenting as an aural polyp. Am J Otolaryngol 29(3):205–208
Lassaletta L, Patrón M, Olóriz J et al (2003) Avoiding misdiagnosis in ceruminous gland tumours. Auris Nasus Larynx 30(3):287–290
Liu Y, Sun J, Huang Y et al (2013) Metastatic adenoid cystic carcinoma of external auditory canal presenting as solitary pulmonary nodule. Thoracic Cancer 4(2):215–216
Liu H, Zhang Y, Zhang T et al (2017) Correlation between the pathology and clinical presentations in patients with adenoid cystic carcinoma of the external auditory canal. Head Neck 39(12):2444–2449
Lynde CW, McLean DI, Wood WS (1984) Tumors of ceruminous glands. J Am Acad Dermatol 11(5 Pt 1):841–847
Magliulo G, Ciniglio AM (2010) Mucoepidermoid carcinoma of the external auditory canal. Otolaryngol Head Neck Surg 142(4):624–625
Magliulo G, Ciniglio Appiani M, Colicchio MG et al (2012) Mucoepidermoid carcinoma of the external auditory canal. Otol Neurotol 33(3):e21-22
Magliulo G, Fusconi M, Pulice G (2003) Mucoepidermoid carcinoma of the external auditory canal: case report. Am J Otolaryngol 24(4):274–277
Michel RG, Woodard BH, Shelburne JD, Bossen EH (1978) Ceruminous gland adenocarcinoma. A light and electron microscopic study. Cancer 41(2):545–553
Mourad WF, Hu KS, Shourbaji RA, Harrison LB (2013) Trimodality approach for ceruminous mucoepidermoid carcinoma of the external auditory canal. J Laryngol Otol 127(2):203–206
Nagarajan P (2018) Ceruminous neoplasms of the ear. Head Neck Pathol 12(3):350–361
Neldner KH (1968) Ceruminoma. Arch Dermatol 98(4):344–348
Nyrop M, Grøntved A (2002) Cancer of the external auditory canal. Arch Otolaryngol Head Neck Surg 128(7):834–837
O’Neill PB, Parker RA (1957) Sweat gland tumours (“Ceruminomata”) of external auditory meatus. J Laryngol Otol 71(12):824–831
Prasad V, Shenoy VS, Rao RA et al (2015) Adenoid cystic carcinoma–a rare differential diagnosis for a mass in the external auditory canal. J Clin Diagn Res 9(1):MD01–MD02
Pulec JL (1977) Glandular tumors of the external auditory canal. Laryngoscope 87(10):1601–1612
Pulec JL, Parkhill EM, Devine KD (1963) Adenoid cystic carcinoma (Cylindroma) of the external auditory canal. Trans Am Acad Ophthalmol Otolaryngol 67:673–694
Ruhl DS, Tolisano AM, Swiss TP et al (2016) Ceruminous adenocarcinoma: an analysis of the surveillance epidemiology and end results (SEER) database. Am J Otolaryngol 37(2):70–73
Saunders TFC, Monksfield P (2014) A case of conservatively managed invasive ceruminoma and a review of the literature. Case Rep Otolaryngol 2014;2014:897540
Tanaka T, Saito R, Ishihara M et al (1984) Glandular tumors of the external auditory canal. Hiroshima J Med Sci 33(1):17–22
Thompson LDR (2017) Update from the 4th edition of the world health organization classification of head and neck tumours: tumours of the ear. Head Neck Pathol 11(1):78–87
Treasure T (2002) External auditory canal carcinoma involving the temporomandibular joint: two cases presenting as temporomandibular disorders. J Oral Maxillofac Surg 60(4):465–469
Turner HA, Carter H, Neptune WB (1971) Pulmonary metastases from ceruminous adenocarcinoma (cylindroma) of external auditory canal. Cancer 28(3):775–780
Tzagaroulakis A, Pasxalidis J, Papadimitriou N et al (2003) Recurrent ceruminous adenocarcinoma of the external auditory canal. ORL J Otorhinolaryngol Relat Spec 65(5):300–302
Virk JS, Kumar G, Khalil S (2014) Ceruminous adenocarcinoma of the ear. Ear Nose Throat J 93(4–5):146–148
Wetli CV, Pardo V, Millard M, Gerston K (1972) Tumors of ceruminous glands. Cancer 29(5):1169–1178
Yang C-Y, Shu M-T, Chen B-F (2010) Ceruminous adenocarcinoma. Otol Neurotol 31(6):1011–1012
Zhang Y, Liu H, Wu Q et al (2019) Predictors of distant metastasis and survival in adenoid cystic carcinoma of the external auditory canal. Otol Neurotol 40(10):e1006–e1011
Zhou Q, Zhang H, Liu H (2013) Adenoid cystic carcinoma of the external auditory canal associated with cholesteatoma in an 8-year-old girl. Int J Pediatr Otorhinolaryngol 77(1):150–152
Funding
No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by KR and DRC. The first draft of the manuscript was written by BW and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest. SEER contains publicly available, de-identified data making informed consent and institutional review board approval unnecessary.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. The study was exempt from institutional review board approval by The Ohio State University Human Research Protection Program.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wanner, B., Rismiller, K. & Carr, D.R. Treatment and survival outcomes of ceruminous carcinomas of the external auditory canal: a SEER database analysis and literature review. Arch Dermatol Res 314, 583–591 (2022). https://doi.org/10.1007/s00403-021-02257-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-021-02257-4