Abstract
Background
Malignant neoplasms of the external auditory canal (EAC) are rare. No consensus on management has emerged.
Objective
To determine possible risk factors influencing tumorgenesis and prognosis of EAC carcinoma.
Materials and methods
108 patients (87 men/21 women) with an average age of 74 ± 13.8 years were recruited from 2005 to 2019 at Department of Otorhinolaryngology, Head and Neck Surgery Heidelberg. The follow-up interval was 43.62 ± 55.39 months. Partial and (sub)total ablative otis, supplementary surgery (petrosectomy, parotidectomy, neck dissection, mastoidectomy) and adjuvant radio(chemo)therapy belonged to treatment options. TNM status was determined at time of diagnosis using the AJCC staging system.
Results
63.9% of patients underwent a total ablative otis. Tumor recurrence was seen in 24.1%. The 1-year survival rate was 87%, the 5-year survival rate was 52%, the mean overall survival (OS) was 3.82 ± 4.6 years. Male EAC carcinoma patients had a better OS (p < 0.001), PFS (p < 0.001) and DSS (p = 0.02) than females. T1 patients had a better OS (p = 0.01), PFS (p = 0.01) and DSS (p < 0.001) than T4 patients. Lymph node but not distant metastasis, tumor grading, perineural, venous and lymphatic invasion, histology, age and tumor localization influenced the OS in EAC carcinoma patients (p = 0.04). The more radical the ablative otis, the worse the OS (p = 0.002), PFS (p = 0.02) and DSS (p < 0.001). Radio(chemo)therapy did not improve the OS.
Conclusions
EAC carcinoma are difficult to treat and benefit from early diagnosis so that a radical combined treatment approach does not need to be used.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malignant neoplasms of the external auditory canal (EAC) are very rare, with an incidence of 1–6:1,000,000 per year [1,2,3]. They are responsible for approximately 0.2% of all head and neck cancers and for 0.2% of all ear diseases with an age peak between the fifth and seventh decades of life [4].
The most frequent tumor entity is the squamous cell carcinoma (SCC), followed by basal cell carcinoma (BCC), adenoid cystic carcinoma (ACC), ceruminous adenocarcinoma, and middle ear adenocarcinoma [2, 4,5,6,7]. Primary symptom of all EAC tumors is chronic otorrhea in 50–90% of cases. Simultaneous otitis externa or otitis media is very common. For this reason, an early diagnosis is difficult, and it leads to frequent misdiagnoses in 69% of cases [8, 9]. A biopsy is recommended in suspicious cases with EAC skin lesions [8].
Currently, there is no consensus on a standardized therapy management and an uniform staging system is lacking [5, 10, 11]. Depending on the tumor size, the therapy has evolved from partial removal of the auricle or soft tissue of the EAC to extensive surgical therapy including combined procedures such as radio- and/or chemotherapy [2, 5, 9, 12, 13].
Due to its low incidence, there is little data in the literature on EAC cancers with overall outdated studies and small sample sizes [1,2,3, 5, 11, 14,15,16,17,18,19,20,21].
Thus, the aim of this retrospective 14-year-long-term analysis is to determine possible risk factors influencing tumorgenesis and prognosis of 108 patients with EAC carcinoma by analyzing their impact on overall, disease-specific and progressive free survival after single or combined treatment.
Methods
Ethical considerations
The Ethics Committee of the Medical Faculty at the University of Heidelberg granted permission to conduct the study (Project No. S-338/2021) according to the Declaration of Helsinki on biomedical research involving human subjects. Informed consent was obtained from all patients. All data were pseudonymized before analysis.
Recruitment
From 2005 to 2019, 1345 patients with malignant neoplasms of the head and neck region were identified at Department of Otorhinolaryngology, Head and Neck Surgery, University Hospital of Heidelberg. Of these, 108 patients were diagnosed with external auditory canal carcinoma, originating from the auricle, the external auditory canal, the petrous bone, preauricular as well as retroauricular. 96.3% of EAC carcinoma patients underwent surgical therapy. The types of surgery were partial, subtotal and total ablative otis. Depending on tumor sizes, the surgical treatment expanded by parotidectomy, neck dissection (selective to radical), petrosectomy, mastoidectomy, radiotherapy and radiochemotherapy.
General demographic data (age, gender) as well as histology, tumor localization, tumor size (T), lymph node involvement (N), distant metastasis (M), grading (G), recurrence (R), lymph invasion (L), venous invasion (V), perineural invasion (Pn), type of surgery, adjuvant therapy were also collected.
Histological staging
Tumors, nodes and metastases (TNM) status was determined for all tumor entities at the time of diagnosis using the American Joint Committee on Cancer (AJCC) staging system for SCCs of the head and neck skin [22]. In the absence of a formal staging system [23], the histologically diagnosed basal cell carcinoma of the EAC could not be classified in TNM according to their tumor sizes.
Statistical analysis
Statistical analysis of the data was performed using R Version 4.2.2. with its libraries survival, ggsurvfit and condSURV. Demographic and clinicopathological patient characteristics were investigated with descriptive statistics. Continuous data were reported as mean values ± standard deviations and categorical data as absolute and relative frequencies. Missing values were included in the descriptive statistics.
Overall (OS) and progressive free survival (PFS) rates were plotted graphically using Kaplan–Meier curves. OS was defined as time from the date of cancer diagnosis to the date of death, PFS as the time from the date of cancer to the date of death from EAC cancer. DSS was calculated similar to OS with the exception that only tumor-related deaths were marked as an event.
Multivariate Cox proportional hazard models were used to explore associations between patient characteristics, tumor parameter, OS, PFS and DSS. Hazard ratios (HR) with 95% confidence intervals were calculated. The Cox proportional hazard model was used for multivariate analysis. P-values of < 0.05 were considered statistically significant.
The 1-year, 3-year and 5-year survival probability as well as the median OS, PFS and DSS were based on the Kaplan–Meier statistics and reported with their respective 95% confidence intervals.
To further test the impact of particular tumor parameters and therapeutic interventions, we performed log-rank tests. In those cases, we tested whether the number of observed events differed significantly to the number of expected events. The expected events were calculated that each group based on the parameters followed the same survival function. A p-value of less than 0.05 rejects this hypothesis, indicating that there are significantly more or less observed events in at least one group than it would have been expected. Hence, the assumption can then be supported that belonging to one of those groups would lead to a higher (or lower) survival rate.
Results
Patients cohort
108 patients (87 men and 21 women) with an average age of 74 ± 13.8 years (range: 9–94 years) were enrolled in this retrospective study. The average follow-up interval was 43.62 ± 55.39 months (range: 1–252 months). The malignant histopathologic diagnoses were predominantly squamous cell carcinoma (61.1%), followed by basal cell carcinoma (31.5%), adenoid cystic carcinoma (2.8%) and malignant melanoma (2.8%). The diagnoses were all histologically confirmed. The EAC carcinoma originally spread mainly from the auricle (69%) and the external auditory canal (15%). Figure 1 illustrates a spreading ear canal carcinoma, including the auricle (A), an EAC carcinoma growing locally on the floor of the external auditory canal (B), and an EAC carcinoma that completely fills the ear canal (C). The cancer extent of the primary tumor (T) was distributed among the patients as follows: T1 (n = 27), T2 (n = 8), T3 (n = 21), T4 (n = 12). Due to the absence of a formal staging system for basal cell carcinoma, the extent of the primary tumor was not classified in 40 EAC carcinoma patients. Regional lymph node involvement (N) was absent in 52 cases (N0) and present in 14 cases (N +). No distant metastases were detected in 69 cases, and M1 was diagnosed in two cases. 63.9% of patients underwent a total ablative otis with a postoperative surgical reconstruction (69.4%). For more than half of the patients with EAC carcinoma, no further operations, such as a middle ear intervention (3.7%), a neck dissection (31.5%), a parotidectomy (35.2%), a mastoidectomy (12%) or a petrosectomy (9.3%), were performed. Most patients had to be irradiated about 2.3 ± 1.7 months postoperatively. A tumor relapse was seen in 26 cases (24.1%). A comprehensive overview of all used patient’s data is listed in Table 1.
Exemplary presentation of a spreading external auditory canal carcinoma, including the auricle (A) Exemplary presentation of an EAC carcinoma, growing locally on the floor of the auditory canal (B) Exemplary representation of an EAC carcinoma completely filling the auditory canal, which is marked in green (C). The photos (A–B) were taken by one of the co-authors (P.F.)
Post-therapeutic survival
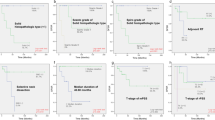
The 1-, 3-, and 5-year survival rates were determined using the Kaplan–Meier method. The values were 87% (80–94%, confidence interval (CI)) for 1-year survival, 60% (CI 50–72%) for 3-year survival, and 52% (CI 41–65%) for 5-year survival (Fig. 2). The mean overall survival (OS) was 3.82 ± 4.6 years, the mean progressive free survival (PFS) was 3.0 ± 3.9 years and the disease-specific survival (DSS) was 2.5 ± 3.1 years. The median OS was 5.8 years (CI 2.9–15), the median PFS was 2.8 years (CI 2.1–8.4) while the median DSS was 1.4 years (CI 1–2.8). Median years of survival were calculated based on the Kaplan–Meier statistics.
Sociodemographic influence on survival
There was a significant difference between men and women concerning the OS, PFS and DSS when using log-rank testing. Male EAC carcinoma patients had a better OS (p < 0.001), PFS (p < 0.001) and DSS (p = 0.02) than female patients, as shown in Fig. 3. There was no significant influence of age at therapy on OS and DSS detectable. However, Cox-Hazard models showed a significant effect of age on PFS.
Prognostic significance
In the present study, no significant impact of histology and tumor localization on OS, PFS or DSS could be calculated (p > 0.05). The cumulative survival of patients was worse with increasing tumor size (T1: p = 0.5; T1: p < 0.001; T3: p = 0.04; T4: p = 0.01). EAC carcinoma patients with T1 had a better OS (p = 0.01), PFS (p = 0.01) and DSS (p < 0.001) than patients with T4. Furthermore, a significant influence of tumor stage according to AJCC on OS (p = 0.003), PFS (p = 0.001) and DSS (p < 0.001) was seen. The lymph node involvement negatively influenced the OS (p = 0.04) and the DSS (p < 0.001) but not the PFS (p = 0.1). The propensity for distant metastasis (M) had a significant impact on DSS (p < 0.001) but not on OS (p = 0.09) and PFS (p = 0.3). The grading of tumor only affected the PFS (p = 0.01) while there was a significant influence of the lymphatic invasion on the PFS (p = 0.03) as well as on the DSS (p = 0.004). Perineural and venous invasion both did not affect the survival of patients with EAC carcinoma significantly.
Prognostic significance of therapy
Survival time appeared to be clinically decreased with combined therapies compared to surgery alone (OS: p < 0.001; PFS: p = 0.02; DSS: p < 0.001). According to the tumor spread, a radical procedure had to be carried out. The more radical the ablative otis, the worse the OS (p = 0.002), PFS (p = 0.02) and DSS (p < 0.001). An additional petrosectomy did not improve the OS (p = 0.9), the PFS (p = 0.5) and the DSS (p = 0.1) whereas the mastoidectomy, the parotidectomy and the neck dissection positively influenced the DSS (p < 0.05). The adjuvant radiotherapy only impacted the DSS (p = 0.003) but not the OS and PFS, while the radiochemotherapy had no significant influence on survival in patients with EAC carcinoma (p = 0.6).
Discussion
Carcinomas of the external auditory canal (EAC) are rare, and management remains challenging due to the lack of reliable clinical and pathological prognostic factors, and the markedly diverse surgical and oncological treatment modalities available [24]. Given such paucity, few epidemiological data are available and no consensus on management has emerged [8]. So, we performed here a long-term analysis of 108 EAC carcinoma patients after single or combined treatment to determine possible risk factors influencing tumorgenesis and prognosis.
Although no staging system for EAC carcinomas is currently recognized by either the Union for International Cancer Control or the American Joint Committee on Cancer, a comprehensive staging system developed by Arriaga et al. [25] and later modified by Moody et al. [26], namely the Pittsburgh Tumor Staging System, is most widely used [27, 28]. The Pittsburgh staging system is used for the SCC of the EAC, and occasionally for the ACC, although its suitability for the ACC is limited with respect to different tumor behaviors [29]. According to Wang et al., this provides ineffectiveness in diagnosis, treatment recommendation, and surgical planning because individual tumor entities exhibit different behaviors in terms of growth, locoregional metastasis, distant metastasis, and recurrence rate [29]. The system is based on tumor extent on computer tomography and histopathologic findings and has been validated using meta-analyses [28]. The staging system of the American Joint Committee on Cancer (AJCC) for squamous cell carcinoma of the skin of the head and neck is also used, since in addition to clinical radiological findings, histopathological parameters as well as nodal and perineural involvement also play a role [4]. In our study, the staging system of the AJCC was used and a significant influence of tumor stage according to AJCC on OS, PFS and DSS was seen, indicating that this tumor staging system has a legitimate application at carcinoma of EAC.
Efforts have been made to identify prognostic factors that can improve treatment protocols. Several disease-related factors such as tumor stage, a poorly differentiated cell type, neck lymph node involvement, and facial paralysis indicate poor prognosis [3, 5, 30]. We could show that lymph node metastasis but not distant metastasis, tumor grading, perineural, venous and lymphatic invasion, histology, age and tumor localization significantly influenced the OS in EAC carcinoma patients. Following the literature, the survival rates of patients with SCCs of the EAC who undergo surgery at early stages are reportedly favorable, highlighting the importance of clinical suspicion and early diagnosis [3, 5, 24,25,26,27, 30,31,32]. In our study, the malignant histopathologic diagnoses were also predominantly squamous cell carcinoma, followed by basal cell carcinoma and adenoid cystic carcinoma. The cumulative survival of our EAC carcinoma patients was worse with increasing tumor size, indicating that EAC carcinoma patients with T1 had a significant better OS, PFS and DSS than those with T4. Generally, SCCs of the EAC are associated with poorer prognoses than other pathologies [24]. As second relevant finding here, male EAC carcinoma patients had a better OS, PFS and DSS than female patients. To date, there have been no studies that have identified gender as a prognostic factor. However, we have to admit that there was an unequal distribution in favor of the male gender in our study (87 men vs. 21 women).
The complexity of the anatomy and the relationship between the tumor with surrounding tissues within a limited space, render it difficult to attain safe resection margins [31]. Essig et al. reported a DFS rate of 81% at 2 years in patients with clear margins, in contrast to a DFS rate of 45% in patients with positive margins [32]. Moody et al. also reported that positive histological margins were associated with reduced survival at 2 years (32%) compared to that of patients with clear margins (75%) [26]. In our study, tumor recurrence was seen in 24.1%. The 1-year survival rate was 87% and the 5-year survival rate was 52%. Thus, the surgeon should consider wide en bloc resection to create oncologically safe margins. But so far, there is no consensus on a standardized therapy management in patients with EAC carcinoma. Various methods ranging from minimally invasive procedures to extensive surgical therapies, including combined procedures such as radio- and/or chemotherapy, could be found in the literature [13, 21]. In our study, the types of surgery varied from partial, subtotal, and total ablative otis to additional extended surgical therapies, such as neck dissection, mastoidectomy, parotidectomy, petrosectomy, or other middle ear surgeries. 18 patients received radiotherapy in addition to surgical therapy, in nine cases, combined radio-chemotherapy was given. In most studies, combined therapy is described as the standard of care [28, 33,34,35]. It was further reported that patients with early tumor stages of EAC carcinoma benefited from a less aggressive surgical approach and that radiotherapy and radiochemotherapy, respectively, was recommended at later tumor stages for positive tumor margins [17, 36, 37]. We noticed here that the more radical the ablative otis, the worse the OS, the PFS and the DSS. Furthermore, an adjuvant radio(chemo)therapy did not improve the OS of our included EAC carcinoma patients. Nakagawa et al. underlined our findings who did not detect a positive significant impact of radiochemotherapy on OS [38]. Additionally, Takenaka et al. described that preoperative radiochemotherapy could improve tumor survival by analyzing 725 EAC tumor patients in a meta-analysis. However, if the prognosis was poor, postoperative RCT had no positive impact on survival [39]. Thus, it is questionable whether a multimodal concept which is frequently applied in advanced tumor stages should be made as a general recommendation. What is important is an early diagnosis and a correspondingly least radical surgical therapy approach. Personalized medicine, which is precisely tailored to the patient, would be the therapy of choice in patients with EAC carcinoma. Extended surgical treatments should be discussed individually, depending on tumor location and extension, because we showed here that the mastoidectomy, the parotidectomy and the neck dissection positively influenced the DSS in patients with EAC carcinoma.
The study has several limitations, one of which is the rarity of this tumor entity and thus the limited number of patients as well as the retrospective nature, which may have led to an underestimation or an overestimation of treatment outcome, preventing generalizable population-based conclusions. Another limitation was the unequal gender ratio, which is in line with further oncological studies [3, 9, 40]. In addition, there were many unknown T4 stages, making it difficult to statistically validate and compare clinical results. Complementary operations were only performed in 3.7 until 35% of cases, so that the therapy effect can only be inadequately assessed. The major limitation of our study was the fact that Nam et al. 2018 already found in his retrospective 10-year study that advanced T stage and advanced overall stage in 26 patients with SCC of the EAC were associated with lower survival after surgical treatment using the modified University of Pittsburgh staging system, underscoring the importance of clinical vigilance and early detection [24]. Despite the same message of a necessary early tumor detection, our study has decisive advantages. The strengths of this 14-year long-term study relate to the extensive clinical data collection of 108 EAC carcinoma patients, which implies a large power with strong significance. Of course, an even larger number of patients with EAC carcinoma would have been desirable, but considering the rare entity and our location advantage through the cooperation with the National Tumor Center in Germany, this number of patients is actually quite remarkable, especially compared to most studies on EAC carcinomas. Our 14-year study continues to benefit from the description of different histologic EAC carcinoma types, treatment diversity, and the use of the AJCC's statistically relevant staging system for OS, PFS, and DSS. Additional studies are needed to identify surrogate biomarkers that could help guide clinical decisions about treatment options in EAC carcinoma. The second step is to find out what subjectively affects the patient's quality of life most due to an EAC carcinoma and its therapeutic treatment, to be able to meet the requirements of high-quality outcome research.
Conclusion
In conclusion, this study shows that EAC carcinoma are difficult to treat and benefit from early diagnosis so that an overly radical combined treatment approach does not need to be used. Personalized medicine would be the therapy of choice in patients with EAC carcinoma.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Carvalho CP, Barcellos AN, Teixeira DC, de Oliveira SJ, da Silva NR (2008) Adenoid cystic carcinoma of the external auditory canal. Braz J Otorhinolaryngol 74(5):794–796. https://doi.org/10.1016/S1808-8694(15)31394-X
Chang CH, Shu MT, Lee JC, Leu YS, Chen YC, Lee KS (2009) Treatments and outcomes of malignant tumors of external auditory canal. Am J Otolaryngol 30(1):44–48. https://doi.org/10.1016/j.amjoto.2008.02.007
Lobo D, Llorente JL, Suarez C (2008) Squamous cell carcinoma of the external auditory canal. Skull Base 18(3):167–172. https://doi.org/10.1055/s-2007-994290
Allanson BM, Low T-H, Clark JR, Gupta R (2018) Squamous cell carcinoma of the external auditory canal and temporal bone: an update. Head Neck Pathol 12(3):407–418. https://doi.org/10.1007/s12105-018-0908-4
Gandhi AK, Roy S, Biswas A, Raza MW, Saxena T, Bhasker S, Sharma A, Thakar A, Mohanti BK (2016) Treatment of squamous cell carcinoma of external auditory canal: a tertiary cancer centre experience. Auris Nasus Larynx 43(1):45–49. https://doi.org/10.1016/j.anl.2015.06.005
Lobo D, Llorente JL, Suárez C (2008) Squamous cell carcinoma of the external auditory canal. Skull Base 18(3):167–172. https://doi.org/10.1055/s-2007-994290
Morita S, Mizumachi T, Nakamaru Y, Sakashita T, Kano S, Hoshino K, Fukuda A, Fujiwara K, Homma A (2018) Comparison of the University of Pittsburgh staging system and the eighth edition of the American Joint Committee on Cancer TNM classification for the prognostic evaluation of external auditory canal cancer. Int J Clin Oncol 23 (6):1029–1037. https://doi.org/10.1007/s10147-018-1314-3
Zhang T, Dai C, Wang Z (2013) The misdiagnosis of external auditory canal carcinoma. Eur Arch Otorhinolaryngol 270(5):1607–1613. https://doi.org/10.1007/s00405-012-2159-4
Park JM, Kong JS, Chang KH, Jun BC, Jeon EJ, Park SY, Park SN, Park KH (2018) The clinical characteristics and surgical outcomes of carcinoma of the external auditory canal: a multicenter study. J Int Adv Otol 14(2):278–284. https://doi.org/10.5152/iao.2018.4952
Prasad S, Janecka IP (1994) Efficacy of surgical treatments for squamous cell carcinoma of the temporal bone: a literature review. Otolaryngol Head Neck Surg 110(3):270–280. https://doi.org/10.1177/019459989411000303
Wanner B, Rismiller K, Carr DR (2022) Treatment and survival outcomes of ceruminous carcinomas of the external auditory canal: a SEER database analysis and literature review. Arch Dermatol Res 314(6):583–591. https://doi.org/10.1007/s00403-021-02257-4
Mazzoni A, Danesi G, Zanoletti E (2014) Primary squamous cell carcinoma of the external auditory canal: surgical treatment and long-term outcomes. Acta otorhinolaryngologica Italica: organo ufficiale della Societa italiana di otorinolaringologia e chirurgia cervico-facciale 34(2):129–137
Schwager K, Pfreundner L Fau - Hoppe F, Hoppe F Fau - Baier G, Baier G Fau - Willner J, Willner J Fau - Baier K, Baier K [Carcinoma of the external ear canal and middle ear as interdisciplinary challenge for ear surgery and radiotherapy] (Das Karzinom des äusseren Gehörgangs und des Mittelohres als interdisziplinäre Herausforderung für Otochirurgie und Strahlentherapie.). (0935–8943 (Print))
Ostrowski VB, Wiet RJ (1996) Pathologic conditions of the external ear and auditory canal. Postgrad Med 100 (3):223–228, 233–227. https://doi.org/10.3810/pgm.1996.09.79
Visnyei K, Gill R, Azizi E, Culliney B (2013) Squamous cell carcinoma of the external auditory canal: a case report and review of the literature. Oncol Lett 5(5):1587–1590. https://doi.org/10.3892/ol.2013.1241
Smit CF, de Boer N, Lissenberg-Witte BI, Merkus P, Hensen EF, Leemans CR (2021) Surgical treatment for squamous cell carcinoma of the temporal bone: predictors of survival. Acta otorhinolaryngologica Italica: organo ufficiale della Societa italiana di otorinolaringologia e chirurgia cervico-facciale 41(4):308–316. https://doi.org/10.14639/0392-100X-N1074
Shinomiya H, Uehara N, Teshima M, Kakigi A, Otsuki N, Nibu KI (2019) Clinical management for T1 and T2 external auditory canal cancer. Auris Nasus Larynx 46(5):785–789. https://doi.org/10.1016/j.anl.2019.02.004
Prabhu R, Hinerman RW, Indelicato DJ, Morris CG, Werning JW, Vaysberg M, Amdur RJ, Kirwan J, Mendenhall WM (2009) Squamous cell carcinoma of the external auditory canal: long-term clinical outcomes using surgery and external-beam radiotherapy. Am J Clin Oncol 32(4):401–404. https://doi.org/10.1097/COC.0b013e31818f2d48
Fleiner F, Jumah M, Göktas O (2009) Cancer of the external auditory canal-diagnostic and treatment. Indian J Otolaryngol Head Neck Surg 61(4):270–274. https://doi.org/10.1007/s12070-009-0081-x
Madsen AR, Gundgaard MG, Hoff CM, Maare C, Holmboe P, Knap M, Thomsen LL, Buchwald C, Hansen HS, Bretlau P, Grau C (2008) Cancer of the external auditory canal and middle ear in Denmark from 1992 to 2001. Head Neck 30(10):1332–1338. https://doi.org/10.1002/hed.20877
Correia-Rodrigues PA-O, Ramalho S, Montalvão P, Magalhães M External auditory canal carcinoma: clinical characteristics and long-term treatment outcomes. (1434–4726 (Electronic))
Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK, Meyer L, Gress DM, Byrd DR, Winchester DP (2017) The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more "personalized" approach to cancer staging. CA Cancer J Clin 67 (2):93–99. https://doi.org/10.3322/caac.21388
Work G, Invited R, Kim JYS, Kozlow JH, Mittal B, Moyer J, Olencki T, Rodgers P (2018) Guidelines of care for the management of basal cell carcinoma. J Am Acad Dermatol 78(3):540–559. https://doi.org/10.1016/j.jaad.2017.10.006
Nam GS, Moon IS, Kim JH, Kim SH, Choi JY, Son EJ (2018) Prognostic factors affecting surgical outcomes in squamous cell carcinoma of external auditory canal. Clin Exp Otorhinolaryngol 11(4):259–266. https://doi.org/10.21053/ceo.2017.01340
Arriaga M, Curtin H, Takahashi H, Hirsch BE, Kamerer DB (1990) Staging proposal for external auditory meatus carcinoma based on preoperative clinical examination and computed tomography findings. Ann Otol Rhinol Laryngol 99(9 Pt 1):714–721. https://doi.org/10.1177/000348949009900909
Moody SA, Hirsch BE, Myers EN (2000) Squamous cell carcinoma of the external auditory canal: an evaluation of a staging system. Am J Otol 21(4):582–588
Lassig AA, Spector ME, Soliman S, El-Kashlan HK (2013) Squamous cell carcinoma involving the temporal bone: lateral temporal bone resection as primary intervention. Otol Neurotol 34(1):141–150. https://doi.org/10.1097/MAO.0b013e318278bf38
Ihler F, Koopmann M, Weiss BG, Droge LH, Durisin M, Christiansen H, Weiss D, Canis M, Wolff HA (2015) Surgical margins and oncologic results after carcinoma of the external auditory canal. Laryngoscope 125(9):2107–2112. https://doi.org/10.1002/lary.25381
Wang Z, Zheng M, Xia S (2016) The contribution of CT and MRI in staging, treatment planning and prognosis prediction of malignant tumors of external auditory canal. Clin Imaging 40(6):1262–1268. https://doi.org/10.1016/j.clinimag.2016.08.020
Leong SC, Youssef A, Lesser TH (2013) Squamous cell carcinoma of the temporal bone: outcomes of radical surgery and postoperative radiotherapy. Laryngoscope 123(10):2442–2448. https://doi.org/10.1002/lary.24063
Mazzoni A, Danesi G, Zanoletti E (2014) Primary squamous cell carcinoma of the external auditory canal: surgical treatment and long-term outcomes. Acta Otorhinolaryngol Ital 34(2):129–137
Essig GF, Kitipornchai L, Adams F, Zarate D, Gandhi M, Porceddu S, Panizza B (2013) Lateral temporal bone resection in advanced cutaneous squamous cell carcinoma: report of 35 patients. J Neurol Surg B Skull Base 74(1):54–59. https://doi.org/10.1055/s-0032-1331021
Breen JT, Roberts DB, Gidley PW (2018) Basal cell carcinoma of the temporal bone and external auditory canal. Laryngoscope 128(6):1425–1430. https://doi.org/10.1002/lary.26785
Hahn SS, Kim JA, Goodchild N, Constable WC (1983) Carcinoma of the middle ear and external auditory canal. Int J Radiat Oncol Biol Phys 9(7):1003–1007. https://doi.org/10.1016/0360-3016(83)90388-7
Oya R, Takenaka Y, Takemura K, Ashida N, Shimizu K, Kitamura T, Yamamoto Y, Uno A (2017) Surgery with or without postoperative radiation therapy for early-stage external auditory canal squamous cell carcinoma: a meta-analysis. Otol Neurotol 38(9):1333–1338. https://doi.org/10.1097/MAO.0000000000001533
Shih L, Crabtree JA (1990) Carcinoma of the external auditory canal: an update. Laryngoscope 100(11):1215–1218. https://doi.org/10.1288/00005537-199011000-00016
Nyrop M, Grontved A (2002) Cancer of the external auditory canal. Arch Otolaryngol Head Neck Surg 128(7):834–837. https://doi.org/10.1001/archotol.128.7.834
Nakagawa T, Kumamoto Y, Natori Y, Shiratsuchi H, Toh S, Kakazu Y, Shibata S, Nakashima T, Komune S (2006) Squamous cell carcinoma of the external auditory canal and middle ear: an operation combined with preoperative chemoradiotherapy and a free surgical margin. Otol Neurotol 27 (2):242–248; discussion 249. https://doi.org/10.1097/01.mao.0000190463.88873.3d
Takenaka Y, Cho H, Nakahara S, Yamamoto Y, Yasui T, Inohara H (2015) Chemoradiation therapy for squamous cell carcinoma of the external auditory canal: a meta-analysis. Head Neck 37(7):1073–1080. https://doi.org/10.1002/hed.23698
Boamah H, Knight G, Taylor J, Palka K, Ballard B (2011) Squamous cell carcinoma of the external auditory canal: a case report. Case Rep Otolaryngol 2011:615210. https://doi.org/10.1155/2011/615210
Funding
No external/additional funding was received for this study. No financial support or funding.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the study. VL: participated in data acquisition and analysis, interpreted the data, and drafted the manuscript. NW: designed and coordinated the study. MS: participated in data interpretation and statistical analysis. PF: interpreted data and revised the manuscript. KZ: designed and coordinated the study and revised the manuscript. MP: designed and coordinated the study, participated in data acquisition and analysis, and critically revised the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
The Ethics Committee of the Medical Faculty at the University of Heidelberg granted permission to conduct the study (Project No. S-338/2021).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lohnherr, V., Wurzrainer, N., Sand, M. et al. Long-term analysis of prognostic risk factors impacting surgical outcomes in patients with external auditory canal carcinoma. Eur Arch Otorhinolaryngol 280, 2965–2974 (2023). https://doi.org/10.1007/s00405-023-07890-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-07890-5