Abstract
Keloid scars are common benign fibroproliferative reticular dermal lesions with unknown etiology and ill-defined management with high rate of recurrence post surgery. The progression of keloids is characterized by increased deposition of extracellular matrix proteins, invasion into the surrounding healthy skin and inflammation. Fibroblasts are considered to be the key cellular mediators of fibrogenesis in keloid scars. Fibroblast activation protein alpha (FAP-α) and dipeptidyl peptidase IV (DPPIV) are proteases located at the plasma membrane promoting cell invasiveness and tumor growth and have been previously associated with keloid scars. Therefore, in this study we analyzed in further detail the expression of FAP-α in keloid fibroblasts compared to control skin fibroblasts. Dermal fibroblasts were obtained from punch-biopsies from the active margin of four keloids and four control skin samples. Flow cytometry was used to analyze FAP-α expression and the CytoSelect® 24-Well Collagen I Cell Invasion Assay was applied to study fibroblast invasion. Secretion of extracellular matrix (ECM) proteins was investigated by multiplexed particle-based flow cytometric assay and enzyme-linked immunosorbent assay. We found an increased expression of FAP-α in keloid fibroblasts compared to control skin fibroblasts (p < 0.001). Inhibition of FAP-α/DPPIV activity using the irreversible inhibitor H2N-Gly-Pro diphenylphosphonate reduced the increased invasiveness of keloid fibroblasts (p < 0.001) indicating that keloid invasion may be partly FAP-α/DPPIV mediated. FAP-α/DPPIV inhibition had no effect, (a) on the synthesis of the ECM proteins procollagen type I C-terminal peptide and fibronectin, (b) on the production of fibroblast growth factor or vascular endothelial growth factor, (c) on the expression of the proinflammatory cytokines interleukin-6 (IL-6), interleukin 8 (IL-8) or monocyte chemotactic protein-1. These results suggest a potential role for FAP-α and DPPIV in the invasive behavior of keloids. FAP-α and DPPIV may increase the invasive capacity of keloid fibroblasts rather than by modulating inflammation or ECM production. Since FAP-α expression is restricted to reactive fibroblasts in wound healing and normal adult tissues are generally FAP-α negative, inhibiting FAP-α/DPPIV activity may be a novel treatment option to prevent keloid progression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Keloids are benign dermal skin tumors unique to humans [38]. They represent a form of abnormal wound healing process which is commonly found in genetically susceptible individuals [20, 23, 33]. Keloids occur at areas of cutaneous injury and grow continuously beyond the original margins of the wound and invade the surrounding healthy skin [22]. Even the spontaneous development of keloids has been discussed but may be the result of a minor, overlooked trauma [27]. Keloids are characterized by the increased production of extracellular matrix proteins including collagen I and fibronectin [13, 32, 38] and by inflammatory processes driven by cytokines such as interleukin-6 [6]. Keloids are more common in darker pigmented ethnicities with up to 15% of the population at risk [38]. The development of keloids leads to enormous clinical problems for the patients [19]. Patients with keloids suffer from itching, pain, restriction of mobility and experience a dramatic decrease of their quality of life [3]. Numerous treatment options have been described [10, 11, 32] but there is still no single effective therapeutic regimen for the treatment of keloids, and keloids have a high rate of recurrence post surgery [4].
The invasive growth of keloids into the surrounding healthy skin requires the breakdown of extracellular matrix (ECM) at the leading edge of keloids [12]. Factors including matrix metalloproteinases (MMPs) [12] or insulin-like growth factor-1 receptor (IGF-1R) [25] have been described to be involved in the invasive character of keloid fibroblasts but the exact mechanisms need to be elucidated. Fibroblast activation protein-alpha (FAP-α), a member of the group II integral serine proteases [24], may play an important role in the invasive properties of keloids. The expression of FAP-α on the cell membrane is a common attribute of reactive stromal fibroblasts [30]. Immunohistological studies have demonstrated that FAP-α, beside its expression in reactive stroma responding to epithelial cancers, is also found in fetal mesenchymal tissues and during wound healing [5, 29]. This led to the conclusion that FAP-α expression is correlated with specialized fibroblast functions in wound healing and since normal adult tissues are generally FAP-α negative [24] FAP-α might be an important target for keloid treatment [15].
FAP-α has been shown to associate with another serine protease, dipeptidylpeptidase IV (DPPIV), on the membrane of fibroblasts [7]. A recent study described that inhibitors of DPPIV-like activity suppress expression of TGFβ-1, fibronectin as well as collagen I which are major components in the pathogenesis of keloids [37]. Therefore, in the present study we analyzed the expression of FAP-α in human keloid fibroblasts compared to control skin fibroblasts. Furthermore, FAP-α and DPPIV activity were inhibited using a well-described irreversible inhibitor H2N-Gly-Pro diphenylphosphonate [8] to study the effect on the invasive capacity of keloid and control skin fibroblasts.
As the development and growth of keloids is characterized by inflammation, increased biosynthesis of growth factors, and deposition of ECM proteins [1, 2, 39] we tested the hypothesis whether FAP-α/DPPIV inhibition can influence the expression of pro-inflammatory cytokines [interleukin-6 (IL-6), interleukin-8 (IL-8) and monocyte chemotactic protein-1 (MCP-1)], the expression of extracellular matrix proteins (procollagen type I C-terminal peptide and fibronectin) and growth factors [fibroblast growth factor (FGF) and vascular endothelial growth factor (VEGF)].
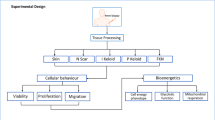
Materials and methods
Patients
All experiments were performed according to the ethical principles of the Helsinki declaration and approved by the Ethical Committee at Linköping University, Sweden. Primary human skin fibroblasts were obtained as previously described [31]. 5 mm punch biopsies were taken from the upper back of four Caucasian donors (25–38 years of age) and from four Caucasian patients (23–37 years of age) with keloids on corresponding anatomical sites. The punch biopsies were taken from the active margin of the keloids. A keloid scar was defined as a dermal tumor that spread beyond the margin of the original wound, continued to grow over time, did not regress spontaneously and had been present for at least a minimum period of 1 year. Keloids were not treated before biopsies were taken.
Cell cultures and conditions
Primary skin fibroblast cultures were established in HEPES-buffered RPMI 1640 (GIBCO, Invitrogen, Paisley, UK) supplemented with 10% fetal calf serum (FCS) (PAA, Pasching, Austria), 10 mM L-glutamine (Invitrogen), 100 U/ml penicillin, and 0.1 mg/ml streptomycin (Sigma–Aldrich). Cell cultures were maintained at 37°C in a humidified incubator with 5% CO2. Cells from passage 2–7 were used and not cultured for more than 3 weeks. Serum-free media was used 24 h prior to all experiments. Keloid and control fibroblasts showed a viability >95% as determined by trypan-blue (Sigma–Aldrich, Deisenhofen, Germany) exclusion.
FAP-α inhibition
The cell permeable inhibitor H2N-Gly-Pro diphenylphosphonate (Gly-ProP(OPh)2, 100 μM, 24 h prior to experiment, stock in DMSO [8]) was used to block FAP-α and DPPIV activity. Controls for DMSO effects were analyzed and no interference with the experiments was noted.
Multiplexed particle-based flow cytometric assay
The Fluorokine MultiAnalyte Profiling assay (R&D Systems, Minneapolis, USA) was performed as previously described [40]. Cytokines analyzed in duplicate included IL-6 and IL-8, FGF, VEGF, and MCP-1. In brief standard curves for each cytokine were generated by using the reference cytokine concentrations supplied by the manufacturer. 50 μl of standard or sample was added per well and incubated for 3 h at room temperature. The microplate wells were washed three times using a vacuum manifold. 50 μl diluted Biotin Antibody Cocktail was added to each well and incubated for 1 h at room temperature. After washing 50 μl Streptavidin-PE were added to each well and incubated for 30 min at room temperature. Hereafter, the microparticles were resuspended by adding 100 μl wash buffer to each well and after 2 min incubation raw data (mean fluorescent intensity) were analyzed using a Luminex analyzer.
Cell invasion assay
Cells were starved in serum-free media 24 h prior to assay to allow expression of free receptors. CytoSelect® 24-Well Collagen I Cell Invasion Assay was used (Cell Biolabs Inc, San Diego,CA, USA). Cells were placed at 5 × 105 cells/well on top of the gel matrix inside the upper chamber with or without inhibitor [the cell permeable FAP-α/DPPIV inhibitor Gly-ProP(OPh)2] and allowed for 24 h to invade toward 10% fetal bovine serum (FBS) through the matrix and adhere to the bottom membrane of the insert. Non-invasive cells were removed from the upper chamber. Invaded cells on the bottom of the invasion membrane were extracted and stained with cell stain solution where after the cells were quantified at OD 560 nm using a colorimetric plate reader.
Enzyme-linked immunosorbent assay (ELISA)
The amounts of fibronectin and procollagen type I C-terminal peptide used as a marker for procollagen I secretion were determined in cell culture supernatants using commercially available ELISA kits (Chemicon, Millipore, Temecula, CA, USA and Quidel, San Diego, USA). Keloid and control fibroblasts were seeded into 12-well tissue culture plates at a density of 1 × 104 cells/well. After 24 h the medium was exchanged by serum free medium. Culture supernatants were harvested after 24, 48, and 72 h then centrifuged, and frozen at −70°C until use. The number of viable fibroblasts in each well at the different time points was analyzed and ELISA results were normalized to 1 × 104 cells. Fibronectin concentration was determined by a microplate reader at 450 nm and procollagen type I C-terminal peptide at 405 nm.
Flow cytometry
Fibroblasts were incubated 30 min at room temperature with 1 μg monoclonal FAP-α antibody (Santa Cruz, Heidelberg, Germany), rinsed twice and incubated with secondary goat anti-mouse IgG-FITC antibody (R&D Systems, Minneapolis, MN, USA) for 30 min. The cells were washed twice and resuspended in PBS with 1% FCS prior to analysis. FAP-α expression was determined by FACScan (Becton–Dickinson, Cockeysville, MD, USA) and data analysis was performed by FACSQuest software (BD). From each sample 2 × 104 cells were analyzed. Fibroblasts incubated with mouse IgG-FITC (Santa Cruz) were used as isotype control.
Statistics
Each experiment was repeated three times. Results are expressed as means ± standard deviation. Differences among groups were analyzed using the one-way analysis of variance (ANOVA) with the Tukey’s post hoc multiple comparison as a post test. p values <0.05 were considered significant.
Results
To analyze the expression of FAP-α primary human fibroblasts from control skin and keloids were studied. Flow cytometry results showed a significant increased expression of FAP-α in keloid fibroblasts (p < 0.001) compared to control skin fibroblasts (Fig. 1a, b).
To determine the effect of FAP-α/DPPIV inhibition on the invasive capacity of keloid and control fibroblasts a collagen I invasion assay was performed. Keloid fibroblasts revealed significant increased invasiveness compared to control skin fibroblasts (p < 0.001) and supplementation of Gly-ProP(OPh)2 significantly reduced the number of invaded keloid fibroblasts (p < 0.001) (Fig. 2).
Inhibition of FAP-α/DPPIV activity decrease the invasive capacity of keloid fibroblasts. The invasion of keloid and control fibroblasts with (+) or without (−) addition of the FAP-α/DPPIV inhibitor Gly-ProP(OPh)2 was analyzed by CytoSelect® Collagen I Cell Invasion Assay. Invasive cells were quantified at OD 560 nm (n = 3, ***p < 0.001)
We studied the consequence of FAP-α/DPPIV inhibition on the expression of procollagen type I C-terminal peptide and fibronectin. Our results showed no effect of FAP-α/DPPIV inhibition on the production of procollagen type I C-terminal peptide and fibronectin (Fig. 3a, b).
To investigate whether FAP-α/DPPIV inhibition can influence the expression of the inflammatory cytokines IL-6, IL-8 and MCP-1 or the production of the growth factors FGF and VEGF a multiplexed particle-based flow cytometric assay of cell culture supernatants from keloid fibroblasts and control skin fibroblasts was performed. Keloid fibroblasts produced more IL-8 after 72 h and VEGF after 24 h compared to control fibroblasts (Fig. 4) but no effect of FAP-α/DPPIV inhibition on the expression of these factors (data not shown for IL-6, FGF, MCP-1) were seen.
Discussion
The results obtained in this study showed for the first time that FAP-α protein expression is increased in keloid fibroblasts compared to normal skin fibroblasts. These results are in line with our previous finding of increased FAP-α mRNA expression in keloid fibroblasts [31]. Given that FAP-α plays an important role in degrading ECM thereby, facilitating cell invasion [26] our results suggest that up-regulation of FAP-α may support the invasive growth of keloids which is a typical clinical sign at their active margin. This hypothesis is supported by our findings showing increased invasion of keloid fibroblasts compared to control skin fibroblasts. Keloid fibroblast invasion may be partly FAP-α/DPPIV mediated as inhibition of FAP-α/DPPIV significantly decreased their invasive capacity. Thus, blocking FAP-α/DPPIV may be a promising treatment option especially as FAP-α is selectively expressed in wound healing fibroblasts [24]. Monsky et al. [21] showed that FAP-α expression is associated with increased invasion of melanoma suggesting FAP-α as a potential candidate for anti-metastatic therapies. This hypothesis is underlined by a recent study showing that melanoma growth was inhibited in tumor-bearing mice vaccinated against FAP-α [15] offering the possibility to vaccinate patients known to be more susceptible to develop keloid disease.
The protease DPPIV is closely associated to FAP-α on the membrane of fibroblasts [7] and they share common biological functions [9]. Thielitz et al. [37] showed that inhibitors of DPPIV-like activity suppress the expression of fibronectin and procollagen type I C-terminal peptide. Hence, we analyzed whether FAP-α inhibition might have the same effect. The FAP-α inhibitor used in our study is not specific for FAP-α, it inhibits DPPIV activity as well [8], Interestingly, our inhibitor had no effect regarding the in vitro production of procollagen type I C-terminal peptide and fibronectin. It is difficult to compare the findings of these studies. It is unclear to what extend FAP-α and DPPIV activity were blocked by the inhibitors used and the keloid fibroblast populations analyzed might be different as Thielitz et al. did not point out from what part of the keloid fibroblasts were taken.
In future studies, shorter time points (6 and 12 h) have to be analyzed to exclude earlier FAP-α/DPPIV inhibition effects on procollagen type I C-terminal peptide and fibronectin production since there maybe a time-related dose effect which needs to be further explored. This might explain why we did not find significantly increased levels of procollagen type I C-terminal peptide and fibronectin in the cell culture supernatants of keloid fibroblasts compared to control fibroblasts, even though they were found to be generally increased in keloids. Furthermore, keloid fibroblasts utilized in this study were taken from the active margin of keloids where invasive growth was present. Previous studies describing increased production of collagen and fibronectin did not differentiate between the dormant center of the keloid compared to its active margin. It is possible that increased secretion of ECM proteins such as collagen and fibronectin are located at the center of the lesion and not at the active margin since there are biological differences described in different keloid regions [18]. This remains to be further elucidated as there is considerable heterogeneity within these lesions compounded by their age, anatomical site, and gender influences [36].
The growth factors VEGF and FGF, the inflammatory cytokines IL-6, IL-8 and MCP-1 are involved in keloid development and modulation of their expression may prove to be valuable in the long-term treatment of keloids [6, 16, 17, 34, 35, 41]. Therefore, we tested whether FAP-α/DPPIV inhibition might be useful for this purpose, especially as the inhibition of DPPIV has shown to have significant effect on inflammation and cytokine production [28]. In line with the results found for procollagen type I C-terminal peptide and fibronectin FAP-α/DPPIV inhibition showed no effect on the expression of the growth factors VEGF and FGF or on the production of the inflammatory cytokines IL-6, IL-8, and MCP-1.
We showed significant increased expression of VEGF at 24 h and IL-8 at 72 h in keloid fibroblasts which is according with the previous reports [14, 17] but we could not confirm increased expression of IL-6 and MCP-1 as suggested by Ghazizadeh and Liao et al. [6, 16]. It is difficult to compare in vitro results from different studies on keloids as keloids are located at different body regions with different gene expression patterns, the age and reason for keloids (burn, trauma, spontaneously) differ, the skin color of patients may be important and cell culture conditions may influence expression of the analyzed cytokines and growth factors. Future studies would include immunohistochemistry analysis of FAP-α in vivo comparing the center and the active margin of keloids, and in particular the specific inhibition of FAP-α protease activity can also be investigated in vivo using an animal model such as a nude mouse harboring keloid tissue.
In conclusion, this preliminary study, for the first time has shown an increased expression of FAP-α and a FAP-α/DPPIV mediated increased invasive capacity of keloid fibroblasts compared to control skin fibroblasts suggesting a potentially novel mechanism for keloid progression and invasiveness.
References
Abergel RP, Pizzurro D, Meeker CA, Lask G, Matsuoka LY, Minor RR, Chu ML, Uitto J (1985) Biochemical composition of the connective tissue in keloids and analysis of collagen metabolism in keloid fibroblast cultures. J Invest Dermatol 84:384–390
Babu M, Diegelmann R, Oliver N (1989) Fibronectin is overproduced by keloid fibroblasts during abnormal wound healing. Mol Cell Biol 9:1642–1650
Bock O, Schmid-Ott G, Malewski P, Mrowietz U (2006) Quality of life of patients with keloid and hypertrophic scarring. Arch Dermatol Res 297:433–438
Durani P, Bayat A (2008) Levels of evidence for the treatment of keloid disease. J Plast Reconstr Aesthet Surg 61:4–17
Garin-Chesa P, Old LJ, Rettig WJ (1990) Cell surface glycoprotein of reactive stromal fibroblasts as a potential antibody target in human epithelial cancers. Proc Natl Acad Sci USA 87:7235–7239
Ghazizadeh M, Tosa M, Shimizu H, Hyakusoku H, Kawanami O (2007) Functional implications of the IL-6 signaling pathway in keloid pathogenesis. J Invest Dermatol 127:98–105
Ghersi G, Zhao Q, Salamone M, Yeh Y, Zucker S, Chen WT (2006) The protease complex consisting of dipeptidyl peptidase IV and seprase plays a role in the migration and invasion of human endothelial cells in collagenous matrices. Cancer Res 66:4652–4661
Gilmore BF, Lynas JF, Scott CJ, McGoohan C, Martin L, Walker B (2006) Dipeptide proline diphenyl phosphonates are potent, irreversible inhibitors of seprase (FAPalpha). Biochem Biophys Res Commun 346:436–446
Gorrell MD (2005) Dipeptidyl peptidase IV and related enzymes in cell biology and liver disorders. Clin Sci (Lond) 108:277–292
Gragnani A, Warde M, Furtado F, Ferreira LM (2010) Topical tamoxifen therapy in hypertrophic scars or keloids in burns. Arch Dermatol Res 302:1–4
Hsu YC, Chen MJ, Yu YM, Ko SY, Chang CC (2010) Suppression of TGF-beta1/SMAD pathway and extracellular matrix production in primary keloid fibroblasts by curcuminoids: its potential therapeutic use in the chemoprevention of keloid. Arch Dermatol Res [Epub ahead of print]
Imaizumi R, Akasaka Y, Inomata N, Okada E, Ito K, Ishikawa Y, Maruyama Y (2009) Promoted activation of matrix metalloproteinase (MMP)-2 in keloid fibroblasts and increased expression of MMP-2 in collagen bundle regions: implications for mechanisms of keloid progression. Histopathology 54:722–730
Kischer CW, Wagner HN Jr, Pindur J, Holubec H, Jones M, Ulreich JB, Scuderi P (1989) Increased fibronectin production by cell lines from hypertrophic scar and keloid. Connect Tissue Res 23:279–288
Le AD, Zhang Q, Wu Y, Messadi DV, Akhondzadeh A, Nguyen AL, Aghaloo TL, Kelly AP, Bertolami CN (2004) Elevated vascular endothelial growth factor in keloids: relevance to tissue fibrosis. Cells Tissues Organs 176:87–94
Lee J, Fassnacht M, Nair S, Boczkowski D, Gilboa E (2005) Tumor immunotherapy targeting fibroblast activation protein, a product expressed in tumor-associated fibroblasts. Cancer Res 65:11156–11163
Liao WT, Yu HS, Arbiser JL, Hong CH, Govindarajan B, Chai CY, Shan WJ, Lin YF, Chen GS, Lee CH (2010) Enhanced MCP-1 release by keloid CD14+ cells augments fibroblast proliferation: role of MCP-1 and Akt pathway in keloids. Exp Dermatol 19(8):e142–e150
Lim CP, Phan TT, Lim IJ, Cao X (2009) Cytokine profiling and Stat3 phosphorylation in epithelial-mesenchymal interactions between keloid keratinocytes and fibroblasts. J Invest Dermatol 129:851–861
Lu F, Gao J, Ogawa R, Hyakusoku H, Ou C (2007) Biological differences between fibroblasts derived from peripheral and central areas of keloid tissues. Plast Reconstr Surg 120:625–630
Marneros AG, Krieg T (2004) Keloids—clinical diagnosis, pathogenesis, and treatment options. J Dtsch Dermatol Ges 2:905–913
Marneros AG, Norris JE, Watanabe S, Reichenberger E, Olsen BR (2004) Genome scans provide evidence for keloid susceptibility loci on chromosomes 2q23 and 7p11. J Invest Dermatol 122:1126–1132
Monsky WL, Lin CY, Aoyama A, Kelly T, Akiyama SK, Mueller SC, Chen WT (1994) A potential marker protease of invasiveness, seprase, is localized on invadopodia of human malignant melanoma cells. Cancer Res 54:5702–5710
Murray JC (1994) Keloids and hypertrophic scars. Clin Dermatol 12:27–37
Nassiri M, Woolery-Lloyd H, Ramos S, Jacob SE, Gugic D, Viciana A, Romanelli P, Elgart G, Berman B, Vincek V (2009) Gene expression profiling reveals alteration of caspase 6 and 14 transcripts in normal skin of keloid-prone patients. Arch Dermatol Res 301:183–188
O’Brien P, O’Connor BF (2008) Seprase: an overview of an important matrix serine protease. Biochim Biophys Acta 1784:1130–1145
Ohtsuru A, Yoshimoto H, Ishihara H, Namba H, Yamashita S (2000) Insulin-like growth factor-I (IGF-I)/IGF-I receptor axis and increased invasion activity of fibroblasts in keloid. Endocr J 47(Suppl):S41–S44
Park JE, Lenter MC, Zimmermann RN, Garin-Chesa P, Old LJ, Rettig WJ (1999) Fibroblast activation protein, a dual specificity serine protease expressed in reactive human tumor stromal fibroblasts. J Biol Chem 274:36505–36512
Pitche P (2006) What is true in “spontaneous” keloids? Ann Dermatol Venereol 133:501
Reinhold D, Kahne T, Steinbrecher A, Wrenger S, Neubert K, Ansorge S, Brocke S (2002) The role of dipeptidyl peptidase IV (DP IV) enzymatic activity in T cell-activation and autoimmunity. Biol Chem 383:1133–1138
Rettig WJ, Garin-Chesa P, Healey JH, Su SL, Ozer HL, Schwab M, Albino AP, Old LJ (1993) Regulation and heteromeric structure of the fibroblast activation protein in normal and transformed cells of mesenchymal and neuroectodermal origin. Cancer Res 53:3327–3335
Scanlan MJ, Raj BK, Calvo B, Garin-Chesa P, Sanz-Moncasi MP, Healey JH, Old LJ, Rettig WJ (1994) Molecular cloning of fibroblast activation protein alpha, a member of the serine protease family selectively expressed in stromal fibroblasts of epithelial cancers. Proc Natl Acad Sci USA 91:5657–5661
Seifert O, Bayat A, Geffers R, Dienus K, Buer J, Lofgren S, Matussek A (2008) Identification of unique gene expression patterns within different lesional sites of keloids. Wound Repair Regen 16:254–265
Seifert O, Mrowietz U (2009) Keloid scarring: bench and bedside. Arch Dermatol Res 301:259–272
Shih B, Bayat A (2010) Genetics of keloid scarring. Arch Dermatol Res 302:319–339
Tan EM, Hoffren J, Rouda S, Greenbaum S, Fox JW 4th, Moore JH Jr, Dodge GR (1993) Decorin, versican, and biglycan gene expression by keloid and normal dermal fibroblasts: differential regulation by basic fibroblast growth factor. Exp Cell Res 209:200–207
Tan EM, Rouda S, Greenbaum SS, Moore JH Jr, Fox JW 4th, Sollberg S (1993) Acidic and basic fibroblast growth factors down-regulate collagen gene expression in keloid fibroblasts. Am J Pathol 142:463–470
Tan KT, Shah N, Pritchard SA, McGrouther DA, Bayat A (2010) The influence of surgical excision margins on keloid prognosis. Ann Plast Surg 64:55–58
Thielitz A, Vetter RW, Schultze B, Wrenger S, Simeoni L, Ansorge S, Neubert K, Faust J, Lindenlaub P, Gollnick HP, Reinhold D (2008) Inhibitors of dipeptidyl peptidase IV-like activity mediate antifibrotic effects in normal and keloid-derived skin fibroblasts. J Invest Dermatol 128:855–866
Tuan TL, Nichter LS (1998) The molecular basis of keloid and hypertrophic scar formation. Mol Med Today 4:19–24
Uitto J, Perejda AJ, Abergel RP, Chu ML, Ramirez F (1985) Altered steady-state ratio of type I/III procollagen mRNAs correlates with selectively increased type I procollagen biosynthesis in cultured keloid fibroblasts. Proc Natl Acad Sci USA 82:5935–5939
Vignali DA (2000) Multiplexed particle-based flow cytometric assays. J Immunol Methods 243:243–255
Zhang GY, Yi CG, Li X, Zheng Y, Niu ZG, Xia W, Meng Z, Meng CY, Guo SZ (2008) Inhibition of vascular endothelial growth factor expression in keloid fibroblasts by vector-mediated vascular endothelial growth factor shRNA: a therapeutic potential strategy for keloid. Arch Dermatol Res 300:177–184
Acknowledgments
This study was supported by grants from the Edvard Welander Foundation, Finsen Foundation, from the Medical Research Council of Southeast Sweden (FORSS) and from the Olle Enkvist Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dienus, K., Bayat, A., Gilmore, B.F. et al. Increased expression of fibroblast activation protein-alpha in keloid fibroblasts: implications for development of a novel treatment option. Arch Dermatol Res 302, 725–731 (2010). https://doi.org/10.1007/s00403-010-1084-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-010-1084-x