Abstract
Background
Understanding the average time from surgery to discharge is important to successfully and strategically schedule cases planned for same day discharge (SDD) for total knee arthroplasty (TKA). The purpose of this study was to (1) evaluate the average time to discharge following unilateral TKA performed in a community hospital and (2) describe patient characteristics and peri-operative factors that may impact SDD.
Methods
This retrospective review included 75 patients having achieved SDD following unilateral TKA between March 2017 and September 2021 at a high-volume multi-specialty community hospital. Time to discharge was calculated from end of surgery, defined as completion of dressing application, to physical discharge from the hospital. Time surgery completed and association with time of discharge was also examined. Pearson’s correlations were performed to evaluate the relationship between total time to discharge and patient demographics.
Results
The average age for all patients was 66.6 ± 10.9 years (Range: 38 to 86) and average BMI of 29.9 ± 5.6 kg/m2 (Range: 20.4 to 46.3). The average time to discharge was 5.8 ± 1.8 h (range: 2.2 to 10.5 h). Time to discharge was significantly longer for patients finishing surgery prior to noon (6.0 ± 1.8 h), than after noon (4.8 ± 1.4 h, p = 0.046). Total time to discharge was not correlated with age (r = 0.018, p = 0.881) or BMI (r=-0.158, p = 0.178), but was negatively correlated with surgical start time (r=-0.196, p = 0.094).
Conclusion
An average of six hours was required to achieve SDD following unilateral TKA performed in a community hospital. The time required for SDD was not found to be related to intrinsic patient factors but more likely due to extrinsic factors associated with time of scheduled surgery. To improve success of SDD, focus should be placed on the development of efficient discharge pathways rather than unchangeable intrinsic patient characteristics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Annually, 700,000 total knee arthroplasties (TKA) resulted in over $12.3 billion in hospital costs [1]. With 3.5 million TKAs expected to be performed annually by 2030 [2], pathways to reduce cost of care must be evaluated [3]. Although associative costs of TKA vary greatly [4], increasing same day discharge (SDD) rates is one potential strategy for decreasing overall costs [5]. Pathways to achieve SDD have been highly successful in ambulatory surgical centers (ASC) involving highly selected patients [6]. However, SDD rates remain significantly lower for TKA performed in a hospital setting [7]. With increasing pressure to reduce cost of care associated with TKA, surgeons are attempting to increase the rates of successful SDD following TKA and many are considering transitioning to ASCs [7, 8].
For surgeons transitioning to the performance of outpatient or SDD TKA, it is important to understand the time necessary to discharge patients from the facility in question. Understanding the average time it takes to physically discharge a patient from the hospital is important to understand how to strategically schedule cases planned for SDD. Additionally, for surgeons considering transitioning to an ASC with limited hours of operation, it is important to know when surgeries should plan to end to comply with hours of operation. Previous studies have indicated that time to discharge ranges from four to eight hours [9]. However, such information may be institution-specific and with limited studies available, more data is required to determine if such discharge time frames are similar in other institutions. Furthermore, it is important to identify potential barriers to achieving SDD for patients undergoing unilateral TKA. Therefore, the purpose of this study was to (1) evaluate the average time to discharge following unilateral TKA performed in a high volume, multispecialty community hospital and (2) identify patient characteristics and peri-operative variables that potentially affect the length of time to discharge.
Materials and methods
This was an institutional review board approved retrospective review of all patients having achieved SDD following unilateral TKA between September 2017 and June 2022. All procedures examined were performed at a high-volume multi-specialty community hospital with at least 10 years of experience with fast-track arthroplasty service. Patients who were highly selected to undergo TKA at a private, non-hospital affiliated stand-alone ASC were excluded as these patients represented younger, highly motivated patients determined to achieve SDD which is not representative of the average patient undergoing TKA at the current study institution. All surgeries were performed by a single, high volume [10] fellowship trained orthopedic surgeon. All patients met the standard clinical and radiographic indications for primary unilateral TKA. The current study site does not exclude patients from undergoing TKA based on demographic or comorbidity status. All patients scheduled to undergo unilateral uncomplicated primary TKA at the study institution are treated with the intention for SDD. Therefore, only patients requiring primary unilateral TKA who received primary TKA implants, patients with diagnoses of osteoarthritis and patients requiring simple hardware removal at the time of index arthroplasty who received primary TKA implants were included. Patients with inflammatory systemic arthritic diagnoses, patients undergoing revision TKA or those requiring revision implant systems due to projected complexity of reconstruction at the time of index arthroplasty were excluded. Each patient received surgical clearance from a primary care physician, an anesthesiologist, and a medical specialist if required. All patients are screened by a core group of experienced anesthesiologists as part of the Perioperative Surgical Home initiative put forth by the American Society of Anesthesiologists (ASA) [11], and ASA classification was performed by a small core group of anesthesiologists experienced in arthroplasty patient assessment and management.
The first surgical case of the day starts with an incision time of approximately 8:00 am and cases are performed in sequence as scheduled with the second case usually having a start time before 9:30 am. Eight to ten knee or hip arthroplasty cases are typically performed per surgical day. Prior to surgery, all patients received antibiotic prophylaxis of either cefazolin or vancomycin. All patients received 500 mg-1000 mg of acetaminophen based on body weight, unless contraindicated. An ultrasound-guided adductor canal nerve block was given prior to induction by the attending anesthesiologist, containing bupivacaine 0.5% (20 cc), epinephrine (100mcg) and clonidine (1mcg/kg). All patients received a pericapsular injection primarily targeting the posterior capsule consisting of bupivacaine 0.15% (1 cc/kg) and toradol (30 mg). All surgeries were performed under general anesthesia. General anesthesia has been used for over a decade at the current study site as it has been safe and conducive to rapid discharge protocols following total joint arthroplasty [12]. Due to avoidance of spinal anesthesia, foley catheters were not used unless patients required preoperative catheter use. A medial parapatellar approach using conventional instrumentation was used for all patients. Tourniquets were used in all patients and was inflated prior to incision and released just prior to closure of the arthrotomy. All patients received one gram of intravenous tranexamic acid prior to incision and before closure of the arthrotomy. Following wound closure, dexamethasone (4 mg) was administered to each patient intravenously to control post-operative nausea. Post-operative pain management primarily included acetaminophen with oral narcotics provided only upon patient request for break through pain. Post-operative nausea was symptomatically treated with anti-emetics. Thromboembolic stockings were not used.
All patients who underwent TKA during the study period were treated with the same rapid discharge protocol previously described and all patients had the expectation to achieve SDD [7, 13, 14]. Under the rapid discharge protocol, physical therapy services were available until 8:00pm to help facilitate SDD. Discharge criteria included the ability to walk 50 feet with an assistive device, successful negotiation of stairs (if required in the home environment), pain and nausea controlled, and hemodynamic stability. If patients failed to achieve SDD, home discharge was expected on postoperative day one. If patients demonstrated inability to achieve home discharge by postoperative day one, plans for acute rehabilitation or skilled nursing facility transfer was pursued.
Data collected included patient demographics (sex, age, BMI, ASA, self-reported race [Asian, Caucasian, other]) and surgical start and end time. The end of surgery was defined as the completion of dressing application. Time to discharge was calculated from end of surgery to physical discharge from the hospital. Noon was chosen as the time point for dichotomized comparison as studies have suggested surgeries completed after noon may negatively influence success rates for SDD [15, 16]. Descriptive statistics were created for each variable, including mean, standard deviation, range and frequency. Data were determined to be parametric by the Kolmogorov-Smirnov test. Therefore, independent t-tests were performed to evaluate gender difference in age, body mass index and time to discharge. Time to discharge was also compared between surgeries ending prior to and after noon. Pearson’s correlations were performed to evaluate the relationship between total time to discharge and patient demographics. All statistical procedures were performed using SPSS version 25, with a significant level set to p < 0.05.
Results
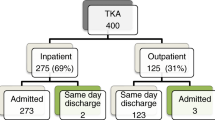
During the study period, 490 unilateral TKAs were performed. Forty-three patients underwent TKA at a non-hospital affiliated ambulatory surgical center (ASC), all of which achieved SDD, and were excluded as those patients represented a highly selected group. Of the remaining 447 unselected community hospital patients, 75 patients (12.5%) achieved SDD, including 46 male (64.2%) and 28 female (35.8%) patients (Table 1). The average age and BMI of all patients were 66.6 ± 10.9 years (Range: 38 to 86) and 29.9 ± 5.6 kg/m2 (Range: 20.4 to 46.3), respectively. When evaluated by gender, there was no significant difference for age (Males: 66.6 ± 9.1; Females: 66.5 ± 11.3; p = 0.964) or BMI (Males: 30.5 ± 5.4 kg/m2; Females: 28.9 ± 5.9 kg/m2; p = 0.253). Thirty-nine patients (52.0%) were ASA 3 and thirty-six (48.0%) were ASA 2. There were 29 (39.2%) Asians, 28 (37.8%) Caucasians, and 17 (23.0%) who self-reported as Other (Table 1). The average total surgical time for all patients was 64.0 ± 12.8 min (range: 43 to 104 min), with an average time to discharge of 5.8 ± 1.8 h (range: 2.2 to 10.5 h) (Table 1). Only three patients were reported to have post-operative nausea. The average time to discharge for these three patients was 5.9 ± 1.8 h (range: 1.3 to 10.4 h).
Sixty-seven patients started surgery prior to noon, with 63 patients finishing surgery prior to noon (Table 1). Time to discharge was significantly longer for patients finishing surgery prior to noon (6.0 ± 1.8 h), than after noon (4.8 ± 1.4 h) (p = 0.046) (Table 2). Thirty-five patients (46.7%) started surgery prior to 9:30am, indicating that only those patients underwent surgery as the first or second case of the day (Table 1). Discharge times ranged from 11:28am to 7:31pm, with 33 patients (44.6%) being discharged after 5:00pm (Table 1). Total time to discharge was not correlated with age (r = 0.018, p = 0.881) or BMI (r=-0.158, p = 0.178) but was negatively correlated with surgical start time (r=-0.196, p = 0.094). There was no difference in time to discharge between sexes, patients younger or older than 70, ASA categories 2 or 3, obese (BMI ≥ 30.0) and non-obese (BMI < 30.0) patients or between the three racial groups examined. Time to discharge was not significantly longer for patients whose procedures exceeded 60 min or for patients who experience postoperative nausea. The only factor found to be associated with a significantly shorter time to discharge was surgical end time after noon (Table 2).
Discussion
As the number of annual TKAs continue to increase, cost reduction will continue to be a priority. For surgeons looking to increase the success rate of SDD or transition cases to an ambulatory surgical center, knowing the time required to discharge is important in understanding how best to schedule cases to achieve the greatest success. In this study, the average time from surgical end to discharge was just over 5 and a half hours, which is consistent with the four to eight hours previously reported [9, 16, 17]. Although 89% of cases were able to start prior to noon, only 35 patients started prior to 9:30am, suggesting that other arthroplasty procedures, specifically the unicompartmental knee arthroplasty, were prioritized prior to TKA. In a high-volume center, performing multiple hip and knee arthroplasties, the number of cases which can be scheduled prior to 10:00am is limited.
The second objective of this study was to evaluate the influence of perioperative variables and patient demographics on total discharge time. While previous research has identified age and gender as risk factors for delayed discharge [18, 19], the current study found no significant association of any specific patient variables, such as age or BMI, on delayed discharge. Interestingly, the average discharge time was approximately 71 min shorter for patients finishing surgery after 12:00pm. While the reason for faster discharge for patients ending surgery after 12:00pm could not be fully determined, it is likely related to a decrease in patient demands on surgical admission center (SAC) and post-anesthesia care unit (PACU) nursing staff as early morning patients are discharged and patient load demands decrease throughout the day. Additionally, patients were generally not evaluated by a physical therapist in the PACU, nor were discharged directly from the PACU. Therefore, mid-day surgical patients may have faced a delay in time to discharge if no beds were available in the SAC or on the floor. At the current institution, patient discharges are planned to occur at or just after noon, therefore, patients awaiting transfer from PACU to the floor prior to noon may have to wait until a bed opens as patients are discharged. Patients ending surgery after noon may be transferred for physical therapy evaluation sooner as beds have already been vacated following noon discharges. To assist with these potential delays, the current study site provided physical therapy services until 8:00pm. This institutional change was important to the success of SDD, as 55.4% of patients were able to discharge by 5:00pm. However, 45% were discharged after 5:00pm with six patients requiring discharge after 7:00pm. The unusual finding that surgeries ending after noon required less time to discharge highlights an important lesson for surgeons trying to develop outpatient or SDD arthroplasty services; understanding overall hospital operations (surgical volume trends, average number of open beds, physical therapy capacity etc.) is important to designing successful outpatient arthroplasty services. In this institution where surgical volumes are greatest before noon, hospital bed availability is low prior to noon and physical therapy evaluation was only allowed after being transferred to a floor bed, cases ending after noon required less time simply due to decreased afternoon patient loads. It is important for surgeons and administrators to understand these factors surrounding hospital operations to best design successful programs. The current findings which demonstrated that SDD required 5–6 h following TKA performed in a high arthroplasty volume, experienced community hospital system should serve as a guide for differing medical systems. If similar support is available for arthroplasty patients, similar results may be expected, if such systems are not well developed, outpatient arthroplasty services will likely fail to achieve SDD.
There were a few limitations to the current evaluation. First, the current study site has over ten years of high volume, fast-track arthroplasty experience and these results may not be generalizable to settings where highly coordinated multidisciplinary management of arthroplasty patients have not been developed. Surgeons and administrators of hospitals without such supportive integrated systems must understand that SDD will be an unrealistic goal as the current study has demonstrated that even with such robust systems of support, SDD following TKA performed in a hospital setting required five to six hours to achieve. Second, the retrospective nature of the study did not allow for the collection of specific reasons for increased time to discharge. Specifically for patients finishing surgery prior to noon, the authors can only speculate that the increased time to discharge was due to higher hospital patient loads in the morning hours and not due to patient specific factors. The current study highlights the importance of understanding the specifics of individual hospital operations. Surgeons need to understand their specific institution’s volume, size and post-operative patient processing protocol in order to best plan strategies to achieve SDD. The current findings should make clear that hospital organization and protocols have a greater influence on SDD than intrinsic patient characteristics. Finally, the current study involved a relatively small number of patients (n = 75) and future studies should evaluate larger cohorts for a better understanding of the feasibility of performing high volume SDD TKA within a hospital setting.
Conclusion
Successful implementation of a rapid, discharge pathway to achieve SDD necessitates an understanding of both the time required for discharge and reasons for potential delays in patient navigation and staff evaluation. Given the specific barriers presenting in this high-volume community hospital, an average of six hours was required to achieve SDD following unilateral TKA. For surgeons developing outpatient TKA services in a community hospital setting or considering transitioning cases to an ASC, this time should be allotted for by either early surgical start times or extended facility and staffing hours.
References
Fingar KR, Stocks C, Weiss AJ, Steiner CA (2006) Most Frequent Operating Room Procedures Performed in U.S. Hospitals, 2003–2012: Statistical Brief #186. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD)
Kurtz S, Ong K, Lau E, Mowat F, Halpern M (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 89(4):780–785
Featherall J, Brigati DP, Arney AN, Faour M, Bokar DV, Murray TG, Molloy RM, Higuera Rueda CA (2019) Effects of a total knee arthroplasty care pathway on cost, Quality, and patient experience: toward measuring the Triple Aim. J Arthroplasty 34(11):2561–2568
Haas DA, Kaplan RS (2017) Variation in the cost of care for primary total knee arthroplasties. Arthroplast Today 3(1):33–37
Bertin KC (2005) Minimally invasive outpatient total hip arthroplasty: a financial analysis. Clin Orthop Relat Res (435): 154–163
Singletary D (2016) Evaluation of the safety and efficacy of same-day discharge following outpatient surgery in a US hospital. Nurs Manag (Harrow) 23(4):34–38
Naito K, Matsumoto M, Andrews SN, Mathews K, Nakasone CK (2023) Can a community hospital successfully transition to outpatient total knee arthroplasty in unselected patients? Knee 41:322–328. https://doi.org/10.1016/j.knee.2023.01.014Epub 2023 Feb 20. PMID: 36812750
Yap LK, Ow KH, Hui JY, Pang WS (2002) Premature discharge in a community hospital. Singap Med J 43(9):470–475
Bodrogi A, Dervin GF, Beaule PE (2020) Management of patients undergoing same-day discharge primary total hip and knee arthroplasty. CMAJ 192(2):E34–E39
Laucis NC, Chowdhury M, Dasgupta A, Bhattacharyya T (2016) Trend toward High-volume hospitals and the influence on complications in knee and hip arthroplasty. J Bone Joint Surg Am 98(9):707–712
Kain ZN, Vakharia S, Garson L, Engwall S, Schwarzkopf R, Gupta R, Cannesson M (2014) The perioperative surgical home as a future perioperative practice model. Anesth Analg 118(5):1126–1130
Stambough JB, Bloom GB, Edwards PK, Mehaffey GR, Barnes CL, Mears SC (2019) Rapid Recovery after Total Joint Arthroplasty Using General Anesthesia. J Arthroplasty 34(9):1889–1896
Nakasone CK, Combs D, Buchner B, Andrews S (2020) Day of surgery discharge success after implementation of a rapid discharge protocol following unilateral unicompartmental knee arthroplasty. Knee
Matsumoto M, Saito S, Andrews S, Mathews K, Morikawa L, Nakasone C (2020) Barriers to achieving same day discharge following unilateral unicompartmental knee arthroplasty. Knee 27(5):1365–1369
Rytter S, Jensen BG, Munk S, Hovsgaard SJ, Hansen TB (2019) A prospective study of day of surgery discharge in 368 consecutive patients with unicompartmental knee replacement. Dan Med J ;66(9)
Berger RA, Kusuma SK, Sanders SA, Thill ES, Sporer SM (2009) The feasibility and perioperative complications of outpatient knee arthroplasty. Clin Orthop Relat Res 467(6):1443–1449
Gillis ME, Dobransky J, Dervin GF (2019) Defining growth potential and barriers to same day discharge total knee arthroplasty. Int Orthop 43(6):1387–1393
Falcone D, Bolda E, Leak SC (1991) Waiting for placement: an exploratory analysis of determinants of delayed discharges of elderly hospital patients. Health Serv Res 26(3):339–374
Ohwaki K, Hashimoto H, Sato M, Tokuda H, Yano E (2005) Gender and family composition related to discharge destination and length of hospital stay after acute stroke. Tohoku J Exp Med 207(4):325–332
Acknowledgements
Not applicable.
Funding
This research received no specific grant from any funding agency in the public, commercial or non-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Conceptualization: Cass K. Nakasone. Methodology: Cass K. Nakasone. Formal statistical analysis: Samantha Andrews. Data collection: Krystin Wong. Writing ? original draft preparation: Maveric Abella, Vera Ong. Writing ? reviewing and editing: Maveric Abella, Vera Ong, Samantha Andrews, Cass K. Nakasone. Supervision ? Cass K. Nakasone. Project administration ?Cass K. Nakasone.
Corresponding author
Ethics declarations
Ethical approval
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Hawai‘i Pacific Health Research Institute (local Western Institutional Review Board) approved this study.
Informed consent
This was a retrospective chart review and data collected were deidentified and presented as large scale, aggregate data. Therefore, no informed consent was obtained or required by the IRB.
Conflict of interest
Author Cass K. Nakasone is a consultant and receives royalties from Ortho Development Inc. but not related to the subject matter discussed in this manuscript. All other authors certify that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abella, M., Ong, V., Wong, K. et al. Time from surgery end to discharge following total knee arthroplasty: implications for same day discharge. Arch Orthop Trauma Surg 144, 2789–2794 (2024). https://doi.org/10.1007/s00402-024-05370-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-024-05370-x