Abstract
Background
Outpatient arthroplasty programs are becoming well established. Adverse event rates have been demonstrated to be no worse than inpatient arthroplasty in the literature for selected patients. The purpose of this study was to determine our rate of outpatient total knee arthroplasty (TKA), examine justification for exclusions, and estimate the proportion of TKAs that can occur safely on an outpatient basis.
Methods
Retrospective case series of 400 consecutive TKAs from Oct 2014 to Mar 2017. Patient demographics, allocation to outpatient surgery vs standard admission, and reason for exclusion from outpatient surgery were recorded. Ninety-day Emergency department (ED) visits, readmission rates, and length of stay (LOS) were compared between groups using independent sample t test and Chi-squared test.
Results
Outpatients were younger (p = 0.001), had lower BMI (p < 0.001), and ASA scores (p < 0.001) than inpatients. One hundred twenty-five (31%) TKAs were assigned to outpatient surgery and 123 achieved discharge on the same day. There was no difference in 90-day ED visits (p = 0.889) or readmission rates (p = 0.338) between groups. Reasons for exclusion from outpatient surgery included medical (absolute 43% and relative 31%), distance > one hour from hospital (18%), no help (7%), and other/unclear (10%). LOS was significantly longer for medical than non-medical exclusions (p < 0.001) and for the absolute compared to relative medical exclusions (p = 0.004).
Conclusion
Outpatient TKA is safe in selected patients, and inclusion can likely be broadened by addressing modifiable exclusions and narrowing medical exclusions. We found that 55% of our TKA population could be appropriate for outpatient surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Outpatient total knee arthroplasty (TKA) has grown in popularity in the last decade due to positive findings, namely safety [1, 2] and cost savings [3, 4]. Cost savings in both the Canadian and American healthcare systems have been demonstrated, in the order of $3300 CAD [4] and up to $8000 USD [3] in savings per case. A recent study reported that patients undergoing outpatient total hip arthroplasty (THA) were satisfied and would recommend it to others [5]. Patient perception towards outpatient arthroplasty pre-operatively was found to be mixed and education was thought to be important to ensure that expectations were appropriate and satisfaction achieved [6, 7].
Many cohort studies have explored the safety of fast track and 23 hour stay TKA programs, with more recent studies focusing on true same day discharge (SDD) outpatient surgery programs. Berger pioneered outpatient TKA, by first reporting on 50 selected patients [1] and then on 111 unselected patients [2]. Several authors that have published on the topic of outcomes in ‘outpatient arthroplasty’ focused on adverse event rates [8, 9], risk factors for admission [10], and length of stay [11]. It is important to note that these studies were not truly examining true SDD outpatient surgery programs, but rather 23 hour discharge programs [9, 12]. However, a recently published study from our center demonstrates safety of the Outpatient Total Knee Arthroplasty Program, reporting no difference between outpatient and inpatient surgery, for emergency department visits in the first 90 days and no difference in quality of recovery (QoR-9) and no difference in two year functional outcomes (KOOS, WOMAC scores) [13].
There is agreement that certain patients remain inappropriate for outpatient arthroplasty, and various patient factors have been identified as being associated with unacceptable risk, such as history of cardiovascular disease, chronic renal or hepatic failure, morbid obesity, insulin-dependent diabetes mellitus, and being in a dependent functional state [2, 14, 15]. In order to safely optimize the economic benefits of outpatient TKA, it is important to understand their current rates and determine the barriers to allow for appropriate modifications. To our knowledge, there are no evidence-based guidelines or estimates that have assessed either current rates of true outpatient TKA, nor estimated the ultimate potential rate of such a pathway for a population of patients seeking TKA. Meninghini has developed a risk assessment score for predicting which patients are appropriate for outpatient surgery [6], but few studies have holistically explored the barriers to SDD TKA. As such, the purpose of this study was to examine current rate of outpatient TKA in a center with established protocols, elicit the reasons for exclusion, and estimate the potential for this pathway after determining what can be modified among the exclusions described.
Methods
This is an IRB-approved, retrospective, single surgeon case series which took place at a large academic, tertiary care centre with an established outpatient SDD TKA program developed by the senior author. Four hundred consecutive primary TKA cases performed at this site were reviewed between Sept 2014 and June 2017 to evaluate the appropriateness of our selection criteria and to describe the safety profile in this series as defined by 90-day readmissions to the hospital for reasons related to the initial TKA.
Outpatient total knee arthroplasty technique
The outpatient surgery program at our center depended on a coordinated multidisciplinary approach. Outpatient cases were discharged home on the day of surgery, generally within eight hours of surgery, and overnight stays were considered admissions/failure of outpatient surgery. All patients were carefully selected to ensure safe assignment to the outpatient surgery program (Table 1). Furthermore, both inpatients and outpatients were encouraged to complete necessary prescriptions for post-operative medications and to rent a cryo compressive device for post op analgesic and swelling control [16].
Cases for outpatient surgery occurred as the first or second case of the day to allow adequate time for recovery before a late afternoon or early evening discharge. A consistent anaesthetic protocol was applied to all patients and involved minimal impact pre-operative fasting, allowing clear fluids until two hours before surgery. All patients received pre-operative adductor canal blocks (with or without indwelling catheter which may last up to 3–4 days post-operatively) unless contraindicated and low dose; short acting spinals (without narcotic) were used as the preferred method of anaesthesia. When possible, subvastus approach was used preferentially over medial parapatellar arthrotomy. Tourniquet use was restricted to cementation of components. Local infiltration analgesia by periarticular injection with local anesthetic and non-steroidal anti-inflammatory was performed.
Prior to discharge, outpatients were mobilized by a physiotherapist (including transfers, ambulation, stairs). Patients must have achieved adequate pain control, tolerated oral intake, and voided urine without difficulty. A post-operative dose of antibiotics was administered six hours post-operatively for the outpatient group. On the first post-operative day, patients were visited at home by a home care nurse for wound/dressing check and by a community physiotherapist to review initial exercises once more, with further formal physiotherapy to occur at outpatient clinics. All TKA patients were seen by the surgeon for follow-up at two weeks after surgery, at six weeks, three months, and one year, assuming an uncomplicated course.
Data collection
Data collection included patient demographics: age, gender, BMI, and medical comorbidities. Pre-operative patient allocation to outpatient versus inpatient surgery was recorded. Reasons for exclusion from outpatient surgery were derived from a chart review, and these were categorized for each inpatient as medical and non-medical (distance, no help, other preference, or nothing documented). Medical was further subcategorized into absolute, which we reserved for irreversible organ failure such as kidney failure, liver failure, or severe cardiac failure as well as patients over 80. Relative medical contra indications were those where we found some discrepancy and controversy in literature as to the impact on length of stay and post-op readmission and comorbidities. Outcome measures collected included disposition after surgery (i.e., outpatient vs inpatient), length of stay (LOS), and 90-day readmissions (all reasons included). The capture of these events was dependent on presentation to the main surgical centre or affiliate site such that it was visible on the electronic medical record or was documented in the post-discharge follow-up phone call or at the time of follow-up with the surgeon.
Statistics
The Kolmogorov-Smirnov test demonstrated that continuous data was normally distributed. Independent sample t tests and Chi-square tests were used for comparing continuous variables and categorical variables, respectively. SPSS version 22.0 (IBM) was used, with significance set at p value of 0.05.
Results
Demographics
The outpatient SDD surgery pathway was assigned to 125 of the 400 patients, leaving 275 inpatients. Comparison of demographic data between the groups revealed that the outpatient group was significantly younger than the inpatient group (mean age 62.9 and 66.0, respectively) and had significantly lower mean BMI (28.8 and 33.5, respectively) and ASA scores (2.16 and 2.59, respectively) (Table 2).
Disposition
Within the group of 125 cases assigned to outpatient surgery, all but three patients achieved discharge on the day (afternoon or evening) of surgery (Fig. 1 ). Two admissions were after a significant vasovagal episode and another for ongoing surgical wound bleeding. Two patients that had been assigned to standard admission switched to outpatient surgery upon their request to be discharged from the recovery room. Both were discharged uneventfully on the day of surgery.
Exclusions from outpatient TKA
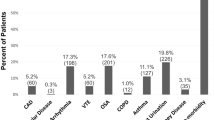
Categories were assigned to reasons for exclusion from outpatient surgery. These included medical: absolute and relative and non-medical (Table 1). Cases excluded from outpatient surgery, thus allocated to inpatient surgery, were 275 of 400 case series (68.8%) (Fig. 2 ). Medical exclusions: absolute and relative were applied to 118 (30%) and 77 (19%), respectively. Distance exclusion could be applied to 49 cases (12.3%) but existed as the sole reason for exclusion in only 33 cases (8.2%). Twenty-one (5.3%) cases were excluded for having inadequate support at home. Finally, there were 26 (6.5%) inpatient cases where we could not confirm any clear medical, support, or geographic exclusion barriers. Other reasons were not always clearly indicated on the patient’s chart, and may have included frailty or poor mobility, or patient refusal or apprehension regarding having outpatient TKA pathway. We further classified exclusions from outpatient surgery of the medical nature as non-modifiable 188 (47%) whereas the remaining 59 (14.5%) comprised exclusions relating to distance from hospital, assistance at home, and “other”, as potentially modifiable barriers (Fig. 3).
A total of 275 (69%) of 400 TKA were excluded from outpatient surgery. Exclusion reasons are shown as percentage of all 400 TKAs; were medical: absolute and relative, distance, lack of help at home, and other. Thirty-three patients were excluded based on distance and lacked other reasons for exclusion
Clinical outcomes
All TKA cases were followed up at the tertiary center by the senior author. There were 17 (13.6% of 125 cases) and 36 (13.1% of 275 cases) emergency department visits in the first 90 days after surgery for the outpatient surgery group and the inpatient group, respectively. Readmission to hospital after discharge (all reasons) occurred for 3 (2.4% of 125) cases in the outpatient group and 12 (4.4% of 275) in the inpatient group. There was no significant difference between outpatient and inpatient groups in either rates of 90-day postoperative visits to the emergency department (p = 0.88) or readmission (p = 0.34). More specifically, there was found to be no significant difference in rate of presentation to the emergency department within the first post-operative week: eight visits within the group of 125 outpatients, 12 visits within the group of 275 inpatients (p = 0.386); all visits during this time frame for both groups were specific to the surgery: either poorly controlled pain, swelling, or wound concerns.
Length of stay
Examination of LOS for the admitted patients revealed that LOS varied significantly according to exclusion reason. Median LOS (acute surgical and extended stay included) for all inpatients was 2.0 days. Patient median LOS was 3.0 and 2.0 days when excluded from outpatient surgery for absolute and relative medical exclusions, respectively. However, patients excluded for distance alone and ‘other’ had shorter LOS: 2.0 and 1.0, respectively. There was a statistically significant difference in LOS for all medical exclusions (median 3.0, range 1–51 days) vs all non-medical exclusions (mean 2.0, range 1–13 days) (p = 0.030), as well as for absolute (median 3.0, range 1–51 days) vs relative (median 2.0, range 1–24 days) medical exclusions (p = 0.004) (Table 3).
Discussion
Over the past decade, great strides have been made towards improved recovery for TKA patients. The pinnacle of fast track arthroplasty is outpatient surgery with its associated cost savings in both the Canadian and American systems. When using generally accepted risk factors for complications as exclusion criteria, we found that our current selection process and outpatient program were successful in rate of successfully completed outpatient cases (98% of 117 cases) and safe with no increased rates of our measured adverse events between outpatient and standard admission patients. Furthermore, we have demonstrated a 2.6% 90-day readmission rate using our selection criteria for outpatient TKA, compared to a rate of 7.2% in a published unselected series [2].
Length of stay in hospital has diminished dramatically, with a focus on fast track pathways, early mobilization, and multimodal pain control. Several studies have examined alternate modalities, such as peri-articular injections of local anaesthesia to replace patient controlled analgesia [17] and adductor canal block in the place of femoral nerve block to provide better ambulation ability, faster functional recovery, and better pain control [18]. Further to advances in pain control, different surgical approaches are also being explored to minimize hospital stay. Of note is the mini subvastus approach, which has been demonstrated to offer faster recovery, less pain, and shorter hospital stay without compromising principles of proper prosthesis position and limb alignment when compared to the medial parapatellar approach [19]. The aforementioned studies demonstrate the constant evolvement of peri-operative and post-operative techniques, which have the capacity of decreasing length of stay and improving patient outcomes.
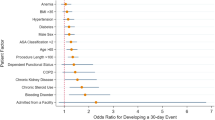
While there is consensus that an outpatient pathway is not for all patients, there is not necessarily agreement as to which particular risk factors for adverse events make admission necessary to ensure safety. In a retrospective review of 1012 consecutive TJA cases at a high-volume center, ischaemic heart disease, congestive heart failure, chronic obstructive pulmonary disease, and liver cirrhosis were identified to be risk factors with odds ratios of 2.8, 9.71, 4.16, and 8.19, respectively, for adverse events. However, BMI, DM2, age, and kidney disease were not independent risk factors [20]. In a more recent, large retrospective database review, creatinine values greater than 1.5 mg/dL were associated with increased readmission (odds ratio 1.89, p < 0.001). Cognitive decline, frailty, smoking, BMI, and malnutrition also contribute to risk [10, 15, 21]. A large series of 13,517 TKA and THAs, published by Pulido and colleagues, demonstrated rates of 3.6 and 3.47 for major and minor systemic complications, respectively [22]. Risk assessment tools are limited, with the American College of Surgeons Risk Calculator shown to be poorly applied to the arthroplasty population [23]. The Outpatient Arthroplasty Risk Assessment tool may improve that performance demonstrating increased positive predictive value (81.6%) for same day or next day discharge than did patient ASA score or the Charlson Comorbidity index [6].
Medical exclusions applied clearly to 40% of our TKA population. This study also demonstrated a significantly shorter LOS noted in the relative vs absolute medical exclusion categories supporting the notion that the exclusion criteria outlined in these categories do represent different populations in terms of expected outcomes. Further study is required to better delineate which medical exclusions could be given a threshold level or disability or dysfunction to permit a more discerning process in selection/exclusion. The definition of what constitutes significant compromising chronic condition is unclear and thresholds for these diagnoses have not been determined.
Finally, we aimed to determine what the potential safe expansion of the outpatient SDD pathway could be, based on current evidence and our applied screening process. Medical comorbidities are fixed, and while thresholds for exclusions can potentially be lowered, the medical status of the patient is the important determinant of safety and thus will remain the major non-modifiable limitation to expansion of outpatient TKA. As outpatient arthroplasty is a developing strategy, attention should be first directed towards addressing barriers to access, which are least likely to risk patient safety such as support and distance to treating hospital which can be modifiable with various strategies. Possible solutions would include local accommodations for patients otherwise fit for outpatient TKA—as is done for various outpatient surgeries for patients that live remotely and do not otherwise require admission. Regarding home support, patients without adequate help at home could perhaps access convalescent care or home care nursing support could be instituted to avoid unnecessary acute bed admissions. These alternative strategies may be more cost-effective, whether incurred by the patient or the system and avoiding admissions that are not “medically necessary” would free up bed allotment for medically necessary conditions.
Limitations
This was a retrospective review and as such the definitive exclusion reasons collected from chart review relied on information that was present either in the office or hospital chart. Emergency department visit and readmission data were restricted to capture the event via presentation/admission to a center linked to the electronic medical record or captured within documentation at the time of follow-up. The study population (urban) may not adequately represent the demographics of other regions in terms of age, BMI, medical comorbidities, socioeconomic status, and size of catchment area/referral base. Furthermore, patient perceptions were not compared between the outpatient and inpatient groups and should be evaluated in future studies. Another key element to consider is patient education prior to surgery. A recent study conducted by O’Reilly and colleagues demonstrated that pre-operative educational sessions remain effective ways of delivering content to patients regarding their surgery[7], and this may therefore improve post-operative outcomes for patients going home the same day.
Conclusions
We found no increased rate of 90-day emergency visits or readmissions relative to the usual inpatient population. It is unlikely that we can narrow the absolute contraindications without risk; it is of note that these patients have a significantly longer LOS than other inpatient TKA cases. We estimate that roughly 55% of the TKA population in this region could be safely considered for outpatient TKA. Current experience in outpatient arthroplasty demonstrates that quality of recovery and functional outcomes are no different for outpatients than inpatients [13]. Addressing barriers to outpatient surgery through an improved understanding of both risk, as well as the patient experience, will promote efficiency in outpatient arthroplasty pathways.
References
Berger RA, Sanders S, Gerlinger T, Della Valle C, Jacobs JJ, Rosenberg AG (2005) Outpatient total knee arthroplasty with a minimally invasive technique. J Arthroplast 20:33–38
Berger RA, Kusuma SK, Sanders SA, Thill ES, Sporer SM (2009) The feasibility and perioperative complications of outpatient knee arthroplasty. Clin Orthop Relat Res 467(6):1443–1449. https://doi.org/10.1007/s11999-009-0736-7
Lovald ST, Ong KL, Malkani AL, Lau EC, Schmier JK, Kurtz SM, Manley MT (2014) Complications, mortality, and costs for outpatient and short-stay total knee arthroplasty patients in comparison to standard-stay patients. J Arthroplast 29(3):510–515
Huang A, Ryu J-J, Dervin G (2017) Cost savings of outpatient versus standard inpatient total knee arthroplasty. Can J Surg 60(1):57
Dorr LD, Thomas DJ, Zhu J, Dastane M, Chao L, Long WT (2010) Outpatient total hip arthroplasty. J Arthroplast 25(4):501–506. https://doi.org/10.1016/j.arth.2009.06.005
Meneghini RM, Ziemba-Davis M, Ishmael MK, Kuzma AL, Caccavallo P (2017) Safe selection of outpatient joint arthroplasty patients with medical risk stratification: the “outpatient arthroplasty risk assessment score”. J Arthroplast 32(8):2325–2331
O'Reilly M, Mohamed K, Foy D, Sheehan E (2018) Educational impact of joint replacement school for patients undergoing total hip and knee arthroplasty: a prospective cohort study. Int Orthop. https://doi.org/10.1007/s00264-018-4039-z
Bovonratwet P, Ondeck NT, Nelson SJ, Cui JJ, Webb ML, Grauer JN (2017) Comparison of outpatient vs inpatient total knee arthroplasty: an ACS-NSQIP analysis. J Arthroplast 32(6):1773–1778
Lovecchio F, Alvi H, Sahota S, Beal M, Manning D (2016) Is outpatient arthroplasty as safe as fast-track inpatient arthroplasty? A propensity score matched analysis. J Arthroplast 31(9):197–201
Otero JE, Gholson JJ, Pugely AJ, Gao Y, Bedard NA, Callaghan JJ (2016) Length of hospitalization after joint arthroplasty: does early discharge affect complications and readmission rates? J Arthroplast 31(12):2714–2725
Den Hartog Y, Mathijssen N, Hannink G, Vehmeijer S (2015) Which patient characteristics influence length of hospital stay after primary total hip arthroplasty in a ‘fast-track’setting? Bone Joint J 97(1):19–23
Kolisek FR, McGrath MS, Jessup NM, Monesmith EA, Mont MA (2009) Comparison of outpatient versus inpatient total knee arthroplasty. Clin Orthop Relat Res 467(6):1438–1442
Gauthier-Kwan OY, Dobransky JS, Dervin GF (2018) Quality of recovery, Postdischarge hospital utilization, and 2-year functional outcomes after an outpatient Total knee arthroplasty program. J Arthroplast 33(7):2159–2164.e2151. https://doi.org/10.1016/j.arth.2018.01.058
Argenson J-NA, Husted H, Lombardi A Jr, Booth RE, Thienpont E (2016) Global forum: an international perspective on outpatient surgical procedures for adult hip and knee reconstruction. JBJS 98(13):e55
Courtney PM, Boniello AJ, Berger RA (2017) Complications following outpatient total joint arthroplasty: an analysis of a national database. J Arthroplast 32(5):1426–1430
Su EP, Perna M, Boettner F, Mayman DJ, Gerlinger T, Barsoum W, Randolph J, Lee G (2012) A prospective, multi-center, randomised trial to evaluate the efficacy of a cryopneumatic device on total knee arthroplasty recovery. J Bone Joint Surg Br 94(11 Suppl a):153–156. https://doi.org/10.1302/0301-620x.94b11.30832
Song MH, Kim BH, Ahn SJ, Yoo SH, Kang SW, Kim YJ, Kim DH (2016) Peri-articular injections of local anaesthesia can replace patient-controlled analgesia after total knee arthroplasty: a randomised controlled study. Int Orthop 40(2):295–299. https://doi.org/10.1007/s00264-015-2940-2
Li D, Yang Z, Xie X, Zhao J, Kang P (2016) Adductor canal block provides better performance after total knee arthroplasty compared with femoral nerve block: a systematic review and meta-analysis. Int Orthop 40(5):925–933. https://doi.org/10.1007/s00264-015-2998-x
Li Z, Cheng W, Sun L, Yao Y, Cao Q, Ye S, Qi L, Xu S, Wu X, Jing J (2018) Mini-subvastus versus medial parapatellar approach for total knee arthroplasty: a prospective randomized controlled study. Int Orthop 42(3):543–549. https://doi.org/10.1007/s00264-017-3703-z
Courtney PM, Melnic CM, Gutsche J, Hume EL, Lee GC (2015) Which patients need critical care intervention after total joint arthroplasty? : A prospective study of factors associated with the need for intensive care following surgery. Bone Joint J 97-B(11):1512–1518. https://doi.org/10.1302/0301-620X.97B11.35813
Sutton JC III, Antoniou J, Epure LM, Huk OL, Zukor DJ, Bergeron SG (2016) Hospital discharge within 2 days following total hip or knee arthroplasty does not increase major-complication and readmission rates. JBJS 98(17):1419–1428
Pulido L, Parvizi J, Macgibeny M, Sharkey PF, Purtill JJ, Rothman RH, Hozack WJ (2008) In hospital complications after total joint arthroplasty. J Arthroplast 23(6):139–145
Edelstein AI, Kwasny MJ, Suleiman LI, Khakhkhar RH, Moore MA, Beal MD, Manning DW (2015) Can the American College of Surgeons risk calculator predict 30-day complications after knee and hip arthroplasty? J Arthroplast 30(9):5–10
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was reviewed and approved by the institutional ethics committee and the authors have no conflicts of interest to disclose.
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Gillis, M.E., Dobransky, J. & Dervin, G.F. Defining growth potential and barriers to same day discharge total knee arthroplasty. International Orthopaedics (SICOT) 43, 1387–1393 (2019). https://doi.org/10.1007/s00264-018-4100-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4100-y