Abstract
Introduction
The primary objective of this study was to assess the incidence of recurrent glenohumeral instability in patients over 40 years with isolated rotator cuff (RC) repair for traumatic shoulder dislocation. The secondary objectives were to identify risk factors for glenohumeral recurrence after RC repair and to describe the causes and incidences of re-intervention.
Materials and methods
In this retrospective cohort study, data of consecutive patients at a single trauma center between January 2014 and July 2019 were reviewed, and 84 patients with a mean age of 57 (range: 40–75) years and follow-up duration of 3.9 (2–6) years were included. The inclusion criteria were as follows: first traumatic anterior shoulder dislocation, reparable RC tear, primary arthroscopic RC repair, no labral or bony Bankart lesion repair, and at least 2 years of follow-up. Patients less than 40 years of age were excluded. Shoulder instability recurrences and surgical reinterventions were reviewed with medical records. Statistical analysis was performed for qualitative variables using the Chi-squared test. Statistical significance was set at P ≤ 0.05.
Results
There was one patient with a redislocation episode (1.2%) at 2.5 years after surgery, who was surgically treated. Age, subscapular tears, bony Bankart injuries, humeral defects, and associated neurological injuries were not risk factors for recurrence in this study. Ten patients (11.9%) required reintervention. Nine patients (10.7%) re-tore their RCs.
Conclusions
Recurrent glenohumeral instability in active patients over 40 years with isolated RC repair after traumatic shoulder dislocation was infrequent, despite the incidence of significant Hill–Sachs defects, anterior glenoid defects, bipolar bone defects, size of the RC injury, and tendon re-tears. The incidence of re-interventions was 11.9%, with symptomatic RC retear as the main cause.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Rotator cuff (RC) tears after a shoulder dislocation are frequent in patients over 40 years of age [1]. The incidence of full-thickness tears increased with age over 40 years, while the risk of a Bankart lesion decreased [2, 3], which might be explained by the reduced tendon elasticity of the RC due to age-related collagen degeneration [4].
Shoulder dislocation and concomitant RC tear may cause loss of function and pain. Redislocation risk should also be a key criterion during the discussion of surgical treatment. It is well-known that redislocation risk after a first-time traumatic dislocation increased in younger patients [5]. The association between age and redislocation was stronger in patients under 40 years of age. However, for older patients, associated injury patterns were primarily relevant. In this regard, concomitant injuries associated with an increased redislocation rate were full-thickness RC tears [6,7,8], particularly complete subscapularis tears [9], anterior glenoid rim fractures [10], and neurologic deficits [6]. While the functional advantages of RC repair are well-known in these cases [10], no standard treatment algorithm could be generated from the current literature regarding the fixation of the capsulolabral complex. Refixation of the capsulolabral complex along with RC repair has been recommended in active patients under 60 years of age [4, 11].
The recurrence rate after isolated arthroscopic soft tissue repair has been described in approximately 18% of patients without a RC tear [12]. On the contrary, the rate of recurrence decreased to 5.7% in patients without a RC tear that underwent open bone reconstruction [12]. However, the incidence of shoulder instability recurrence after isolated RC repair in active patients over 40 years with an anterior traumatic shoulder dislocation remains unknown.
The primary objective of this study was to assess the incidence of recurrent glenohumeral instability in patients over 40 years with isolated RC repair for traumatic shoulder dislocation. The secondary objectives were to identify risk factors for glenohumeral recurrence after RC repair and to describe the causes and incidences of re-intervention. We hypothesized that isolated RC repair after a traumatic shoulder dislocation would prevent future instability recurrence.
Materials and methods
Patients
In this observational retrospective cohort study, we reviewed medical records of all patients who underwent RC repair surgery between 2014 and 2019 in a single trauma center database. All included patients were admitted due to occupational accidents and were treated under our national workers’ accident insurance law. The inclusion criteria were as follows: (1) presence of first traumatic anterior shoulder dislocation; (2) presence of preoperative evaluation as a repairable RC tear; (3) presence of a primary arthroscopic RC repair; (4) absence of a labral or bony Bankart repair; (5) presence of at least 2 years of follow-up. We excluded patients younger than 40 years of age, patients with prior shoulder surgery, concomitant proximal humerus fractures, and anterior glenoid fractures with fragments greater than 20% of the glenoid surface area. The evaluation and approval of the hospital ethics committee on which none of the authors of the investigation participated, was requested.
Surgical intervention and follow-up
After the initial trauma, all patients were treated in the emergency department during the same day. All patients had a shoulder reduction under conscious sedation and were referred to the shoulder department for outpatient follow-up. Shoulder radiographs were obtained before and after close reduction.
Further imaging studies included magnetic resonance imaging (MRI) for RC injuries, which were suspected in patients, who, upon their first visit to the shoulder specialist, experienced persistent pain at 90º of elevation or exhibited positive Jobe’s sign, belly press, lag signs, pseudoparesia, or pseudoparalysis [13, 14]. A computed tomography (CT) scan was performed in patients with bony Bankart injury observed on shoulder radiographs. Patients with bony fragments greater than 20% of the glenoid surface area were treated with bone fixation and excluded from this study. Neurological lesions were suspected during physical examination if any sensory or motor deficits of the brachial plexus terminal branches were observed. All patients with suspected nerve injury were examined using electromyography (EMG) between the fourth and sixth weeks after the initial injury.
A team of five shoulder surgeons performed all arthroscopic RC surgeries using suture anchors. Each surgeon decided the specific suture anchor configuration during surgery. A single row technique was performed in 79.7% and a double-row transosseous equivalent repair was used in 20.3% of the cases. The mean number of anchors used was 2.3 (range: 1–4). Biceps tenotomy or tenodesis was performed in 85.7% of the patients. No capsulolabral or bony Bankart repair was performed as an associated procedure in the included patients.
At the end of the surgery, the following variables were recorded: sex, age, type of RC injury, and surgical technique. According to the International Society of Arthroscopy, Knee Surgery, and Orthopedic Sports Medicine consensus [15], RC injuries were classified based on the size and retraction, according to Snyder [16] and Patte [17], respectively. The Goutallier [18, 19] classification was used for fatty degeneration. Subscapular injuries were classified according to Lafosse et al. [20], and nerve injuries based on the initial EMG findings were described and classified according to Seddon [21]. Bone defects were measured using an anteroposterior X-ray after shoulder reduction with the patient’s shoulder internally rotated and in a brace. Hill–Sachs lesions were considered significant if the defect/radius ratio was greater than 15% [22], while anterior glenoid bone injury was considered positive in the presence of a bony Bankart lesion or in the absence of the anterior glenoid rim line [23]. The presence of labral injuries was also registered after arthroscopic examination.
All patients were placed in a shoulder immobilization device for the first 3 weeks. Hand and elbow exercises were allowed and encouraged. Passive-assisted mobilization was initiated by a physiotherapist between the third and sixth weeks. The shoulder immobilization device was used until 6 weeks, and active scapular balance exercises were initiated. Strength exercises were performed from the 12th week onward. Additional MRI scans were performed if pain persisted at 90º of elevation or there was a positive Jobe’s sign, belly press, or lag sign, pseudoparesia, or pseudoparalysis at the sixth month of follow-up [13, 14].
Shoulder instability recurrences and surgical reinterventions were reviewed based on the medical records of each patient. Shoulder instability recurrence was defined as any reported episode during follow-up, of subluxation or dislocation who consulted in the emergency department or on an outpatient basis and was validated by a shoulder team specialist.
Statistical analysis
A descriptive analysis of all the variables was conducted. A Chi-squared test was performed to determine associations between known variables and recurrence of dislocation. Statistical significance was set at P ≤ 0.05.
Results
Cohort demographics
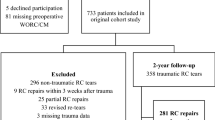
Data from 350 consecutive patients with arthroscopic RC repair were found in our surgical database during the study period. Of these, 106 patients had an isolated RC repair after a traumatic shoulder dislocation. Five patients were younger than 40 years of age, and 17 had less than 2 years of follow-up. There were 84 (24%) patients that fulfilled the inclusion criteria. The average age of the patients was 57 [range: 40–75, standard deviation (SD): 8.8] years, and 51 (60.7%) were men. The dominant arm was affected in 61 patients (73.5%). The average time from injury to surgery was 2.9 (SD: 1.05) months. The mean follow-up period was 3.9 (range: 2–6) years.
Injury description
Of the RC injuries included in this study, 66.2% were isolated tears of the posterosuperior cuff, and 93.1% had a Goutallier score ≤ 2. The incidence of subscapular tendon tears was 33.7%, and 42.3% of the cases were Lafosse type 2. A descriptive analysis of RC injuries is presented in Table 1.
Regarding bone defects, 26.2% had a significant Hill–Sachs lesion, while 14.3% had an absence of the anterior glenoid line or a bony Bankart lesion upon preoperative X-ray examination. A descriptive analysis of bone defects in the different age groups is shown in Table 2. An anteroinferior labral tear was present in 52% of patients between 40 and 65 years of age, and in 38.4% of those older than 65 years of age.
Nerve injuries were found in 30 patients (35.7%). According to EMG findings, isolated damage to the axillary nerve was the most frequent injury (82.9%). According to the Seddon classification [14, 20], 40% [11] of cases had neuropraxia and 60% [17] had axonotmesis. All neurological injuries were post-ganglionic and were initially managed without surgery. All nerve injuries showed at least partial recovery on sensory and motor clinical examination during follow-up without the need of further surgical treatment.
Outcome measures
Ten patients (11.9%) underwent reintervention. Nine patients (10.7%) had a RC re-tear. The mean time from initial trauma to surgery in patients who had a re-tear was 2.2 (SD: 0.4) months, the mean age of these patients was 55 (SD: 8.85) years. These re-tear patients initially had a repaired posterosuperior RC tear and three associated repaired subscapular tendon tears [12]. The posterosuperior extension was C4 [9] in six patients, and retraction was Patte 3 in four patients [24]. Six patients underwent re-operation with a new RC repair, while three underwent surgery for a reverse shoulder arthroplasty.
Only one patient (1.2%), who was a horse breaker, experienced instability recurrence during follow-up. The patient experienced new trauma on his shoulder due to falling off during horse riding, which occurred 2.5 years after the surgery. Upon initial trauma, he was 58 years, injured his non-dominant arm, had a C1 posterosuperior RC tear, a significant Hill–Sachs lesion, and no bone injury at the anterior glenoid. MRI after recurrence did not show a tendon re-tear. He was treated surgically with arthroscopic capsulolabral fixation, and a Remplisagge was added to fill the humeral bone defect [23]. Postoperatively, he was able to return to his occupational duties. He completed 3 years of follow-up after recurrence, with no further shoulder dislocation or subluxation.
Discussion
The main objective of this study was to describe the incidence of recurrent glenohumeral instability in patients 40 years and over, who underwent isolated RC repair after a traumatic shoulder dislocation. Shoulder stability was restored in all but one patient, and the main cause of reintervention was RC re-tear.
A traumatic shoulder dislocation can cause a RC injury, which may be previously weakened by repetitive microtrauma in younger athletes or from physiologic degeneration as a person ages [10]. The risk of a full-thickness RC tear after shoulder dislocation significantly increased with increasing age, with an incidence as high as 70% in patients aged over 60 years [1,2,3]. Risk factors for recurrence have been described. A full-thickness tear of the RC increased the relative risk of re-dislocation by 30% [6]. Walch et al. Found that 77% of patients ≥ 40 years of age, who presented with a recurrent dislocation, had prior RC tears [8]. Furthermore, Porcellini et al. revealed a strong correlation between the number of dislocations and full-thickness posterosuperior tendon tears [7].
Persistent pain and weakness 2–3 weeks after a traumatic anterior shoulder dislocation should prompt further RC evaluation with imaging techniques, such as MRI [10]. Early diagnosis of RC pathology is important for faster functional restoration and better outcomes in these patients. The literature has also addressed whether operative or non-operative treatment is more likely to result in a painless, functional shoulder. In symptomatic patients, surgery is more likely to improve function, result in less pain, decreased recurrence, and higher patient satisfaction than non-operative treatment [2, 25, 26].
At the time of surgery, RC repair with or without a capsulolabral or bony Bankart repair, if present, must be decided. Bone defects should also be considered. Several factors might affect the decisions of the physicians. Combined RC repair and stabilization surgery has been recommended for patients with either chronic instability or those aged < 60 years [4]. Like younger patients, some patients older than 40 years of age might have an anterior capsulolabral detachment as a cause of an anterior shoulder dislocation [27]. In these patients, anterior stabilization and RC repair have been advocated to improve function and restore stability [7, 28,29,30].
In our study, an active population aged between 40 and 75 years of age was included, with 64.3% of these patients under the age of 60 years. A recurrent dislocation occurred only in one patient, who fell while riding a horse during his duties as a horse-breaker. Due to its mechanism, whether this event resulted from treatment complication or represented an independent new complication remained debatable. Although almost half of the patients had an anteroinferior labral lesion, there was no increase in the incidence of recurrences in this group compared to those without labral lesions, regardless of age.
Theoretically, repairing the concavity compression of the RC will restore shoulder stability in these patients. Several factors might have contributed to our results. First, all patients underwent a strict follow-up that allowed early diagnosis of symptomatic RC pathology and surgical treatment to prevent the development of recurrent dislocation and further articular damage. Second, patients over 40 years were associated with a lower rate of recurrent dislocation in the absence of a RC injury [6].
Although shoulder stability might be restored with an isolated RC repair, whether labral or bony Bankart injuries as a concomitant procedure would further increase functional results compared to isolated RC repairs remained unknown. Porcellini et al. repaired both capsular and RC lesions in a series of 50 patients, whose postoperative outcomes improved significantly [7]. Shields et al. reported a case series of 13 patients who underwent arthroscopic simultaneous RC repair and Bankart repair with a minimum of 2 years of follow-up. At the final follow-up, the affected extremity had similar ASES shoulder score and Constant scores compared to the noninjured, asymptomatic side [31]. Gomes et al. analyzed 33 patients that underwent arthroscopic repair of complete RC tears associated with a traumatic anterior dislocation and classified them into patients with fixed Bankart lesions or those without a Bankart lesion. The postoperative UCLA score of the group with a Bankart injury repair was 33.96%, while the score of the group without Bankart injury was 33.7% (P = 0.743) [32]. Ro et al. reported a case series of 50 patients aged over 40 years, who were treated with arthroscopic capsulolabral repair (only 4 with concomitant RC repair) for chronic anterior shoulder instability. These patients reportedly showed significant improvement in clinical outcomes. However, their range of motion (ROM) decreased at the final follow-up in terms of forward flexion, external rotation at the side, internal rotation to posterior, and cross-body adduction [33]. Xiaoxi et al. described a cohort of 11 patients who underwent RC repair with an intact glenoid labrum after an anterior shoulder dislocation. No patients in this study had recurrent dislocations after RC repair, with improved functional outcome scores and ROM at a mean follow-up of 26.0 ± 10.7 months [34]. According to our study, there was no increased risk of redislocation in patients with an unfix labral or bony Bankart injury compared to patients with no capsulolabral injury. The requirement for capsulolabral repair to improve functional outcomes must be further analyzed. Future studies should include patients with a RC repair associated with Bankart repair and a control group of unfixed Bankart injuries.
Of the 10 patients who required re-intervention, 9 were due to a RC re-tear. Since only symptomatic patients were studied using MRI during follow-up after surgery, the actual incidence of RC tears might be underestimated. While tendon re-tears might be a risk factor for recurrent shoulder dislocation, none of our patients presented with recurrent shoulder dislocation associated with a tendon re-tear.
The main limitation of this study was its retrospective design and the lack of a control group. Other limitations included a heterogeneous patient cohort, small sample size, selection biases, involvement of multiple surgeons in the treatment of these patients and no functional scores were reported. In addition, all patients in our series were under a workers’ compensation insurance law, which has been described as a prognostic factor or poorer results in RC repairs [35]. Larger comparative well-controlled studies should be conducted in the future to evaluate functional and prognostic results in the treatment of patients with traumatic anterior dislocation and RC repair.
Conclusions
The incidence of recurrent glenohumeral instability in active patients over 40 years of age with isolated RC repair after traumatic shoulder dislocation was infrequent, despite the incidence of significant Hill–Sachs defects, anterior glenoid defects, bipolar bone defects, size of the RC injury, and tendon re-tears. The incidence of re-interventions was 11.9%, with symptomatic RC retear as the main cause.
References
Hawkins RJ, Bell RH, Hawkins RH, Koppert GJ (1986) Anterior dislocation of the shoulder in the older patient. Clin Orthop Relat Res 206(206):192–195. https://doi.org/10.1097/00003086-198605000-00033
Simank HG, Dauer G, Schneider S, Loew M (2006) Incidence of rotator cuff tears in shoulder dislocations and results of therapy in older patients. Arch Orthop Trauma Surg 126(4):235–240. https://doi.org/10.1007/s00402-005-0034-0
Loew M, Thomsen M, Rickert M, Simank HG (2001) Injury pattern in shoulder dislocation in the elderly patient. Unfallchirurg 104(2):115–118. https://doi.org/10.1007/s001130050700
Wellmann M, Habermeyer P (2012) Recognition and management of combined instability and rotator cuff tears. Shoulder instability: a comprehensive approach. Saunders, Philadelphia, pp 466–474
Hovelius L, Rahme H (2016) Primary anterior dislocation of the shoulder: long-term prognosis at the age of 40 years or younger. Knee Surg Sports Traumatol Arthrosc 24(2):330–342. https://doi.org/10.1007/s00167-015-3980-2
Robinson CM, Kelly M, Wakefield AE (2002) Redislocation of the shoulder during the first six weeks after a primary anterior dislocation: risk factors and results of treatment. J Bone Jt Surg Am 84(9):1552–1559. https://doi.org/10.2106/00004623-200209000-00007
Porcellini G, Paladini P, Campi F, Paganelli M (2006) Shoulder instability and related rotator cuff tears: arthroscopic findings and treatment in patients aged 40 to 60 years. Arthroscopy 22(3):270–276. https://doi.org/10.1016/j.arthro.2005.12.015
Walch G et al (1997) Rotator cuff tears associated with anterior instability. Complex and revision problems in shoulder surgery. Lippincott-Raven, Philadelphia, pp 65–70
Neviaser RJ, Neviaser TJ, Neviaser JS (1993) Anterior dislocation of the shoulder and rotator cuff rupture. Clin Orthop Relat Res 291(291):103–106. https://doi.org/10.1097/00003086-199306000-00012
Gombera MM, Sekiya JK (2014) Rotator cuff tear and glenohumeral instability: a systematic review. Clin Orthop Relat Res 472(8):2448–2456. https://doi.org/10.1007/s11999-013-3290-2
Voigt C, Lill H (2009) Schulterinstabilität Rotatorenmanschettenruptur. Orthopadie 38(1):70–74
Williams HLM, Evans JP, Furness ND, Smith CD (2019) It’s not all about redislocation: a systematic review of complications after anterior shoulder stabilization surgery. Am J Sports Med 47(13):3277–3283. https://doi.org/10.1177/0363546518810711
Tennent TD, Beach WR, Meyers JF (2003) A review of the special tests associated with shoulder examination. Part I: The rotator cuff tests. Am J Sports Med 31(1):154–160. https://doi.org/10.1177/03635465030310011101
Tokish JM, Alexander TC, Kissenberth MJ, Hawkins RJ (2017) Pseudoparalysis: a systematic review of term definitions, treatment approaches, and outcomes of management techniques. J Shoulder Elbow Surg 26(6):e177–e187. https://doi.org/10.1016/j.jse.2017.02.024
Calvo and the ISAKOS upper Extremit E (2013) ISAKOS classification system for rotator cuff tears. In: Arce G, Bak K, Shea KP, Savoie F III, Kibler WB, Itoi E (eds) Shoulder concepts 2013: consensus and concerns. Internet. Springer, Berlin. https://doi.org/10.1007/978-3-642-38097-6_3
Patte D (1990) Classification of rotator cuff lesions. Clin Orthop Relat Res 254(254):81–86. https://doi.org/10.1097/00003086-199005000-00012
Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC (1994) Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res 304(304):78–83
Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C (1999) Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg 8(6):599–605. https://doi.org/10.1016/s1058-2746(99)90097-6
Lafosse L, Jost B, Reiland Y, Audebert S, Toussaint B, Gobezie R (2007) Structural integrity and clinical outcomes after arthroscopic repair of isolated subscapularis tears. J Bone Jt Surg Am 89(6):1184–1193. https://doi.org/10.2106/JBJS.F.00007
Seddon HJ (1943) Three types of nerve injury. Brain 66(4):237–288. https://doi.org/10.1093/brain/66.4.237
Hardy P, Lopes R, Bauer T, Conso C, Gaudin P, Sanghavi S (2012) New quantitative measurement of the Hill-Sachs lesion: a prognostic factor for clinical results of arthroscopic glenohumeral stabilization. Eur J Orthop Surg Traumatol 22(7):541–547. https://doi.org/10.1007/s00590-011-0883-x
Charousset C, Beauthier V, Bellaïche L, Guillin R, Brassart N, Thomazeau H, French Arthroscopy Society (2010) Can we improve radiological analysis of osseous lesions in chronic anterior shoulder instability? Orthop Traumatol Surg Res 96(8):S88-93. https://doi.org/10.1016/j.otsr.2010.09.006
Koo SS, Burkhart SS, Ochoa E (2009) Arthroscopic double-pulley remplissage technique for engaging Hill-Sachs lesions in anterior shoulder instability repairs. Arthroscopy 25(11):1343–1348. https://doi.org/10.1016/j.arthro.2009.06.011
Jouve F, Graveleau N, Nové-Josserand L, Walch G (2008) Luxation récidivante antérieure de l’épaule et rupture de la coiffe des rotateurs: résultats du traitement chirurgical. Rev Chir Orthop Réparatrice Appar Mot 94(7):659–669. https://doi.org/10.1016/j.rco.2008.03.032
Pevny T, Hunter RE, Freeman JR (1998) Primary traumatic anterior shoulder dislocation in patients 40 years of age and older. Arthroscopy 14(3):289–294. https://doi.org/10.1016/s0749-8063(98)70145-8
Sonnabend DH (1994) Treatment of primary anterior shoulder dislocation in patients older than 40 years of age. Conservative versus operative. Clin Orthop Relat Res 304(304):74–77
Araghi A, Prasarn M, St Clair S, Zuckerman JD (2005) Recurrent anterior glenohumeral instability with onset after forty years of age: the role of the anterior mechanism. Bull Hosp Jt Dis NY 62(3–4):99–101
Goldberg JA, Chan KY, Best JP, Bruce WJ, Walsh W, Parry W (2003) Surgical management of large rotator cuff tears combined with instability in elite rugby football players. Br J Sports Med 37(2):179–181. https://doi.org/10.1136/bjsm.37.2.179 (discussion 181)
Hawkins RJ, Morin WD, Bonutti PM (1999) Surgical treatment of full-thickness rotator cuff tears in patients 40 years of age or younger. J Shoulder Elbow Surg 8(3):259–265. https://doi.org/10.1016/s1058-2746(99)90139-8
Voos JE, Pearle AD, Mattern CJ, Cordasco FA, Allen AA, Warren RF (2007) Outcomes of combined arthroscopic rotator cuff and labral repair. Am J Sports Med 35(7):1174–1179. https://doi.org/10.1177/0363546507300062
Shields E, Mirabelli M, Amsdell S, Thorsness R, Goldblatt J, Maloney M, Voloshin I (2014) Functional and imaging outcomes of arthroscopic simultaneous rotator cuff repair and bankart repair after shoulder dislocations. Am J Sports Med 42(11):2614–2620. https://doi.org/10.1177/0363546514550993
Godinho GG, Freitas JMA, de Oliveira FF, Santos FML, de Simoni LF, Godinho PC (2016) Evaluation of functional results from shoulders after arthroscopic repair of complete rotator cuff tears associated with traumatic anterior dislocation. Rev Bras Ortop Engl Ed 51(2):163–168
Ro K, Kim MS, Kim JD, Rhee YG (2019) Arthroscopic findings and clinical outcomes in patients 40 years of age and older with recurrent shoulder dislocation. Arthroscopy 35(2):314–322. https://doi.org/10.1016/j.arthro.2018.08.041
Ji X, Ye L, Hua Y, Zhou X (2020) Rotator cuff repair improves clinical function and stability in patients older than 50 years with anterior shoulder dislocations and massive rotator cuff tears. Orthop J Sports Med. https://doi.org/10.1177/2325967120969213
Kemp KAR, Sheps DM, Luciak-Corea C, Styles-Tripp F, Buckingham J, Beaupre LA (2011) Systematic review of rotator cuff tears in workers’ compensation patients. Occup Med (Lond) 61(8):556–562. https://doi.org/10.1093/occmed/kqr068
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The evaluation and approval of the hospital ethics committee on which none of the authors of the investigation participated, was requested.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Marsalli, M., Errázuriz, J., Morán, N.I. et al. Recurrence of glenohumeral instability in patients with isolated rotator cuff repair after a traumatic shoulder dislocation. Arch Orthop Trauma Surg 143, 3857–3862 (2023). https://doi.org/10.1007/s00402-022-04628-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04628-6