Abstract
Purpose
The complex and dynamic spinopelvic interplay is not well understood. The aims of the present study were to investigate the following: (1) whether native acetabular anteinclination (AI) in standing position changes following lumbar spinal fusion (LSF); (2) potential correlations between AI change (ΔAI) and several spinopelvic parameters such as the change in lumbar lordosis (ΔLL), pelvic tilt (ΔPT), and anterior pelvic plane angle (ΔaPP).
Methods
A total of 485 patients (Males: 262, Females: 223) with an average age of 64 ± 13 years who underwent a primary LSF were identified from our institutional database. The difference (Δ) between pre-and postoperative acetabular anteinclination (AI), lumbar lordosis (LL), anterior pelvic plane angle (aPP), sacral slope (SS), and pelvic tilt (PT) were measured on a standing lateral radiograph (EOS®) and compared to find the effect of LSF on the lumbopelvic geometry.
Results
Following LSF, the average absolute ΔAI was 5.4 ± 4 (0 to 26)°, ΔLL: 5.5 ± 4 (0 to 27)°, ΔaPP: 5.4 ± 4 (0 to 38)°, ΔPT: 7 ± 5 (0 to 33)° and ΔSS: 5.3 ± 4 (0 to 33)°. No significant differences were observed between LSF levels. A ΔAI ≥ 10° was observed in 66 (13.6%) and ΔAI ≥ 20° in 5 (1%) patients. The Pearson correlation demonstrated a strong negative correlation of ΔAI with ΔLL (r = 0.72, p < .001).
Conclusion
Clinical decision-making should consider the relationship between native anteinclination and lumbar lordosis to reduce the risk of functional acetabular component malalignment in patients with concomitant hip and spine pathology.
Level of evidence
Retrospective case–control study, Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There has been an increasing interest in the dynamic interplay between the spine, hip, and pelvis, especially in the setting of lumbar spinal fusion (LSF) and total hip arthroplasty (THA). Lumbar spine alignment can affect the pelvic position, which in turn influences the functional acetabular orientation [4, 9]. Under physiological conditions, during the transition from the standing to sitting position, the pelvis tilts posteriorly, thus increasing the acetabular anteversion to provide increased clearance for the femur to flex [8, 15]. However, following LSF, abnormal spinopelvic mechanics and pelvic hypermobility (> 30° change in pelvic tilt between standing and sitting) have been reported [5], which might become relevant in the setting of total hip arthroplasty (THA).
Current literature supports that patients with a concomitant THA and LSF might present a significantly higher dislocation rate compared to THA patients without LSF [1, 6, 16,17,18,19] due to a decreased acetabular opening angle and functional arc of motion before impingement [10]. Furthermore, in patients with a sagittal imbalance, the abnormal position of the pelvis might lead to a functional malpositioning of the acetabular component, even if the component is positioned correctly within the pelvis [15]. Therefore, it is recommended that in patients with a previous LSF, the acetabular component orientation should be adjusted to account for the position and the stiffness of the lumbar spine [7, 14]. Nevertheless, the degree of acetabular adjustment remains undefined, as the change of acetabular orientation before and following the LSF has never been reported in the literature. The sagittal acetabular component position measured on lateral spinopelvic-hip radiographs is defined as anteinclination (AI) and represents a combination of both the anteversion and inclination of the acetabulum [15].
Therefore, the purpose of the present study was to identify: (1) whether native acetabular AI changes following LSF; (2) the potential correlations between AI change and several spinopelvic parameters such as the change in lumbar lordosis, pelvic tilt, anterior pelvic plane angle and sacral slope, demographics (age, gender, BMI) and the level or the number of levels fused.
Material and methods
Study design, inclusion, and exclusion criteria
The present study was approved by the state ethical committee and was entirely conducted at the authors’ institution. The inclusion criteria were patients older than 18 years, who underwent a primary LSF with good-quality (entire spine was visible and the greater sciatic notches and anterior superior iliac spines were superimposed) pre-and postoperative standing lateral radiographs (EOS®). The indication for LSF was degenerative spinal canal stenosis with severe back pain, refractory to conservative treatments. Exclusion criteria were any history of lumbar spine fracture or infection, inflammatory spinal diseases such as ankylosing spondylitis, previous total hip arthroplasty, and neurologic or musculoskeletal disorders, which could impact motion or muscle tone.
Patient characteristics
Between January 2018 to December 2020, a total of 485 patients (Males: 262, Females: 223) with an average age of 64 ± 13 (20–89) years underwent a LSF at our institution and met the inclusion and exclusion criteria (Table 1). One-level LSF was performed in 270 (55.6%), a two-level LSF in 115 (23.7%), whereas a multi-level LSF (≥ 3 levels) in 100 (20.5%) patients (Table 1).
Radiologic measurements
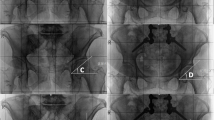
All parameters of interest were measured on preoperative (within 2 months before LSF) and postoperative (1 year following LSF) standing lateral radiographs (EOS®) by two orthopedic residents (D.D, S.H). Lumbar lordosis (LL), was defined as the angle formed by the line tangent to the superior endplate of L1 and the line tangent to the superior endplate of S1 for each film (Fig. 1). The anterior pelvic plane (aPP) was defined as the angle between the plane created by the bilateral anterior superior iliac spine to the pubic symphysis and the coronal vertical plane (Fig. 1) [3]. The pelvic tilt (PT) was defined as the angle formed by the sacral endplate midpoint to the center of the bifemoral heads and the vertical axis (Fig. 1), whereas the sacral slope (SS) as the angle formed by the line tangent to the superior endplate of S1 and the horizontal (Fig. 1). The pelvic incidence (PI) was defined as the angle between the line perpendicular to the sacral plate at its midpoint and the line connecting this point to the femoral head axis [11]. Finally, the acetabular anteinclination (AI) was determined by the line connecting the superior and inferior acetabular wall on the right side to the horizontal axis (Fig. 1) [2].
An example of pre-and postoperative standing lateral radiographs (EOS®) of a patient who underwent a LSF at the level L5/S1. For illustration purposes, the thoracic spine is not demonstrated. The acetabular anteinclination (blue lines) was measured on the pre-and postoperative radiographs. The sacral slope (green lines) and anterior pelvic plane (orange lines) are demonstrated in the preoperative radiograph, whereas the lumbar lordosis (purple lines) and pelvic tilt (red lines) are shown on the postoperative radiograph for the simplicity of the figures
Repeatability analysis
The radiographs of 100 randomly selected patients were reevaluated by two orthopedic residents (D.D, S.W) blinded to the patient’s clinical details. Then each observer reassessed all the radiographs after a 4 week interval to avoid recall bias. The observers measured all the radiographic spinopelvic parameters. The intraobserver and interobserver reliabilities of the measurements were evaluated using a single-measure intraclass correlation coefficient (ICC) with a two-way random-effects model for absolute agreement.
Subgroup analysis
The patients were divided into two groups according to the difference in AI (ΔAI ≥ 10° and ΔAI < 10°) to identify potential differences in demographics and surgical parameters between groups.
Statistical analysis
Descriptive statistics used mean, standard deviation, range, and percentages to present the data. The changes in the radiologic parameters following LSF were presented in absolute values. All parameters were tested with the Kolmogorov–Smirnov test for normality. When the criteria for normality were met, a two-tailed paired t test was used. Otherwise, the Wilcoxon signed-rank test was applied. The analysis of variance (ANOVA) was used to compare the ΔAI between the fused levels (both between specific levels fused and multiple levels). The Pearson correlation and multiple linear regression analysis were performed to evaluate whether the ΔAI correlated with the other spinopelvic parameters, patient demographics, and the level or the number of levels fused. The chi-square test was used to compare categorical data. The level of significance was set to p ≤ 0.05. All the statistical analyses were performed using SPSS version 23 software (SPSS Inc., Chicago, IL).
Results
Intraobserver and interobserver reliability
The intraobserver and interobserver reliability was in excellent agreement (≥ 80%) for all the radiographic parameters (Table 2).
Radiographic parameters
The mean preoperative AI (34 ± 10°), LL (43.5 ± 14°), aPP (2.9 ± 10°), SS (35.8 ± 10°), PT (15.7 ± 14°), and PI (59.2 ± 13°) demonstrated no significant differences following LSF (Table 2).
Following LSF, the average absolute ΔAI was 5.4 ± 4 (0–26)°, ΔLL: 5.5 ± 4 (0–27)°, ΔaPP: 5.3 ± 5.8 (0–38) °, ΔPT: 7 ± 5 (0–33)° and ΔSS: 5.3 ± 4 (0–33)° (Table 2). A ΔAI ≥ 10° was observed in 66 (13.6%) and ΔAI ≥ 20° in 5 (1%) patients. No significant differences in the ΔAI were observed between the level fused (Fig. 2).
The Pearson correlation demonstrated a strong negative correlation of ΔAI with the ΔLL (r = − 0.72, p < 0.001). Other spinopelvic parameters, the level or the number of levels fused, as well as the involvement of the sacrum in the LSF, did not correlate with a ΔAI.
A subgroup analysis demonstrated that patients with a ΔAI ≥ 10° had no significant differences compared to patients with ΔAI < 10° following LSF in demographics, the involvement of sacrum in the LSF, or the number of multi-level fusion (Table 3).
Discussion
The complex and dynamic interplay between the spine, hip, and pelvis is not well understood. A potential change of native AI following LSF could result in the much-debated change in risk for THA instability. The main purpose of the present study was to investigate whether the native AI changes following LSF and to identify potential correlations between the ΔAI and several spinopelvic and demographic parameters. Following LSF, the average absolute ΔAI was 5.4 ± 4, whereas a ΔAI ≥ 10° was observed in 13.6% of the patients. The ΔAI correlated strongly with the ΔLL (r = 0.72, p < 0.001).
To the current date, only a few studies have investigated the functional acetabular orientation following LSF. In a retrospective radiological study, Bernstein et al. [2] analyzed 50 patients with LSF and 100 patients with low back pain and reported an average change in acetabular anteversion between flexion and extension of the lumbar spine of 21° and 15° in patients without and with a LSF, respectively. In patients with a LSF involving the sacrum, the average change in acetabular anteversion from flexion to extension was 10°. Similarly, Lazennec et al. [10] reported an average change in acetabular anteversion of 7.1° between sitting and standing in the 93 THA patients with LSF and 12.1° in the control group of 150 THA patients without LSF. Park et al. [13] reported an average decrease of about 5–10° in PT and 3–5° in LL with unchanged PI in 104 patients with degenerative lumbar spine disease from standing to supine. Although these studies contributed significantly to the understanding of dynamic spinopelvic mobility during functional activities, they did not report the effect of LSF on spinopelvic parameters in an intrasubject-specific manner. The present study compared the change of several spinopelvic parameters following LSF in the same individual and reported an average change of 5.4 (0–26)° in AI, with 13.6% of the patients demonstrating a change of ≥ 10°. These results suggest that the native acetabular AI could change following a LSF, implying that both hip and spine surgeons should be aware of these changes when planning THA in patients with previous LSF or vice versa.
Spinopelvic relationships and their impact on the functional THA acetabular component orientation remains a continued area of interest, especially in an attempt to predict the ideal patient-specific acetabular safe zones based on preoperative functional imaging. Buckland et al. [4] demonstrated in a prospective, multicenter study with 33 patients (41 THA) who underwent a spinal realignment procedure, that a mean ΔAI of 5° and high correlation of ΔAI with the ΔPT (r = 0.83, p < 0.05), ΔSS (r = − 0.76, p < 0.05) and ΔLL (r = − 0.69, p < 0.05). Nevertheless, in a prospective radiological analysis of 24 patients without a LSF and 27 with a previous LSF undergoing a THA, Nam et al. [12] reported high intrasubject variability in pelvic motion and functional component orientation following THA. Haffer et al. [6] in a prospective study of 197 THA patients demonstrated a significant difference in cup anteversion between between siiting and standing of an average (stiff/neutral/hypermobile 6° for stiff, 12° for neutral ans 20° for hepermobile patients. The present radiological analysis of 485 patients, who underwent LSF, demonstrated that the native ΔAI following LSF correlated strongly with the ΔLL (r = 0.72, p < 0.001) only. Other spinopelvic parameters, the level or the number of levels fused, as well as the involvement of the sacrum in the LSF, did not correlate with a ΔAI.
The present study should be interpreted in light of its potential limitations. The most obvious drawback was the retrospective study design. However, due to the standardized clinical and radiological follow-up protocol and the excellent documentation in a university hospital setting, the necessary patient data were available for full analysis. Furthermore, the manual measuring on standing lateral radiograph images could lead to errors in the studied parameters. Nevertheless, a standardized measurement technique was applied and multiple independent measurements were performed by two observers, showing excellent intra- and interobserver reliabilities, suggesting that the results were valid, accurate, and reproducible. Moreover, the sample size was quite heterogenous as patients with LSF at several levels were included. A subgroup analysis was however performed to analyze the effect of different fusion levels on the ΔAI. Finally, all the patients in the present study underwent LSF for lumbar spinal stenosis and therefore might have different changes in acetabular AI than patients who underwent LSF for other pathologies such as scoliosis, kyphosis, or high-grade isthmic spondylolisthesis.
In conclusion, the current study investigated the effect of LSF on the native AI in 485 patients in a standing position and demonstrated that the AI changes at an average of 5.4 ± 4° following LSF, with 13.6% of the patients demonstrating a ΔAI ≥ 10°. The ΔAI correlated strongly with the ΔLL (r = 0.72, p < 0.001). These results suggest that the native acetabular AI could change following a LSF, implying that clinical decision-making should consider the relationship between native acetabular anteinclination and lumbar lordosis to reduce the risk of functional acetabular component malalignment in THA patients undergoing a LSF or vice versa.
Availability of data and materials
The materials described in the manuscript, including all relevant raw data, will be freely available to any researcher wishing to use them for non-commercial purposes, without breaching participant confidentiality.
References
Barry JJ, Sing DC, Vail TP, Hansen EN (2017) Early outcomes of primary total hip arthroplasty after prior lumbar spinal fusion. J Arthroplasty 32(2):470–474
Bernstein J, Charette R, Sloan M, Lee GC (2019) Spinal fusion is associated with changes in acetabular orientation and reductions in pelvic mobility. Clin Orthop Relat Res 477(2):324–330
Buckland A, DelSole E, George S et al (2013) Sagittal pelvic orientation a comparison of two methods of measurement. Bull Hosp Jt Dis 75(4):234–240
Buckland AJ, Vigdorchik J, Schwab FJ et al (2015) Acetabular anteversion changes due to spinal deformity correction: bridging the gap between hip and spine surgeons. J Bone Joint Surg Am 97(23):1913–1920
Grammatopoulos G, Gofton W, Jibri Z et al (2019) 2018 Frank Stinchfield award: spinopelvic hypermobility is associated with an inferior outcome after THA: examining the effect of spinal arthrodesis. Clin Orthop Relat Res 477(2):310–321
Haffer H, Wang Z, Hu Z, Hipfl C, Pumberger M (2021) Acetabular cup position differs in spinopelvic mobility types: a prospective observational study of primary total hip arthroplasty patients. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-04196-1
Ike H, Dorr LD, Trasolini N, Stefl M, McKnight B, Heckmann N (2018) Spine-pelvis-hip relationship in the functioning of a total hip replacement. J Bone Joint Surg Am 100(18):1606–1615
Lazennec JY, Boyer P, Gorin M, Catonne Y, Rousseau MA (2011) Acetabular anteversion with CT in supine, simulated standing, and sitting positions in a THA patient population. Clin Orthop Relat Res 469(4):1103–1109
Lazennec JY, Brusson A, Rousseau MA (2011) Hip-spine relations and sagittal balance clinical consequences. Eur Spine J 20(Suppl 5):686–698
Lazennec JY, Clark IC, Folinais D, Tahar IN, Pour AE (2017) What is the impact of a spinal fusion on acetabular implant orientation in functional standing and sitting positions? J Arthroplasty 32(10):3184–3190
Le Huec JC, Aunoble S, Philippe L, Nicolas P (2011) Pelvic parameters: origin and significance. Eur Spine J 20(Suppl 5):564–571
Nam D, Riegler V, Clohisy JC, Nunley RM, Barrack RL (2017) The impact of total hip arthroplasty on pelvic motion and functional component position is highly variable. J Arthroplasty 32(4):1200–1205
Park SA, Kwak DS, Cho HJ, Min DU (2017) Changes of spinopelvic parameters in different positions. Arch Orthop Trauma Surg 137(9):1223–1232
Phan D, Bederman SS, Schwarzkopf R (2015) The influence of sagittal spinal deformity on anteversion of the acetabular component in total hip arthroplasty. Bone Joint J 97(8):1017–1023
Ranawat CS, Ranawat AS, Lipman JD, White PB, Meftah M (2016) Effect of spinal deformity on pelvic orientation from standing to sitting position. J Arthroplasty 31(6):1222–1227
Salib CG, Reina N, Perry KI, Taunton MJ, Berry DJ, Abdel MP (2019) Lumbar fusion involving the sacrum increases dislocation risk in primary total hip arthroplasty. Bone Joint J 101(2):198–206
Schmidt-Braekling T, Coyle MJ, Dobransky J et al (2021) Spinal pathology and outcome post-THA: does segment of arthrodesis matter? Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-04220-4
Sing DC, Barry JJ, Aguilar TU et al (2016) Prior lumbar spinal arthrodesis increases risk of prosthetic-related complication in total hip arthroplasty. J Arthroplasty 31(9):227-232e221
Yang DS, Li NY, Mariorenzi MC, Kleinhenz DT, Cohen EM, Daniels AH (2020) Surgical treatment of patients with dual hip and spinal degenerative disease: effect of surgical sequence of spinal fusion and total hip arthroplasty on postoperative complications. Spine (Phila Pa 1976) 45(10):E587–E593
Funding
No funding was received for this work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by [DD], [SH], [EW] and [SW]. The first draft of the manuscript was written by [DD] and a major revision was performed by [MB] and [MF]. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors of this manuscript have nothing to disclose that would bias the content of the manuscript.
Ethical approval
Kantonale Ethikkommission Zürich, BASEC Nr.: 2021-00084.
Consent to participate
The authors give their consent for participation
Consent for publication
The authors give the journal consent for publication
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dimitriou, D., Haupt, S., Weber, S. et al. The effect of lumbar spinal fusion on native acetabular anteinclination in standing position. Arch Orthop Trauma Surg 143, 2733–2738 (2023). https://doi.org/10.1007/s00402-022-04531-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04531-0