Abstract
Background
Deep infection following arthroplasty remains a devastating complication. Some registry data suggests that modern positive-pressure surgical helmet systems (SHS) are associated with a paradoxical increase in infection rates, and as such their role in arthroplasty remains unclear. The aim of this study was to investigate whether SHS increase wound contamination in total knee arthroplasty (TKA) and if this contamination can be reduced by placing tape around the gown/glove interface.
Methods
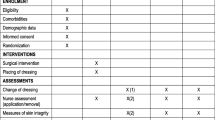
Seventy-five patients were randomised into three groups: scrubbed theatre staff wore standard surgical gowns (SG), SHS without tape at the gown/glove interface, or SHS with tape. All TKA operations were carried out by the same surgeon. Wound contamination was assessed using a wound culture technique. Blinded laboratory analysis was performed.
Results
There were 5/50 culture positive cases when a SHS was used compared to 0/25 when a SG was used; but this difference was not statistically significant (p = 0.16). There were 4/24 culture positive cases when SHS with tape was used compared to 1/26 when SHS without tape was used; but this difference was not statistical significant p = 0.18.
Conclusion
We found no difference in wound contamination between SG and SHS. Addition of tape at the gown/glove interface did not alter the contamination rate. The choice of surgical gown should take into account cost, comfort and personal protection; as this study found no evidence that wound contamination rates will be altered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Charnley introduced the body exhaust suit (BES) [1, 2] in an attempt to reduce wound contamination during arthroplasty, and in a large randomised trial BES reduced infection rates by 90% (0.7 vs. 0.06%) [3]. However, negative-pressure BES with intake and exhaust tubing were cumbersome, leading to the development of the modern positive-pressure SHS, where air is drawn into the grown through a hood via a helmet-mounted fan. The positive pressure inside SHS is a concern, as air under positive pressure may escape through any gap which is not sealed, such as between the surgeon’s gown and glove. Recent studies using fluorescent particles found increased contamination around the surgeon’s cuffs when using SHS in comparison to conventional gowns [4, 5].
Additionally, Hooper et al. [6] reported data from the New Zealand Joint Registry, showing higher rates of early revision due to infection in both hip and knee arthroplasty procedures performed using SHS compared to conventional gowns (0.251 vs. 0.028%, p = 0.016). Other reports found similar findings, and the lower infection rates seen in earlier BES studies have not been replicated in studies on modern SHS (Table 1).
However, proving causation using registry data is difficult as patient groups are uncontrolled, and it is thus difficult to exclude all potential confounding variables. As deep infection is rare, clinical studies are difficult to power adequately. ‘Surrogate’ markers for infection are therefore used, such as air particle counts or wound washings [7,8,9,10]. Recently, tetrazolium-stained membrane imprint (TSMI) technique has been used to compare wound contamination, providing a culture-based technique to allow more accurate identification of contamination [10].
The aim of this study was to use TSMI culture to evaluate whether SHS gowns lead to increased wound contamination in TKA surgery, and whether this contamination can be reduced by the use of tape around the surgeon’s glove.
Materials and methods
Between March 2013 and September 2014, 75 patients undergoing primary TKA for osteoarthritis were enrolled in this prospective, randomised controlled trial. All patients undergoing primary TKA under a single surgeon were eligible for enrolment. Patients were advised of the study in preadmission and consented on the day of surgery at the time of the surgical consent. Inclusion criteria were that the primary TKA was for osteoarthritis, and that the single surgeon in the study was performing the procedure. The study was approved prospectively by the regional ethics and disability committee, as well as the institution in which it was performed.
Patients were randomised into three groups using sequentially numbered, sealed and opaque envelopes that were opened in theatre. Randomisation was performed prior by a third-party off site using a random number generator. In group 1, the scrubbed theatre staff wore standard surgical gowns. In group 2, the scrubbed theatre staff wore SHS without tape at the gown/glove interface. In group 3, the scrubbed theatre staff wore SHS with tape at the gown/glove interface on both cuffs. All TKAs were carried out in a standardised manner with 2 g of prophylactic cefazolin administered prior to the skin incision, in one of two ultra clean conventionally ventilated theatres. Following a previously described technique [10], after initial incision two cellulose acetate and nitrate membrane filters [Millipore (UK) Ltd., Watford, UK] measuring 47 mm in diameter with a pore size of 5 μm were placed onto the wound for 30 s, then transferred to agar with β-lactamase (190 units/l agar) to neutralise the cefazolin used for antibiotic prophylaxis. Five more membranes were then placed onto the wound prior to closure or at the end of the first hour which ever came first. The incubation of wound samples was aerobic. Although anaerobic organisms can be identified in air, infection of implants by anaerobes is very uncommon. The samples were incubated at 37 °C for 48 h. They were then stained with tetrazolium (0.5 ml of 0.75%) which allowed the living bacterial colonies to be easily distinguished from the dead tissue (Fig. 1). This TSMI culture technique is previously described [13]. Skin-to-skin operative time was recorded to ensure that the gown was not affecting operative time.
Based on the studies conducted by Hooper et al. and Der Tavitian et al., we estimated that there would be a twofold increase in wound contamination when SHS were used [6, 10]. A sample size of 23 in each group was required to give 80% power to detect a significant difference between the groups (p < 0.05). We recruited 75 patients in total to allow for any technical issues with the TSMI method.
The outcome measure was the number of cases with positive cultures and negative controls using the tetrazolium-stained membrane imprint technique. All cases were performed in one of two ultra clean, conventionally ventilated operating rooms.
Statistical analysis was performed using SPSS 20 software. A Fisher’s exact test was used to determine statistical significance as there were values less than 5 for two of the groups.
Results
The average patient age was 67 with a range from 42 to 84. Sixty-four percent were females (48/75). Neither age nor sex was statistically different between the three groups. Operative time was no different between the three groups. The average time for a TKA in the standard gown was 66.9 ± 9.7 min, in a SHS with tape 65 ± 14.7 min and in a SHS without tape 64 ± 11.6 min (Table 2).
There were more culture positive cases in the SHS group (5/50) compared to the standard gown group (0/25). However, this did not reach statistical significance p = 0.16.
There were more culture positive cases in the group with tape around the gown/glove interface (4/24) compared to the group without tape at the gown/glove (1/26). However, this did not reach statistical significance p = 0.18.
Discussion
Charnley’s BES was reported to significantly reduce deep infection in a large randomised clinical trial in 1982 [3]. Although used with the same goal of reducing infection, modern positive pressure suits are fundamentally different and evidence of the same benefit has not been proven. Contamination at the gown/glove interface due to the positive pressure within the suit has been described as a possible mechanism in two studies [4, 5], and the role of modern SHS in decreasing infection in arthroplasty remains unclear. This randomised controlled trial sought to answer this question by measuring wound contamination as a surrogate marker for deep infection, and found no difference in contamination rates between SHS with or without tape and conventional theatre attire.
There were limitations to this study. First, our overall contamination rate was lower than in the Der Tavitian study [10] on which our power calculation was based, raising the possibility of a type II error. Our lower contamination rate may be due to less contamination in a more modern operating theatre, or possibly due to an unknown difference in sampling technique. Second, the nature of the relationship between intraoperative contamination and deep infection is unclear, making interpretation of contamination studies such as this difficult. Studies show a correlation between infection and contamination [3], however, little is known about whether this is a linear relationship or whether there is a ‘threshold’ level of contamination above which deep infection is more likely to occur. However, as deep infection is rare following arthroplasty, prospective studies using this as an outcome are difficult to perform. We therefore focused on intraoperative contamination, as a surrogate marker for deep infection.
Although we were unable to demonstrate a difference in contamination levels between groups; there are several factors that have been postulated to increase wound contamination with SHS. First, theatre room staff are thought to be the source of contamination in 98% of cases; [11, 12] an individual can shed between 5000 and 55,000 particles per minute [13]. Increased temperature and airflow inside SHS may increase bacterial shedding [14]. SHS gowns are a positive pressure system which is fundamentally different from the original negative pressure BES. Positive pressure may lead to skin particles escaping at the gown/glove interface [4]. The intake fan on the helmets may also disrupt operating room ventilation by drawing air around the surgeon’s head and potentially particles [4].
Despite these potential causes, we were unable to show a difference in contamination between SHS and SG. We were also unable to show a difference between SHS with or without tape at the gown/glove interface. This is consistent with the findings of a recent systematic review, which found while there was clear evidence of a reduction in both wound contamination and deep infection rates with BES; no such difference was seen between the SHS and SG groups [15]. Studies comparing both BES and SHS to conventional attire were reviewed. In contrast to BES, SHS were not shown to decrease and in some cases even increase both air and wound contamination. Registry studies of deep infection showed either no difference or slightly increased deep infection when SHS were used.
Only one previous study has compared wound contamination with SHS or SG in arthroplasty. In 2003, Der Tavitian and colleagues compared air and wound counts between the two groups at 10 min intervals in total hip arthroplasty [10]. They found a mean of 14 positive cultures in the SHS group and 8 in the SG group, but the difference was not significant. There was no correlation between air and wound counts, and the trend of increased wound contamination with time suggested wound contamination was a better surrogate marker for deep infection. In contrast, four previous studies have compared wound contamination between BES and conventional gowns; two of which showed decreased contamination compared to normal gowns and two which showed a trend towards decreased contamination but did not reach statistical significance [15].
A recent retrospective study of 56,216 primary TKA’s by Namba and colleagues evaluated multiple patient and perioperative risk factors for deep infection, although they found multiple associations the use of a BES was not statistically significant [16].
A systematic review and mixed treatment comparison by Zheng and colleagues further highlights the complexity of analysing single elements of infection control in arthroplasty and the overshadowing benefit of prophylactic systemic antibiotics [17].
In conclusion, we found no difference in wound contamination in TKA with the use of normal gowns vs. SHS. The addition of tape at the gown/glove interface did not alter the contamination rate. The overall contamination rate was very low, and if a true difference exists it is likely to be small. The choice of surgical attire in TKA should take into account cost, surgeon preference and personal protection; however, there is currently little evidence that the use of SHS will alter wound contamination or rates of deep infection.
References
Charnley J (1964) A clean-air operating enclosure. Br J Surg 51:202
Charnley J (1979) Low friction arthroplasty of the hip. Springer, Berlin
Lidwell O, Lowbury E, Whyte W (1982) Effect of ultraclean air in operating rooms on deep sepsis in the joint after total hip or knee replacement: a randomised study. Br Med J 285:10–14
Young SW, Chisholm C, Zhu M (2014) Intraoperative contamination and space suits: a potential mechanism. Eur J Orthop Surg Traumatol 24(3):409–413 (Epub 2013 Feb 9)
Fraser JF, Young SW, Valentine KA, Probst NE, Spangehl MJ (2015) The gown-glove interface is a source of contamination: a comparative study. Clin Orthop Relat Res 473(7):2291–2297
Hooper GJ, Rothwell AG, Frampton C, Wyatt MC (2011) Does the use of laminar flow and space suits reduce early deep infection after total hip and knee replacement?: the ten-year results of the New Zealand Joint Registry. J Bone Jt Surg Br 93–1:85–90
Blomgren G, Hambraeus A, Malmborg AS (1983) The influence of the total body exhaust suit on air and wound contamination in elective hip-operations. J Hosp Infect 4–3:257–268
Bohn WW, McKinsey DS, Dykstra M, Koppe S (1996) The effect of a portable HEPA-filtered body exhaust system on airborne microbial contamination in a conventional operating room. Infect Control Hosp Epidemiol 17:419
Shaw JA, Bordner MA, Hamory BH (1996) Efficacy of the Steri-Shield filtered exhaust helmet in limiting bacterial counts in the operating room during total joint arthroplasty. J Arthroplasty 11–4:469–473
Der Tavitian J, Ong SM, Taub NA, Taylor GJS (2003) Body-exhaust suit versus occlusive clothing. A randomised, prospective trial using air and wound bacterial counts. J Bone Jt Surg Br 85–4:490–494
Owers KL, James E, Bannister GC (2004) Source of bacterial shedding in laminar flow theatres. J Hosp Infect 58–3:230–232
Whyte W, Hodgson R (1982) The importance of airborne bacterial contamination of wounds. J Hosp Infect 3(2):123–135
Anon (1996) Surgical helmet systems. Health Devices 25(4):116–145
Newton G, Brown S, Dias J, Bullock D (1991) Can conventional theatre clothing be as effective as the “space suit”. J Bone Jt Surg (Br) 73-B:170
Young SW, Zhu M, Shirley OC, Wu Q, Spangehl MJ (2016) Do ‘surgical helmet systems’ or ‘body exhaust suits’ affect contamination and deep infection rates in arthroplasty? A systematic review. J Arthroplasty 31(1):225–233 (Epub 2015 Aug 1)
Namba RS, Inacio MCS, Paxton EW (2013) Risk factors associated with deep surgical site infections after primary total knee arthroplasty. J Bone Jt Surg Am 95:775–782
Zheng H, Barnett AG, Merollini K et al (2014) Control strategies to prevent total hip replacement-related infections: a systematic review and mixed treatment comparison. BMJ Open 4:003978
Acknowledgements
Funding was provided by Wishbone Trust NZOA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Each author certifies that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Ethical approval
Ethical approval granted by the Northern ethical committee, reference number 12/NTA/11.
Rights and permissions
About this article
Cite this article
Shirley, O.C., Bayan, A., Zhu, M. et al. Do surgical helmet systems affect intraoperative wound contamination? A randomised controlled trial. Arch Orthop Trauma Surg 137, 1565–1569 (2017). https://doi.org/10.1007/s00402-017-2795-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-017-2795-7