Abstract
Introduction
Serum metal ions are part of the regular follow-up routine of patients with metal-on-metal total hip arthroplasties (MoM-THA). Increased cobalt levels have been suggested to indicate implant failure and corrosion.
Questions
(1) Is there a correlation between the size of the osteolysis measured on a CT scan and metal ion levels? (2) Can metal ion levels predict the presence of osteolysis in MoM-THA? (3) Are cobalt and chromium serum levels or the cobalt-chromium-ratio diagnostic for osteolysis?
Materials and methods
CT scans of patients (n = 75) with a unilateral MoM-THA (Birmingham Hip System, Smith & Nephew, TN, USA) implanted by a single surgeon were reviewed to determine the presence of osteolysis. Statistical analysis was performed to detect its association with metal ion levels at the time of the imaging exam.
Results
The incidence of osteolysis was the same in men and women (35.6 vs 35.7 %). The cobalt-chromium-ratio correlates with the size of the osteolysis on the CT scan and the femoral component size in the overall study population (p = 0.050, p = 0.001) and in men (p = 0.002, p = 0.001) but not in women (p = 0.312, p = 0.344). The AUC for the cobalt-chromium-ratio to detect osteolysis was 0.613 (p = 0.112) for the overall population, 0.710 for men (p = 0.021) and 0.453 (p = 0.684) for women. The data suggest that a cut off level of 1.71 for the cobalt-chromium-ratio has a sensitivity of 62.5 % and specificity of 72.4 % to identify male patients with osteolysis.
Conclusions
The disproportional increase of cobalt over chromium, especially in male patients with large component sizes can not be explained by wear alone and suggests that other processes (corrosion) might contribute to metal ion levels and might be more pronounced in patients with larger component sizes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Large head metal-on-metal hip arthroplasties (MoM-THA) have shown high failure rates in the past despite the initial hope of providing low bearing wear rates [1, 2]. The Birmingham Hip System (Smith & Nephew, Memphis, TN), which has shown good clinical results in the long-term follow-up when used in resurfacing [3], has a failure rate of 12.0 % at 10 years in the National Joint Replacement Registry of Australia when used in THA [4]. Most common reasons for failure are metal related pathologies including adverse reaction to metal debris (ARMD) and osteolysis/loosening [4]. Metal ions have been suggested as a marker for failure of implants as they may represent accelerated wear of the bearing surface in resurfacing [5], however, studies have shown that cobalt and chromium may not have enough sensitivity to detect tissue or bone reaction in MoM-THA [6]. Furthermore, compared to resurfacings, MoM-THAs are suspected to fail due to corrosion of their taper junction [7]. The resulting corrosion products and metal ions might promote a different immunologic response and might, therefore, explain the higher failure rates of MoM-THA compared to HR.
Most studies investigating the relationship between serum metal ions and imaging findings focus on soft-tissue reactions, [8] however, osteolysis, the second most common reason for revision in MoM-THA [4], has not been studied extensively. Gender may be an important factor for failure of metal-on-metal hip replacement [9], however, there is currently no data linking gender to osteolysis in MoM-THAs.
The current study analysis the following research questions: (1) Is there a correlation between the size of the osteolysis measured on a CT scan and metal ion levels? (2) Can metal ion levels predict the presence of osteolysis in MoM-THA? (3) Are cobalt and chromium serum levels or the cobalt-chromium-ratio diagnostic for osteolysis?
Materials and methods
Patients
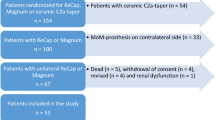
This study retrospectively investigates a series of patients with a MoM-THA using the Birmingham Hip System (Smith & Nephew, TN, USA) and the Synergy Stem (Smith & Nephew, TN, USA) performed by a single high-volume surgeon between 2007 and 2010. The study included patients with at least one CT scan and corresponding metal ion results more than 20 months after the index procedure. CT scanning is part of the senior authors’ regular follow-up routine 2–3 years after surgery. During the time period the senior author performed 109 unilateral MoM-THA. Five patients were lost to follow-up, 24 patients did not have a CT scan and 7 patients did not have corresponding metal ion levels. This left 73 patients for inclusion into the study. Demographic data, imaging studies (X-ray and CT scan) and metal ion levels were evaluated and collected in a secured Excel spreadsheet.
The study included 45 male and 28 female patients with an average follow-up of 65.9 months (range 33–94) after MoM-THA. The average age was 55.2 years (SD ±13.6) for men and 55.2 years (SD ±5.9) for women (p = 0.423).
Imaging Evaluation
Imaging was performed for all patients included in this study an average of 51. 6 months after surgery (range 20–91 months years). Anteroposterior radiographs were evaluated for acetabular inclination. The CT scan was retrospectively reviewed and patients were grouped into group A (no osteolysis) or group B (osteolysis) by the senior author. The dimension of osteolysis was reported by an experienced radiologist using PACS (Sectra IDS7, 2015, Linkoeping).
Serum metal ion levels
Cobalt and chromium serum levels were measured within 30 days of the CT scan in 70 patients and within 60 days in 3 patients.
Statistics
All statistical data analyses were performed using SPSS software (Version 23, IBM Corporation, New York). Since metal ions are not normally distributed, we used non-parametric tests for the analysis (Mann-Whitney U, Wilcoxon, Spearman). For correlations the Spearman test was used. We used a non-parametric ROC to determine sensitivity and specificity. A p value of p < 0.05 was considered statistically significant.
Results
Study population, radiological and laboratory data
Seventy-three patients (45 men, 28 women) with unilateral MoM-THA met the inclusion criteria (Table 1).
Femoral component size differed significantly between men and women (47.1 vs 43.6, p < 0.001). There was no significant difference between other demographic data and serum metal ion levels. 35.6 % (16/45) of the men and 35.7 % (10/28) of the women showed osteolysis on the CT scan (Table 2). There was no statical difference in the size of the osteolysis between men and women (p = 0.874).
Cobalt was significantly higher than chromium in men (p < 0.001), and showed a trend in women (p = 0.086). Cobalt (p = 0.117) and chromium (p = 0.803) did not differ significantly between men with osteolysis and men without osteolysis, however, the cobalt-chromium-ratio was significantly higher for male patients with osteolysis (average 3.0; range 1–15) than for patients without osteolysis (average 1.5; range 0.2–5.1) (p = 0.021). In women with or without osteolysis there was no significant difference for the three parameters (cobalt: p = 0.755, chromium: p = 0.733, ratio: p = 0.684). The average ratio in female patients with osteolysis (average 1.8; range 0.7–5.9) was similar to the ratio in patients without osteolysis (average 1.8; range 0.74–10.0).
Correlation metal ions, femoral component size and size of the osteolysis
The cobalt-chromium-ratio correlated significantly with the size of the osteolysis on the CT scan and the femoral component size in the whole study population (Table 3). There was no correlation between component size and size of the osteolysis, neither in the whole study population nor in men or women alone (Tables 3, 4, 5). However, divided by gender the cobalt-chromium-ratio correlated with the size of the osteolysis in men only( p = 0.002) (Fig. 1). This was also found in patients without revision (k = 376; p = 0.016) which in general had smaller areas of osteolysis and were followed up. The femoral head size correlated with cobalt (p = 0.008) and the cobalt-chromium-ratio (p = 0.001) in men (Tables 2, 3).
ROC analysis
In the overall population neither the cobalt-chromium-ratio (AUC of 0.613, p = 0.112) nor cobalt (AUC of 0.586, p = 0.224) and chromium levels (AUC of 0.493, p = 0.927) showed a significant correlation with osteolysis on CT scans. However, for men the cobalt-chromium-ratio had an AUC of 0.710 for pathologic CT (p = 0.021, CI 0.556–0.864) (Fig. 2). The data suggest that a cut off level of 1.71 for the cobalt-chromium-ratio has a sensitivity of 62.5 % and specificity of 72.4 % to identify male patients with osteolysis. Cobalt serum ions (AUC: 0.642, p = 0.118, CI 0.474–0.810) and chromium serum ions (AUC: 0.523, p = 0.803, CI 0.338–0.707) performed worse. For women none of the three parameters showed a significant correlation (ratio: AUC 0.453, p = 0.684; cobalt: AUC 0.536, p = 0.755; chromium: AUC 0.467, p = 0.774) (Fig. 3).
Post-hoc power analyses (alpha error 0.05) were performed for the observed ratios and sample sizes of men and women with and without osteolysis. This showed a power of 2.5 % for men and women respectively.
Discussion
Metal-on-metal total hip arthroplasties can develop osteolysis [10] and are reported to have increased metal ion levels secondary to corrosion and bearing surface wear [1, 11]. The diagnosis of osteolysis in metal-on-metal THA remains challenging and no risk factor for progression has been identified. Our data show a significant correlation between the size of the osteolysis and the cobalt-chromium-ratio in men. However, considering the relatively low sensitivity and specificity the study failed to establish a clear threshold for the diagnosis of osteolysis.
Our study has the following limitations: (1) the differential diagnosis between degenerative cysts and osteolysis is difficult in small lesions (2) since not all patients underwent revision surgery, the findings could not be confirmed intraoperatively in all patients (3) the study is retrospective in nature, however, metal ion levels and imaging results are in general not influenced by this. (4) While the post-hoc power analysis suggests that the study might be underpowered to show a significant difference between the Cobalt-Chromium-ratio for patients with and without osteolysis, the area under the curve for the ROC in male patients (0.71) supports the value of the ratio as a diagnostic test to identify male patients with osteolysis.
Periprosthetic osteolysis and resulting aseptic loosening are common reasons for revision in total hip arthroplasty [12]. In MoM-THA adverse reactions to metal debris (ARMD) and osteolysis are an important failure mechanism [8, 13]. Osteolysis is based on a cellular response caused by material released from the arthroplasty which disrupts the normal balance between bone formation and resorption. Hayter et al. [14] found osteolysis in 24.1 % of the patients with a painful MoM-THA compared to 35.6 % in the current study. The increased incidence of osteolysis might be related to the fact that all patients in the current study underwent CT scanning, a test very sensitive for identifying osteolysis.
Elevated metal ions [1, 15], female sex [16] and small femoral diameter [1] are confirmed risk factors for the development of ARMD. However, the current paper is the first to suggest that a correlation between the size of osteolysis and the cobalt-chromium ratio exists in men with a BHR MoM-THA. Studies have previously shown that cobalt is raised out of proportion compared to chromium in large head metal-on-metal arthroplasties [17]. Taper sleeve corrosion has been accused to be an independent source of cobalt ion levels [7, 18].
There has been an attempt to standardize the follow-up protocols for MoM-THA and resurfacings [19, 20]. However, most protocols are not evidence based, have not proven its cost effectiveness [21] and do not agree on the optimal type of cross sectional imaging [19, 20]. Despite the significant correlation between the cobalt-chromium-ratio and the size of osteolysis in the current study, a clear cut off threshold could not be established. The study supports the importance of cross sectional imaging in the workup of MoM-THA as laboratory parameters lack sensitivity and specificity. Although CT scanning appears to be a better imaging test for the detection of osteolysis compared to metal artifact reduction sequence (MARS) MRI in metal-on-metal hip arthroplasties [22, 23], it has not been widely recognized in screening protocols for MoM-THA [19, 20, 24, 25].
A recent publication by Fehring et al. [26] concluded that the cobalt-chromium ratio does not predict tissue damage at the time of revision surgery. The paper has come under criticism because it: (1) was not based on a clearly defined study population, (2) did not include all patients with revision surgery, (3) did not report the cobalt-chromium-ratio for non-revised patients, (4) and assumed normal distribution of the metal ion levels without testing for it [27]. The current paper reports data on a well-defined study population and includes revised as well as non-revised patients. In addition non-parametric tests were used since the data are not normally distributed.
Conclusion
Cobalt and chromium are routinely measured during the follow-up of MoM-THA. The disproportional increase of cobalt over chromium, especially in male patients with large component sizes cannot be explained by wear alone and suggests that other processes (corrosion) might contribute to metal ion levels and might be more pronounced in patients with larger component sizes. This might suggest an increased risk for patients with bilateral Modular Birmingham MoM-THA.
References
Bolland BJ et al (2011) High failure rates with a large-diameter hybrid metal-on-metal total hip replacement: clinical, radiological and retrieval analysis. J Bone Joint Surg Br 93(5):608–615
Langton DJ et al (2011) Accelerating failure rate of the ASR total hip replacement. J Bone Joint Surg Br 93(8):1011–1016
Daniel J et al (2014) Results of Birmingham hip resurfacing at 12 to 15 years: a single-surgeon series. Bone Joint J 96-B(10):1298–1306
National Joint Replacement Registry Australian Orthopaedic Association, Metal on Metal Total Conventional Hip Arthroplasty Supplementary Report. 2014: Australia
De Smet K et al (2008) Metal ion measurement as a diagnostic tool to identify problems with metal-on-metal hip resurfacing. J Bone Joint Surg Am 90(Suppl 4):202–208
Bosker BH et al (2015) Pseudotumor formation and serum ions after large head metal-on-metal stemmed total hip replacement. Risk factors, time course and revisions in 706 hips. Arch Orthop Trauma Surg 135(3):417–425
Cooper HJ et al (2012) Corrosion at the head-neck taper as a cause for adverse local tissue reactions after total hip arthroplasty. J Bone Joint Surg Am 94(18):1655–1661
Bayley N et al (2015) What are the predictors and prevalence of pseudotumor and elevated metal ions after large-diameter metal-on-metal THA? Clin Orthop Relat Res 473(2):477–484
Latteier MJ et al (2011) Gender is a significant factor for failure of metal-on-metal total hip arthroplasty. J Arthroplasty 26(6 Suppl):19–23
Carr AM, DeSteiger R (2008) Osteolysis in patients with a metal-on-metal hip arthroplasty. ANZ J Surg 78(3):144–147
Lohmann CH et al (2014) Metallic debris from metal-on-metal total hip arthroplasty regulates periprosthetic tissues. World J Orthop 5(5):660–666
Kurtz S et al (2005) Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am 87(7):1487–1497
Lombardi AV et al (2015) Large-diameter metal-on-metal total hip arthroplasty: dislocation infrequent but survivorship poor. Clin Orthop Relat Res 473(2):509–520
Hayter CL et al (2012) MRI findings in painful metal-on-metal hip arthroplasty. AJR Am J Roentgenol 199(4):884–893
Bosker BH et al (2012) High incidence of pseudotumour formation after large-diameter metal-on-metal total hip replacement: a prospective cohort study. J Bone Joint Surg Br 94(6):755–761
Reito A et al (2013) High prevalence of adverse reactions to metal debris in small-headed ASR™ hips. Clin Orthop Relat Res 471(9):2954–2961
Hart AJ et al (2014) Surveillance of patients with metal-on-metal hip resurfacing and total hip prostheses: a prospective cohort study to investigate the relationship between blood metal ion levels and implant failure. J Bone Joint Surg Am 96(13):1091–1099
Matharu GS et al (2015) Influence of implant design on blood metal ion concentrations in metal-on-metal total hip replacement patients. Int Orthop. doi:10.1007/s00264-014-2644-z
U.S. Food and Drug Administration, General Recommendation for Orthopaedic Sugeons after Metal-on-Metal Hip Replacment Surgery (Follow-up) (2015)
European Federation of National Associations of Orthopedics and Traumatology. Consensus statement “Current evidence on the management of metao-on-metal bearings” (2012). https://www.efort.org/wp-content/uploads/2013/10/2012_05_10_MoM_Consensus_statement1.pdf. Accessed 18 June 2015
Matharu GS et al (2015) Follow-up of metal-on-metal hip arthroplasty patients is currently not evidence based or cost effective. J Arthroplasty. doi:10.1016/j.arth.2015.03.009
Robinson E et al (2014) Cross-sectional imaging of metal-on-metal hip arthroplasties. Can we substitute MARS MRI with CT? Acta Orthop 85(6):577–584
Waldstein W, Schmidt-Braekling T, Boettner F (2014) MRI does not detect acetabular osteolysis around metal-on-metal Birmingham THA. Arch Orthop Trauma Surg 134(7):1009–1015
Health Canada Government of Canada. Metal-on-metal hip implants-information for orthopaedic surgeons regarding patient management following surgery-for health professionals (2015). http://www.healthycanadians.gc.ca/recall-alert-rappel-avis/hc-sc/2012/15835a-eng.php. Accessed 19 June 2015
Therapeutic Goods Administration Department of Health Australian Government. Metal-on-metal hip replacement implants–information for general practitioners, orthopaedic surgeons and other health professtional (2012). https://www.tga.gov.au/metal-metal-hip-replacement-implants. Accessed19 June 2015 (recommend)
Fehring TK et al (2015) Cobalt to Chromium ratio is not a key marker for adverse local tissue reaction (ALTR) in metal on metal hips. J Arthroplasty 30(9 Suppl):107–109
Reito A, Lainiala O, Eskelinen A (2015) Letter to Editor: cobalt to chromium ratio is not a key marker for adverse local tissue reaction in metal-on-metal hips. J Arthroplasty. doi:10.1016/j.arth.2015.09.019
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We certify that we have not signed any agreement with commercial interest related to this study, which would in any way limit publication of any and all data generated for the study or to delay publication for any reason. The senior author reports personal fees from Smith & Nephew, personal fees from Ortho Development Corporation and personal fees form Depuy, outside the submitted work.
Rights and permissions
About this article
Cite this article
Renner, L., Schmidt-Braekling, T., Faschingbauer, M. et al. Do cobalt and chromium levels predict osteolysis in metal-on-metal total hip arthroplasty?. Arch Orthop Trauma Surg 136, 1657–1662 (2016). https://doi.org/10.1007/s00402-016-2565-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-016-2565-y