Abstract
Introduction
The aim of this prospective study was to investigate the effect of local hip bone density on mechanical failure after fixation of pertrochanteric fractures and to establish possible risk factors for the failures.
Materials and methods
A total of 136 consecutive patients presenting a closed unilateral pertrochanteric fracture were enrolled. The patients were treated with a sliding hip screw or an intramedullary nail. Dual energy X-ray absorptiometry measurements for bone density of the contralateral hip were made within 4 weeks postoperatively. Follow-up evaluations on the standard radiographs were documented for any mechanical failure including loss of reduction, screw or blade cut-out, lateral migration of the screw or blade, and implant breakage. Secondary outcomes were also recorded including patient characteristics and fixation construct variables as possible predictors for mechanical failure.
Results
At a minimum of 2 years of follow-up, 38 patients were reported with mechanical failure at an estimated risk of 27.9 %. The local bone density measurements for the study population showed no difference between patients with (0.710 g/cm2) and without (0.726 g/cm2) mechanical failure (P = 0.180). We also observed no significant correlation between local bone density and failure in patients with good fracture reduction (P = 0.862). The multivariate regression analysis identified fracture type (P < 0.001) and quality of fracture reduction (P < 0.001) as being independent predictors for mechanical failure, whereas local bone density was not (P = 0.658).
Conclusions
Local hip bone density does not appear to have a significant influence on mechanical failure after internal fixation of pertrochanteric fractures. Stable fractures and fractures with good reduction are expected to obtain satisfactory outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pertrochanteric fractures are likely common fractures secondary to osteoporosis in advanced age, and account for about 40–50 % of hip fractures [1, 2]. Treatment of pertrochanteric fractures with extramedullary or intramedullary implants has the potential to achieve good clinical outcome even in patients with poor bone quality [1, 3–5]. In comparison with plate system, nail fixation appears to have more advantages of superior mechanical property in unstable fractures [2, 6]; even though, a substantial number of complications including mechanical failure (MF) are known [7–10].
Among the factors contributing to MF, poor local bone quality was assumed to lead to a high number of mechanical complications [8, 11, 12]. However, most of the earlier studies aimed to investigate the significant correlation between whole-body bone mineral density (BMD) and fixation failure, without accounting for local BMD on the proximal femur [14, 15]. Owing to this limitation, the association between local hip bone density and MF has not yet been proven in a clinical setting.
For these reasons, the primary purpose of this prospective study was to investigate the effect of local bone density on MF. We hypothesized that a lower local BMD leads to a higher rate of postoperative MF in patients with pertrochanteric fractures. Secondary outcomes focused on other variables that could potentially impact on postoperative failures.
Patients and methods
Patient selection
From May 2011 to December 2012, a consecutive series of 212 patients who met the criteria was included in the prospective study at our trauma center. This protocol was in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans and was approved by the institutional review board of our hospital. The inclusion criteria included patients aged 50 years and older and with a radiologically confirmed, acute, closed, unilateral pertrochanteric fracture due to a traumatic injury, with surgical treatment of internal fixation. The exclusion criteria were (1) multiple fractures; (2) fractures with concomitant severe visceral injury; (3) a history of previous injury or operation of the affected limb which could mislead the evaluation of hip function; (4) previous dysfunction of the hip such as osteoarthritis or osteonecrosis of the femoral head; (5) pathological fractures; (6) cognitive impairment which might impose an influence on compliance to postoperative rehabilitation; (7) a follow-up of less than 2 years after the surgery.
Out of 212 patients, 5 patients were excluded because of refusal to participate in the study and 43 patients who failed to meet the exclusion criteria were also ruled out (Fig. 1). Thus, the remaining 164 patients (113 females and 51 males) were eligible to undergo a dual-energy X-ray absorptiometry (DXA) scan. All enrolled patients signed the written informed consents prior to entering the study. The mean age of those patients was 77.2 years (range 50–92 years). The causes of the fractures consisted of traffic accidents (19 patients), sports injury (35 patients), falling from a height (13 patients) and falling down (97 patients). According to the mechanism of the injury, 37 patients sustained a high-energy injury whereas 127 patients suffered a low-energy hip fracture.
Local bone density scan
Following the recommendation by World Health Organization [16], we measured local bone density of the contralateral hip using DXA (GE-LUNAR Corp, Madison, WI) within the first 4 weeks postoperatively. Local hip BMD scan was performed in three bone sites of femur (neck, intertrochanteric zone and trochanter) according to the manufacturer’s guidelines, and the mean BMD was recorded thereafter. To minimize errors in the measurements, the lower limb was fixed at an internal rotation of 15° during the scan. According to the guideline, the measurement of BMD in Ward’s triangle was not applied due to poor accuracy for repeated measurements [16]. Meanwhile, whole-body BMD scan was made to screen osteoporosis, which was diagnosed with a T score less than −2.5. As per the records, all the scans were done by a single examiner. Prior to the injury, only 29 patients administered calcium and Vitamin D regularly. The patients received a standard treatment protocol including bisphosphonate, strontium, or PTH as soon as osteoporosis was diagnosed.
Surgical interventions
The surgical procedures were performed within 48 h of admission, by four surgeons including one junior surgeon, two senior surgeons and one hip specialist. The mean time between the injury and operation was 2.0 days (range 0–5 days). All the patients were operated on a supine position on a fracture table using standard reduction techniques. The sliding hip screw system (Synthes, Solothurn, Switzerland) was used for extramedullary fixation of the stable fractures, whereas the Proximal Femoral Nail Antirotation (PFNA-II) (Synthes, Solothurn, Switzerland) was used for intramedullary fixation. The decision of a short or long implant was also left to the surgeons. However, a short nail was used in patients with extremely anterior bowing of the femur to avoid stress contact or penetration to the cortical bone.
All the patients received prophylactic intravenous antibiotics before the procedure. The patients were allowed to fully bear weight as tolerated on the injured hip after surgery [17]. Systematical passive and active rehabilitation was tailored to the characteristics and needs of the individual patients in collaboration with a physical therapist.
Follow-up
The patients were reviewed at 6 weeks, 3, 6 months after surgical procedure, followed by yearly review thereafter. During the entire follow-up, all mechanical and non-mechanical complications were noted.
Radiologic reviews were done using two standard views, i.e., anteroposterior (AP) and lateral radiographs, which were taken by one senior radiologist on the first day after surgery and at every follow-up. Potential magnification errors were corrected with the use of a metal coin of a known diameter as the reference. Preoperative and postoperative radiographs were analyzed by an independent investigator and were then confirmed by another senior surgeon who did not participate in the procedures. The fractures were classified preoperatively according to AO/OTA classification [18] and subsequently categorized as either stable (31-A1.1, 31-A1.2, 31-A1-3, and 31-A2.1) or unstable (31-A2.2, 31-A2.3, 31-A3.1, 31-A3.2, and 31-A3.3) (Fig. 2) [19].
On the immediate postoperative radiographs, we focused our evaluations on the quality of fracture reduction and the position of the screw or blade. In addition, we measured neck-shaft angle which refers to the angle formed by axis of femoral shaft and line drawn along the axis of the femoral neck which passes through the center of the femoral head. We introduced neck-shaft angle in the present study as it was an important reference for the displacement of the fragments and implants. The quality of fracture reduction was graded as good when there was normal or valgus alignment on an anteroposterior radiograph with a less than 20° of angulation on the lateral radiographs, and a less than 4 mm of displacement between the major fragments [20]. Otherwise, poor reduction was graded when the reduction met neither criteria. Moreover, the position of the screw or blade in the femoral head was assessed using tip–apex distance (TAD) described by Baumgaertner et al. [21]. According to TAD, the patients were categorized into two groups: greater than or equal to 25 mm and less than 25 mm.
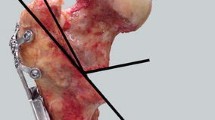
Follow-up radiographs were assessed for the presence or absence of MF and bone healing. We defined MF as loss of fracture reduction, screw or blade cut-out, lateral migration of the screw or blade, and implant breakage. Loss of reduction was defined as displacement of the fractures, varus deformation or loss of neck-shaft angle greater than 10° as compared to the immediate postoperative radiographs (Fig. 3) [21]. The amount of lateral migration of the screw or blade was measured on the AP views by comparing the immediate postoperative radiographs with the most recent radiographs and was calculated as the change in the relative length of the unengaged part of the screw or blade, after correcting for the magnification. We defined excessive lateral migration as the migration laterally greater than or equal to 10 mm (Fig. 4). As to bone healing, union was defined as visible callus in more than two planes without complaints about pain during full weight bearing, whereas non-union was defined as having no callus formation after 6 months and the lacking of progressive fracture healing on three consecutive radiographs taken 1 month apart [19].
a The preoperative radiograph showed a stable pertrochanteric fracture (AO/OTA 31-A1.2) in a 75-year-old female patient. b The immediate postoperative radiograph showed a good reduction with the neck-shaft angle of 122° (α 1). Neck-shaft angle refers to the angle formed by axis of femoral shaft and a line drawn along the axis of the femoral neck which passes through the center of the femoral head. c The radiograph at the follow-up of 6 months after surgery showed the occurrence of mechanical failure (α 2 = 106°). Varus deformation was found with loss of neck-shaft angle of 16°
a The preoperative radiograph showed a pertrochanteric fracture (AO/OTA 31–A2.1) in an 81-year-old female patient. b The immediate postoperative radiograph showed a good reduction. The true length of the unengaged part of the blade (true d 1) was calculated by multiplying the relative length measured on the radiograph (d 1) with the magnification of the radiograph. The magnification was calculated by dividing the true diameter of the coin by the diameter measured on the radiograph (d c1). c The radiograph at the follow-up of 6 months after surgery showed the occurrence of blade lateral migration. Excessive lateral migration was found as the migration laterally of 15 mm (true d 2–true d 1)
The final evaluations on both clinical and radiological outcomes were performed blindly by another independent surgeon at the endpoint of the follow-up.
Statistical analysis
We used IBM SPSS Statistics, Version 20.0 for Windows (SPSS Inc., Chicago, Illinois) for all analyses. All continuous variables were expressed as mean ± standard deviation, and the categorical variables were expressed by the absolute and relative frequencies. To investigate the effect of local bone density, we categorized the patients into mechanical failure (+MF) group and non-mechanical failure (−MF) group on the basis of complications observed at the final follow-up. Fisher’s exact test, Student’s t test and ANOVA test were performed for quantitative data, and Chi-square test was used to find out the difference of categorical variables between the two groups. Sum rank test was used to analyze the data regarding the type of the surgeons, which was considered as one-way ordinal contingency table. Multivariate linear regression analysis was then conducted to assess any independent predictors of postoperative failure. Variables that were factored in the multivariate regression model included gender, age, bone mass index, fracture side, accident type, fracture type, nail length, quality of reduction, the type of the surgeons, implant type, TAD, T score, and local BMD. Odds ratio (OR) was used to describe the risk of failure. P value of 0.05 or less was considered as significant.
According to the statistics program based on G-power 3.1 software (Grant Devilly, Vic., Australia), the minimum number of participants to satisfy this independent measurement design was required to be 68 in total. The significance level was set to 0.05, the effect size to 0.25, and a power of 0.8 were set. Thus, a sample size of 164 participants was determined to be sufficient.
Results
Out of the 164 enrolled patients, 28 patients failed to accomplish the entire follow-up period of at least 2 years after surgery due to loss of contact or death from other conditions (Fig. 1). Therefore, the final cohort consisted of 136 patients, and the follow-up ranged from 2 to 3 years.
We found MF in 38 patients and the total failure rate was 27.9 % (Table 1). In the +MF group (n = 38), loss of reduction (18/38, 47.4 %) was the most commonly reported complication. Most of the failures (28/38, 73.7 %) were found within 3 months after surgery, whereas only 5.3 % (2/38) of the mechanical complications occurred after 1 year.
The mean areal BMD at the contralateral hip was 0.721 g/cm2 for the study population. The mean local BMD determined for the contralateral hip was not significantly different between the patients in the +MF (0.710 ± 0.066 g/cm2, range 0.534–0.837 g/cm2) and −MF group (0.726 ± 0.061 g/cm2, range, 0.572–0.854 g/cm2, P = 0.180). In terms of whole-body BMD, we observed a total of 16 patients with diagnosed osteoporosis in the +MF group and 41 patients in the −MF group (P = 0.977).
Significant differences were seen between the +MF and −MF group with regard to fracture type and fracture quality of reduction (both, P < 0.001) (Tables 2, 3). The failure rate was higher in unstable pertrochanteric fractures than in stable fractures (38.1 % versus 10.7 %). Moreover, less failure was also observed in patients with good fracture reduction (Tables 2, 3).
We subsequently investigated the cause of failures in patients with good fracture reduction. With respect to local bone density, we did not find any statistical difference between the patients with and without failure (mean, 0.723 g/cm2 versus 0.726 g/cm2, t = 0.175, P = 0.862). In the subgroup analysis of the same types of fractures treated by the same implant, local bone status was also not significantly different between the patients with and without MF (F = 1.005, P = 0.318) (Table 4).
Table 5 shows the logistic regression analysis. The results showed that local bone density was not a significant factor associated with MF (P = 0.658). The multiple linear regression model identified only unstable fractures (OR = 31.199, P = 0.005) and poor reduction of the fractures (OR = 9.308, P < 0.001) as the predictive factors for increased failure risk.
Discussion
The present study, including 136 pertrochanteric fracture patients over 50 years of age treated with plate or nail system, showed similar local BMD measurement of the contralateral hip between the patients with and without MF. The results challenge the widespread belief that BMD has a tremendous impact on postoperative outcome after pertrochanteric fractures [6, 7, 22–25]. An in vitro study demonstrated that patients with BMD less than 250 mg/cm3 bore high risk of fixation failure after intertrochanteric fractures [8]. However, this study used BMD measurements based on the whole-body scan. Patients graded as osteoporotic in those studies might appear to have a relatively lower BMD in the spine but a normal BMD in the hip. As a step towards establishing the definitive relationship between local bone density and clinical outcome, our study utilized local bone density instead of whole body values.
The subgroup analysis showed that local bone density was not associated with MF in the patients with good fracture reduction. The results did not differ when the patients were subgrouped by fracture pattern and types of implants. The similar results had been seen in the treatment of proximal humerus fractures and femoral neck fractures [26, 27]. Davis et al. found that bone density did not display significant influence on the cut-out rate of intertrochanteric fractures fixed by sliding hip screw or Küntscher Y-nail [14]. We were cautious to agree with the results for two possible reasons. One reason was that old designed implants used in the study might develop less intensity and toughness in their mechanical properties than the modern constructs did. The other reason was that these authors measured local BMD by Singh index which is a poor measure of bone density [28, 29].
Our study reported an overall high failure rate of 27.9 %, which is comparable to the recent literatures (20.5–37 %) [6, 7, 30]. However, other studies reported relatively lower rate of mechanical complications (8.8–13 %) [2, 14, 31]. We attributed the differences to our strict radiographic criteria. Unlike those studies, loss of reduction was documented in the present study as an additional form of mechanical complications. Furthermore, loss of reduction potentially included any visible movements in the bone–implant interface. We believe that, by the time displacement occurs, the loss of mechanical nature of the implants will lead to failure in the bone–implant interface. Thus, bone healing is no longer determined by primary fixation.
The implant is believed to bear more stress in unstable pertrochanteric fractures than in stable fractures before bone heals. Therefore, unstable fractures are potentially more likely to suffer failures in mechanical fixation [10, 30], as was supported by our findings. However, the results were not in agreement with those by Gardner et al. [19]. In their study, the authors found that fracture pattern did not exhibit a significant effect on blade tip movement. We explained the different results for the reason that fixation failure observed in the study only referred to the complications of the blades rather than all MFs observed on the radiographs.
Consistent with the results in recent studies [30, 32], our study showed that poor fracture reduction was an independent predictor for an increased failure risk. However, several studies documented conflicting results [6, 19]. Streubel et al. revealed a negative effect of fracture reduction on MF after locking plate fixation [6]. Besides, Gardner et al. did not investigate significant association between quality of reduction and blade failure [19]. The potential factor contributing to this discrepancy was the different methodology used. In those studies, the authors either fixed the fractures by locking plates or observed the failures only referring to blade complications.
As known, the TAD is an important predictor for cut-out of the screw or blade. The optimal tip–apex distance is 25 mm or less for a dynamic hip screw [8]. However, the TAD in the cut-out of the helical blade in PFNA shows a bimodal distribution, different to that of a sliding hip screw [33]. A recent study found that the TAD is not a potential predictor for cut-out in cephalomedullary nailing of proximal femoral fractures [31]. In the present study, we did not isolate patients with the screw or blade cut-out from those with other mechanical complications. It might be one possible explanation for non-correlation between the TAD and fixation failure.
One issue in this study deserves special mention. We used modern DXA to measure areal BMD (g/cm2) values at different areas of the hip. Although quantitative CT allows for a true three-dimensional bone density measurement (g/cm3) without superimposition of cortical bone and other tissues, the measurement of BMD obtained from DXA is the most widely used technique in the clinical setting because of its ease of use, low radiation exposure and its ability to measure BMD at both the hip and the spine [34]. In addition, areal BMD measured across an entire hip was then expressed as a T score to facilitate its interpretation for osteoporosis diagnosis [16]. Therefore, we believed DXA as a simple and reliable method for assessing local bone density in the unaffected hip in the clinical study. However, the quantitative CT-derived BMD sets the platform for which future studies can be based.
We acknowledge some limitations to the study. First, there was bias in the selection of the patients as 28 patients were excluded because of insufficient follow-up. Some patients with mechanical complications may have been managed at other institutions or did not require surgical intervention. There is also the possibility that a patient could suffer from fixation failure beyond the given follow-up period. Second, the evaluation of stability of the fractures was based on AO/OTA classification. Since the reliability of this classification was unknown, intraobserver or interobserver errors might appear during the evaluation. Third, as most of the measurements depended on radiographic analysis, the quality of radiographs might exert influence on the results. Rotational differences in x-ray position could lead to differences in the measurements of loss of reduction and blade migration of the screw or blade. Therefore, we used a relative value of 10 mm of migration and 10° of varus angulation as significant. Although the value was lack of evidence support, we finally achieve the ability to identify those dramatic complications.
To summarize, our findings demonstrated that local hip bone density does not appear to have a significant influence on MF after internal fixation of pertrochanteric fractures, whereas unstable fractures and poor reduction of the fractures may potentially predict increased failure risk. However, further randomized control trials are needed to support our results.
References
Park SR, Kang JS, Kim HS et al (1998) Treatment of intertrochanteric fracture with the Gamma AP locking nail or by a compression hip screw—a randomized prospective trial. Int Orthop 22:157–160
Herman A, Landau Y, Gutman G et al (2012) Radiological evaluation of intertrochanteric fracture fixation by the proximal femoral nail. Injury 43:856–863. doi:10.1016/j.injury.2011.10.030
Aros B, Tosteson AN, Gottlieb DJ et al (2008) Is a sliding hip screw or im nail the preferred implant for intertrochanteric fracture fixation? Clin Orthop Relat Res 466:2827–2832. doi:10.1007/s11999-008-0285-5
Yuan GX, Shen YH, Chen B et al (2012) Biomechanical comparison of internal fixations in osteoporotic intertrochanteric fracture. A finite element analysis. Saudi Med J 33:732–739
Matre K, Vinje T, Havelin LI et al (2013) TRIGEN INTERTAN intramedullary nail versus sliding hip screw: a prospective, randomized multicenter study on pain, function, and complications in 684 patients with an intertrochanteric or subtrochanteric fracture and 1 year of follow-up. J Bone Joint Surg Am 95:200–208. doi:10.2106/JBJS.K.01497
Streubel PN, Moustoukas MJ, Obremskey WT (2013) Mechanical failure after locking plate fixation of unstable intertrochanteric femur fractures. J Orthop Trauma 27:22–28. doi:10.1097/BOT.0b013e318251930d
Kim WY, Han CH, Park JI et al (2001) Failure of intertrochanteric fracture fixation with a dynamic hip screw in relation to pre-operative fracture stability and osteoporosis. Int Orthop 25:360–362
Konstantinidis L, Papaioannou C, Blanke P et al (2013) Failure after osteosynthesis of trochanteric fractures. Where is the limit of osteoporosis? Osteoporos Int 24:2701–2706. doi:10.1007/s00198-013-2392-8
Andruszkow H, Frink M, Fromke C et al (2012) Tip apex distance, hip screw placement, and neck shaft angle as potential risk factors for cut-out failure of hip screws after surgical treatment of intertrochanteric fractures. Int Orthop 36:2347–2354. doi:10.1007/s00264-012-1636-0
Wu CC, Tai CL (2010) Effect of lag-screw positions on modes of fixation failure in elderly patients with unstable intertrochanteric fractures of the femur. J Orthop Surg (Hong Kong) 18:158–165
Swiontkowski MF, Harrington RM, Keller TS et al (1987) Torsion and bending analysis of internal fixation techniques for femoral neck fractures: the role of implant design and bone density. J Orthop Res 5:433–444
Goh JC, Shah KM, Bose K (1995) Biomechanical study on femoral neck fracture fixation in relation to bone mineral density. Clin Biomech 10:304–308
Tingart MJ, Lehtinen J, Zurakowski D et al (2006) Proximal humeral fractures: regional differences in bone mineral density of the humeral head affect the fixation strength of cancellous screws. J Shoulder Elbow Surg 15:620–624. doi:10.1016/j.jse.2005.09.007
Davis TR, Sher JL, Horsman A et al (1990) Intertrochanteric femoral fractures. Mechanical failure after internal fixation. J Bone Joint Surg Br 72:26–31
Walsh ME, Wilkinson R, Stother IG (1990) Biomechanical stability of four-part intertrochanteric fractures in cadaveric femurs fixed with a sliding screw-plate. Injury 21:89–92
(2003) Osteoporosis: strategies for prevention and management. World Health Organ Tech Rep Ser 921:1–164
Koval KJ, Friend KD, Aharonoff GB, Zukerman JD (1996) Weight bearing after hip fracture: a prospective series of 596 geriatric hip fracture patients. J Orthop Trauma 10(8):526–530
Müller ENS, Koch P, Schatzker J et al (1990) The comprehensive classification of fractures of long bones. Springer, Berlin, pp 120–121
Gardner MJ, Briggs SM, Kopjar B et al (2007) Radiographic outcomes of intertrochanteric hip fractures treated with the trochanteric fixation nail. Injury 38:1189–1196. doi:10.1016/j.injury.2007.03.014
Baumgaertner MR, Curtin SL, Lindskog DM et al (1995) The value of the tip–apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am 77:1058–1064
Im GI, Shin YW, Song YJ (2005) Potentially unstable intertrochanteric fractures. J Orthop Trauma 19:5–9
Laros GS, Moore JF (1974) Complications of fixation in intertrochanteric fractures. Clin Orthop Relat Res 101:110–119
Laros GS (1975) Intertrochanteric fractures. The role of complications of fixation. Arch Surg 110:37–40
Larsson S, Friberg S, Hansson LI (1990) Trochanteric fractures. Mobility, complications, and mortality in 607 cases treated with the sliding-screw technique. Clin Orthop Relat Res 260:232–241
Bonnaire F, Weber A, Bosl O et al (2007) “Cutting out” in pertrochanteric fractures–problem of osteoporosis? Unfallchirurg 110:425–432
Kralinger F, Blauth M, Goldhahn J et al (2014) The influence of local bone density on the outcome of one hundred and fifty proximal humeral fractures treated with a locking plate. J Bone Joint Surg Am 96:1026–1032. doi:10.2106/JBJS.M.00028
Viberg B, Ryg J, Overgaard S et al (2014) Low bone mineral density is not related to failure in femoral neck fracture patients treated with internal fixation. Acta Orthop 85:60–65. doi:10.3109/17453674.2013.875360
Koot VC, Kesselaer SM, Clevers GJ et al (1996) Evaluation of the Singh index for measuring osteoporosis. J Bone Joint Surg Br 78:831–834
Hauschild O, Ghanem N, Oberst M et al (2009) Evaluation of Singh index for assessment of osteoporosis using digital radiography. Eur J Radiol 71:152–158. doi:10.1016/j.ejrad.2008.03.019
Liu W, Zhou D, Liu F et al (2013) Mechanical complications of intertrochanteric hip fractures treated with trochanteric femoral nails. J Trauma Acute Care Surg 75:304–310. doi:10.1097/TA.0b013e31829a2c43
Kashigar A, Vincent A, Gunton MJ et al (2014) Predictors of failure for cephalomedullary nailing of proximal femoral fractures. Bone Joint J 96(8):1029–1034. doi:10.1302/0301-620X.96B8.33644
Pervez H, Parker MJ, Vowler S (2004) Prediction of fixation failure after sliding hip screw fixation. Injury 35:994–998. doi:10.1016/j.injury.2003.10.028
Nikoloski AN, Osbrough AL, Yates PJ (2013) Should the tip–apex distance (TAD) rule be modified for the proximal femoral nail antirotation (PFNA)? A retrospective study. J Orthop Surg Res 17(8):35. doi:10.1186/1749-799X-8-35
Bansal SC, Khandelwal N, Rai DV et al (2011) Comparison between the QCT and the DEXA scanners in the evaluation of BMD in the lumbar spine. J Clin Diagn Res 5(4):694–699
Acknowledgments
We would like to thank Weiliang Wang M.D. and Debiao Zhou M.D. for the preparation of the manuscript, and Edem Prince Ghamor-Amegavi M.D. for valuable help in revising the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
The protocol involving human study has been approved by the institutional review board at our hospital and is in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
All participating patients signed written informed consents prior to entering the study.
Rights and permissions
About this article
Cite this article
Li, C., Xie, B., Chen, S. et al. The effect of local bone density on mechanical failure after internal fixation of pertrochanteric fractures. Arch Orthop Trauma Surg 136, 223–232 (2016). https://doi.org/10.1007/s00402-015-2369-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-015-2369-5