Abstract
Background
Iatrogenic vascular injury as a result of closed hip nailing is not common, but is a regularly reported complication after hip fracture surgeries.
Methods
To prevent vascular injury in closed hip nailing by identifying the range of distances and angles between deep and superficial femoral arteries (DFAs and SFAs) and distal screws.
Patients and methods
Forty subjects who underwent computed tomography angiographies were included in this study. Imaginary lines marking the distal screws (proximal femoral nail antirotation-II [PFNA-II], 180 and 300 mm; inter-trochanteric/sub-trochanteric nails [ITST], 200 and 300 mm) were drawn on the scout film. On arterial phase images, angles between distal screw lines and those marking DFAs or SFAs, as well as the distance between each artery and far cortex, were measured using the cross-reference capabilities of the picture archiving and communication system.
Results
The short nails (PFNA-II 200 mm and ITST 180 mm) were closest to the DFAs, indicating that these nails are most likely to cause injury (PFNA-II 200 mm: 11.2 ± 13.7° anterior and 9.87 ± 5.83 mm; ITST 180 mm: 22.56 ± 15.92° posterior and 9.24 ± 4.74 mm). The short nails were relatively distant from the SFAs, which were located posteriorly to the long nails (PFNA-II 300 mm and ITST 300 mm).
Conclusions
These data indicate that insertion of distal screws into intramedullary nails increases the risk of injury to vascular structures. Surgeons must take care in drilling or inserting screws to ensure the prevention of vascular injury.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Proximal femur fractures are one of the most common types of fracture. Due to the growing prevalence of osteoporosis coupled with prolonged life expectancy, the incidence of proximal femur fractures is expected to increase further in the future [1–4, 7, 8]. Internal fixation mediated by sliding hip screw or intramedullary (IM) nails are standard procedures in the treatment of proximal femur fractures. Iatrogenic vascular injury as a result of these procedures is not common, but is a regularly reported complication after hip fracture surgeries [5, 6, 9, 10, 12, 13]. Injury to the deep femoral artery (DFA) [5, 6, 9, 10], the superficial femoral artery (SFA) [12], or their branches may cause a compartment syndrome or form a large mass that requires additional treatments such as vascular surgery or excision. Despite regular reports detailing this complication, we could find only two studies, which have been conducted to prevent vascular injury following hip nailing: one cadaveric study [11] and one study which attempted to locate the position of the superficial femoral artery with color-flow duplex scanning [13]. Virtually no data exist with respect to the DFA, in which injuries are more frequently reported compared to the superficial femoral artery. Additionally, no correlation has yet been reported between the incidence of vascular injury with the position of distal screws and the deep or superficial femoral arteries. We therefore sought to identify the angles and distances that are likely to cause vascular injury after distal screw insertion in closed hip nailing and to suggest guidelines for preventing the injury.
The purpose of the study was to identify the following data in a Korean population: (1) The relationship between distal screws of proximal femoral IM nails and femoral arteries using lower extremity computed tomography (CT) angiography; and (2) The range of angles and distances within which injuries can be prevented during surgery. The ultimate objective of this study was to prevent vascular injuries during surgical procedures.
Materials and methods
Participants
Forty subjects (20 men and 20 women) who underwent CT angiography of the lower extremities in 2009 for evaluation of vascular lesion were included in this study. The mean age, height, and weight of the subjects were 68.9 years (range 63–74 years), 158.9 cm (range 150–170 cm), and 62.7 kg (range 53–80 kg), respectively. Exclusion criteria were a history of disease and/or trauma to the bone, bone deformities, and vascular lesion of femoral artery. The institutional review board at Yonsei University College of Medicine approved this study, and the requirement for informed consent was waived.
Images
Lower extremity CT angiography data were acquired by means of a LightSpeed VCT 64 (GE Healthcare, Milwaukee, WI) set to 100 kVp and 94 mAs with an image resolution of 0.4 mm/pixel and a slice thickness of 1.2 mm. Scout view and axial images of the arterial phase were used to measure the angles and distances from the superficial and deep femoral arteries to the distal screw position of the IM nail.
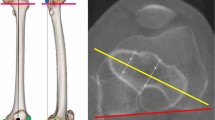
Positioning the distal screw of the IM nail on the CT scout image
Basic profiles of the IM nail were acquired. Proximal femoral nail antirotation-II (PFNA-II; Synthes, Solothurn, Switzerland) 200 and 300 mm, as well as Inter-trochanteric/sub-trochanteric nails (ITST; Zimmer, Warsaw, IN) 180 and 300 mm were used to measure the distance and angles between the distal screw and femoral arteries. The CT angiography scout images were used to predict the position of the distal screws on the anteroposterior (AP) plane (Fig. 1, right CT scout image). First, an imaginary line was drawn from the great trochanter tip to the IM canal, taking into consideration the lateral bowing of each nail. Second, a line was drawn for the blade (PFNA-II) or lag screw (ITST), which would fix the proximal part of femur. The angle between the blade or lag screw and the body of the IM nail was determined, and a line was drawn from the blade or lag screw in an attempt to pass through the nearly mid or mildly inferior portion of femoral neck and head. Third, a line was drawn connecting the distal screw of the static hole of each nail. Distances from the lateral entry point of the blade or lag screw to the distal screw were 83.5, 94, 200, and 223 mm in PFNAII 200 mm, ITST 180 mm, PFNA-II 300 mm, and ITST 300 mm, respectively (Figs. 1, 2, right images). The PFNA-II 200 mm distal screw line had an obliquity of 108° in the inferomedial direction, whereas the other distal screw lines were perpendicular to the IM nail bodies.
Angles and distances between distal screws of IM nails and DFAs or SFAs. Imaginary distal screws lines of IM nails were drawn on a scout image.  PFNAII 200 mm,
PFNAII 200 mm,  ITST 180 mm,
ITST 180 mm,  PFNAII 300 mm,
PFNAII 300 mm,  ITST 300 mm. Angles between distal screw lines and SFAs
ITST 300 mm. Angles between distal screw lines and SFAs  or DFAs
or DFAs  , and distances between the nearest femur shaft cortex and SFAs
, and distances between the nearest femur shaft cortex and SFAs  or DFAs
or DFAs  were measured on axial images of arterial phase using the cross reference system. IM intramedullary, DFA deep femoral artery, SFA superficial femoral artery, PFNA-II proximal femoral nail antirotation-II, ITST inter-trochanteric/sub-trochanteric nail
were measured on axial images of arterial phase using the cross reference system. IM intramedullary, DFA deep femoral artery, SFA superficial femoral artery, PFNA-II proximal femoral nail antirotation-II, ITST inter-trochanteric/sub-trochanteric nail
 –
– Schematic relationship of angles and distances between distal screw lines and DFAs or SFAs with nails of two different lengths. Endpoint is
Schematic relationship of angles and distances between distal screw lines and DFAs or SFAs with nails of two different lengths. Endpoint is  short nails or
short nails or  long nails, and relationship between perforating arteries and screws with DHS or short nails are also shown
long nails, and relationship between perforating arteries and screws with DHS or short nails are also shown  and
and  . DFA deep femoral artery, SFA superficial femoral artery, AV anteversion, TEA transepicondylar axis, PFNA-II proximal femoral nail antirotation-II, ITST inter-trochanteric/sub-trochanteric nail, DHS dynamic hip screw, PA perforating artery
. DFA deep femoral artery, SFA superficial femoral artery, AV anteversion, TEA transepicondylar axis, PFNA-II proximal femoral nail antirotation-II, ITST inter-trochanteric/sub-trochanteric nail, DHS dynamic hip screw, PA perforating artery
Assessment of angles and distances between distal screws and arteries on axial images
The left image of Fig. 1 shows the methods we used to measure the angles between the distal screw lines and the DFAs or SFAs, as well as the distances between the far cortex and the arteries on axial CT images of the arterial phase compared to scout films using the cross-reference capabilities of the picture archiving and communication system. The femoral neck and head anteversion of each patient compared to a transepicondylar line was first assessed. Considering the nail anteversion profile of the blade or lag screw (10° in PFNAI-II 200 and 300 mm, 0° in ITST 180 mm, and 15° in ITST 300 mm), a line for the distal screw that crossed the center of the IM canal was drawn and measured with the scout view using the cross-sectional reference system. Other lines were drawn that crossed the center of the IM canal and the DFAs or SFAs on the same axial image. Angles between the distal screw lines and the lines passing through the DFAs or SFAs were measured first. When an artery was located anteriorly to the distal screw lines, the angle was considered positive and when the artery was located posteriorly, the angle was considered negative. The distance between each artery and the femur shaft cortex nearest to each artery (the far cortex) was measured and recorded. The distances and angles between the distal screws lines and DFAs or SFAs were measured for the short nails (PFNA-II 180 mm and ITST 200 mm) and the relationship between the distal screws lines and SFAs were assessed for the long nails (PFNA-II 300 mm and ITST 300 mm). In addition to measuring the angles and distances, the distances from the perforating artery and the blades or lag screw entry points of the IM nails were also assessed.
An orthopedic surgeon with 6 years of experience (KKP) and a musculoskeletal radiologist with 5 years of experience (YHL), both of whom were unaware of all clinical information, reviewed the CT images. Each clinician was blinded to the assessments of the other clinician, and measured each angle and distance twice at an interval of 3 weeks with the subject data being reviewed ordered randomly.
Statistical analysis
Statistical analysis was performed using the SPSS for Windows statistical package (version 15.0, SPSS, Chicago, IL) and a p value <0.05 was considered significant. All data are summarized as mean ± standard deviations (SDs) along with the range of values. Intraclass correlation coefficients and 95 % confidence intervals were calculated to determine intra- and interobserver reliabilities. Student’s t test was used to compare the ratios between male and female subjects.
Results
The mean femoral neck anteversion compared to the transcondylar line was 12.12 ± 8.03° (range −7.5 to 22.2). Perforating arteries around the proximal femur area were located 63.16 ± 12.12 mm (range 42.1–78.9) proximally and 110.05 ± 19.67 mm (range 81.2–135.4) distally from the starting point of the proximal screws of the IM nails (Fig. 2c, d).
With respect to the short nails, the mean angles between the distal screw lines and DFAs and mean distances between the far cortex and DFAs were 11.2 ± 13.7° and 9.87 ± 5.83 mm in PFNA-II 200 mm and −22.56 ± 15.92° and 9.24 ± 4.74 mm in ITST 180 mm, respectively (Table 1). For the SFAs, the mean angles and distances were 28.09 ± 8.87° and 27.81 ± 5.21 mm with PFNA-II 200 mm, respectively, and 16.00 ± 8.45° and 27.27 ± 5.69 mm with ITST 180 mm, respectively (Table 1). With respect to the long nails, the mean angles between the distal screw lines and SFAs and the mean distances between the far cortex and SFAs were 32.96 ± 16.10° and 22.85 ± 4.86 mm in PFNA-II 300 mm and 38.45 ± 17.76° and 19.28 ± 3.44 mm in ITST 300 mm, respectively (Table 1). The interobserver and intraobserver measurements demonstrated reliable agreement. The intraclass correlation coefficients were 0.888–0.991 [95 % confidence intervals (CI) 0.722–0.997] for interobserver reliabilities and 0.928–0.993 (95 % CI 0.821–0.997) for interobserver reliabilities.
The angles between the distal screw lines and SFAs, as well as the distances between the far cortex and DFAs or SFAs, were significantly different in males compared to females (Table 2). However, no significant differences were evident in the angles between distal screw lines and DFAs in male compared to female subjects (Table 2).
Discussion
The purpose of this study was to prevent vascular injury by identifying the range of distances and angles within which the distal screw used in closed hip nailing may cause vascular injury. We found that with short nails, the distal screw was the closest to the DFAs, indicating that a short nail is most likely to cause injury. The SFAs were located relatively distant from the short nail and located posteriorly to the long nails, indicating long nails were less likely cause injury. However, caution is necessary to prevent injury to the SFAs as well, as their position may be altered by traction, adduction, and rotation of the femur during surgery. Moreover, the possibility of injury cannot be eliminated during the deep insertion of a drill bit.
There are some limitations in the design of this study. First, the measurements were performed on CT images taken with the subject in the supine position. As mentioned above, the position of the SFAs and DFAs can be affected when the lower leg of the patient undergoes traction, adduction, and internal rotation during surgery. However, it is practically impossible to take a CT image with the subjects in the operating position. Additionally, because the purpose of this study was to assess the relationship between the distal screw in IM nails and the vascular structure, we designed the study accordingly, despite the associated limitations. Such limitations are partly addressed by the findings from Yang et al. [13], who used the color-flow duplex scanning method to measure the distance between the femur and SFAs decreased by approximately half when adduction alone or both adduction and internal rotation were applied. Applying these results to our findings led to the conclusion that the distance between the far cortex and vascular structures further decreases during surgery, and therefore increases the risk of injury to vascular structures.
A second limitation is, because this is a study based on images, the safe angles and distances of the current study could be different in real operations. However, the primary goal of this study was to investigate the correlation between the distal screws and the position of DFAs and SFAs. We therefore think the results of this study are meaningful for predicting the incidence of arterial injury through the simulation of nail insertion, instead of merely identifying anatomic knowledge.
A third limitation is that this study was based on data collected from only Korean subjects, and only short nails used in Asian subjects were investigated. Because this study involved nails commonly used for Korean patients, we believe that nails used on Caucasian patients are required to apply these findings to Caucasians. Finally, the results of this study are limited to the static locking hole because we have used the static rather than dynamic locking hole in operating on elderly patients with severe osteoporosis. However, consideration must be taken when it comes to the dynamic locking hole: its position is different from that of the static locking hole and the hole through which a screw can be inserted is wider.
Despite these limitations, we performed this study because injury to the femoral artery after closed hip nailing has been regularly reported and there is a lack of systematic research investigating vascular injury due to this procedure. We chose to investigate DFAs and SFAs because of recent injury reports in SFAs that may lead to fairly severe complications. Although the results of the previous study by Yang et al. are meaningful because they report the practical relationship between the femur and SFAs, that study was limited to measurements involving the SFAs and did not report angle measurements. We expect that this current study will deliver important, novel data that will contribute significantly to the field.
We sought to report clinically practical data in order to aid surgeons in identifying distances and angles that may cause arterial injuries due to drilling or distal screw insertion. Figure 2 summarizes our findings, indicating that careful attention is required to prevent injuries to DFAs when using short nails (Fig. 2a). The anteversion of the PFNA-II 200 mm blade itself is 10°, resulting in the 10° angle between the distal screw lines, and the angle with DFAs further decreases, requiring additional caution. Passing from proximal to distal parts, the SFAs are shifted from the anterior to the posterior part of the thigh (Fig. 2). According to our data, the SFAs were located approximately 20–30 mm from the femoral far cortex (Fig. 2b). However, because the SFAs are located medially in mid part of the thigh and adduction or the combination of adduction and internal rotation may decrease the distance between the nail and SFA, caution is critical to avoid injury when using a medium-sized nail.
In addition to DFAs and SFAs, we collected data on the perforating arteries. These arteries were located 63.16 ± 12.12 mm (range 42.1–78.9) and 110.05 ± 19.67 mm (range 81.2–135.4) distally from the insertion point of the blade or lag screw (Fig. 2c, d). With short nails, the distal screw was located 83 mm (PFNA-II 200 mm) or 94 mm (ITST 200 mm) distally from the insertion point of the blade or lag screw. Therefore, injury is still possible when using short nails. In particular, because the position of the perforating arteries is close to the femoral far cortex area, drilling must be performed with extreme caution. Additionally, the frequently used 135° four-hole dynamic hip screw (DHS; Synthes) involves screw holes at 24, 40, 55, and 71 mm from the hip screw insertion point. As shown in Fig. 2, cautious drilling is required during the insertion of the third and fourth distal screws in order to prevent damage to the proximal perforating artery.
When data from male and female subjects were compared, significant differences with respect to the distances between the far cortex and the DFAs or SFAs were identified (Table 2). These differences are probably due to the smaller overall size of women compared to men (164.5 ± 6.53 vs. 153.3 ± 4.38, p value <0.001 in height and 65.7 ± 7.45 vs. 59.9 ± 5.53, p value = 0.03 in weight). Interestingly, there were no significant differences between male and female subjects with respect to the angles between the distal screw lines and the DFAs. In contrast, the SFAs were located significantly posteriorly to the distal screw lines in both short and long nails in female subjects compared to males (Table 2). We hypothesize that these discrepancies are due to differences in the length of the thigh, as the SFAs pass more posteriorly in the proximal area in women compared to men. In short, the femoral arteries are closer to the femur in women compared to men, indicating that more careful drilling is critical to prevent injury in female patients.
This study provides practical guidelines for preventing vascular injury in Korean patients following closed hip nailing. As significant patient variation exists and rotations are performed in a variety of postures for satisfactory reduction during surgery, it is difficult to formulate clear guidelines to completely eliminate the risk of vascular injury. However, our data suggest that the insertion of distal screw in IM nails likely increases the risk of injury to vascular structures. Therefore, surgeons must take great care in drilling or inserting screws to ensure that vascular injury does not occur.
References
Cooper C, Melton LJ 3rd (1992) Epidemiology of osteoporosis. Trends Endocrinol Metab 3:224–229
Cooper C, Campion G, Melton LJ 3rd (1992) Hip fractures in the elderly: a world-wide projection. Osteoporos Int 2:285–289
Cooper C, Atkinson EJ, Jacobsen SJ, O’Fallon WM, Melton LJ 3rd (1993) Population-based study of survival after osteoporotic fractures. Am J Epidemiol 137:1001–1005
Cooper C, Cole ZA, Holroyd CR, Earl SC, Harvey NC, Dennison EM, Melton LJ, Cummings SR, Kanis JA (2011) Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int 22:1277–1288
Ebong WW (1978) False aneurysm of the profunda femoris artery following internal fixation of an intertrochanteric femoral fracture. Injury 9:249–251
Fordyce A (1968) False aneurysm of the profunda femoris artery following nail and plate fixation of an intertrochanteric fracture. Report of a case. J Bone Jt Surg Br 50:141–143
Johnell O, Cooper C, Melton LJ 3rd (1993) How do we prevent hip fractures? Lancet 341:89
Kanis JA, Black D, Cooper C, Dargent P, Dawson-Hughes B, De Laet C, Delmas P, Eisman J, Johnell O, Jonsson B, Melton L, Oden A, Papapoulos S, Pols H, Rizzoli R, Silman A, Tenenhouse A (2002) A new approach to the development of assessment guidelines for osteoporosis. Osteoporos Int 13:527–536
Karanikas I, Lazarides M, Arvanitis D, Papayanopoulos G, Exarchou E, Dayantas J (1993) Iatrogenic arterial trauma associated with hip fracture surgery. Acta Chir Belg 93:284–286
Karkos CD, Hughes R, Prasad V, D’Souza SP (1999) Thigh compartment syndrome as a result of a false aneurysm of the profunda femoris artery complicating fixation of an intertrochanteric fracture. J Trauma 47:393–395
Riina J, Tornetta P 3rd, Ritter C, Geller J (1998) Neurologic and vascular structures at risk during anterior-posterior locking of retrograde femoral nails. J Orthop Trauma 12:379–381
Yang KH, Park HW, Park SJ (2002) Pseudoaneurysm of the superficial femoral artery after closed hip nailing with a Gamma nail: report of a case. J Orthop Trauma 16:124–127
Yang KH, Yoon CS, Park HW, Won JH, Park SJ (2004) Position of the superficial femoral artery in closed hip nailing. Arch Orthop Trauma Surg 124:169–172
Acknowledgments
We thank to Dong-Su Jang for graphic help and Hee Yeon Lee for data organization.
Conflict of interest
This work was supported by Yonsei University Research Fund (No. 7-2011-0753) which was funded by Korean Institute of Medicine.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Han, C.D., Lee, Y.H., Yang, K.H. et al. Relationship between distal screws and femoral arteries in closed hip nailing on computed tomography angiography. Arch Orthop Trauma Surg 133, 361–366 (2013). https://doi.org/10.1007/s00402-012-1674-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-012-1674-5