Abstract
Background
MRI is the current pre-operative imaging standard in recurrent anterior shoulder instability; however, CT has increasingly gained interest due to its advantages in the detection of bony glenoid defects. This study compares the value of CT imaging and MRI for pre-operative surgical planning in recurrent anterior shoulder instability.
Methods
Between 2006 and 2009, 83 patients presented to the author’s department with recurrent anterior shoulder instability. For 48 patients, both, pre-operative MRI and CT images were available. The respective patho-morphological descriptions were retrospectively compared with the intra-operative findings. The effect of each imaging technique on the pre-operative surgical planning was analyzed and the accuracy in predicting the necessity of open versus arthroscopic surgery was compared.
Results
In determining the necessity of open versus arthroscopic surgery CT imaging rendered an inaccurate prediction in 4.8 % of the cases which is less than the 25.0 % calculated for MRI. (p = 0.019). MRI showed a low sensitivity (35.3 %) in the detection of significant glenoid bone defects (≥20 % of the glenoid width measured on en-face views using a best-fit circle technique) while CT imaging provided an accurate prediction of the intra-operative finding in all cases.
Conclusion
Despite the advantages of MRI in the detection of soft tissue damages in recurrent anterior shoulder instability CT imaging proved to be more important for pre-operative planning by prevailing in the detection of glenoid defects. Therefore, the replacement of MRI as preoperative imaging standard with CT imaging is recommended.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Anterior shoulder instability is a musculoskeletal pathology of traumatic or atraumatic origin which commonly affects young adults and leads to discomfort and limitation of participation in high-level activities [26]. While a patient presenting with first-time anterior shoulder dislocation can be treated non-operatively or surgically [13], recurrent anterior shoulder instability is generally addressed surgically. The current pre-operative standard imaging algorithm for patients presenting with recurrent anterior shoulder instability at clinical examination is composed by magnetic resonance imaging (MRI) for detection of labral damage or other accompanying soft tissue injuries [29] in addition to a conventional radiographic imaging series at least including a true anteroposterior and axillary lateral view of the gleno-humeral joint [8].
Labral damage in its various forms represents the central pathology in gleno-humeral instability [18] and is found in nearly all cases of recurrent anterior shoulder instability [39]. Despite the common pre-operative evaluation with MRI (native or MR-arthrography), labral integrity is still best assessed intra-operatively. In case labral damage is detected, open or arthroscopic Bankart repair techniques can be performed with the latter increasingly gaining favor [27]. Another major factor for shoulder stability is the bony integrity of the glenoid. According to Yamamoto et al. [38] a glenoid defect in the 3 o’clock position with a width of 6 mm or more significantly decreases the anterior stability of the affected shoulder. Undetected damage to the glenoid rim has been described as the leading reason for recurrence of instability after surgical stabilization [6, 37]. While mere fractures of the glenoid or bony Bankart lesions with clearly visible fragment are easy to identify, intra-operative detection of glenoid damage can be difficult when attritional bone loss is present [37] or the fragment is hidden within the capsulo-labral soft tissue complex [35]. Therefore, it is of major importance to detect and quantify bony glenoid defects pre-operatively using cross sectional imaging techniques [8]. Whenever the defect is significant, open surgical intervention with bony augmentation instead of arthroscopic Bankart repair is required [8]. Thus, pre-operative cross-sectional imaging represents a criterion of utmost importance for surgical planning. Due to the disadvantages of MRI in bone imaging [33], lately, computed tomography (CT) imaging has increasingly been employed in pre-operative assessment of recurrent anterior shoulder instability for the detection and quantification of glenoid bone damage [1, 10, 12]. In case of attritional bone loss, several different methods have been described and validated to estimate the extent of the missing anterior glenoid rim using CT imaging [11, 20, 24, 35].
CT scans in the pre-operative imaging routine for patients with recurrent anterior shoulder instability facilitate the detection of bony glenoid damage and help to decide whether open bone augmentation surgery instead of an arthroscopic Bankart repair is needed. The immediate benefit of pre-operative MRI to determine labral damage appears limited since it is present in nearly all cases of recurrent anterior shoulder instability [39], is best detectable intra-operatively, and addressable during both, open or arthroscopic surgery. We hypothesized that a pre-operative CT scan instead of MRI is sufficient for efficient surgical planning in patients presenting with recurrent anterior shoulder instability upon clinical examination. To investigate this hypothesis the influence of MRI and CT imaging on the surgical treatment plan for patients with recurrent anterior shoulder dislocations is retrospectively analyzed in this study.
Methods
Over the course of 3.5 years (2006 until 2009) 83 patients were surgically treated at the author’s institution for recurrent anterior shoulder instability. Due to the above-explained reasons we established CT scanning with three-dimensional reconstruction of the glenoid (a so called “en-face”-view) as routine pre-operative imaging in addition to radiographic evaluation including a true a.p.- and axillary lateral view of the affected shoulder. Even though MR imaging is not performed as standard prior to surgery at the author’s institution anymore, a great percentage of the patients referred to our tertiary care institution by other physicians had already MR imaging. The inclusion criteria for this retrospective study were (1) history of recurrent anterior shoulder instability, including failed prior arthroscopic or open stabilization surgery; and (2) complete pre-operative MRI and CT-scans with 3D-reconstruction of the glenoid. Thus, 48 patients were included in this study.
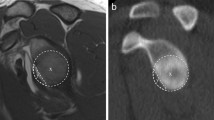
All available MRIs and CT-scans were re-evaluated for study purposes in a blinded fashion by the same musculo-skeletal radiologist. Pathological findings were listed and compared with the intra-operatively described patho-morphological findings documented on the surgical report. Analyzed findings included labral damage, significant bony glenoid defects (≥20 % of the glenoid width measured according to Sugaya et al. [34, 35] on 3D “en face” CT or parasagittal “en face” MRI images), Hill-Sachs lesions, humeral avulsions of the gleno-humeral ligament (HAGL), capsular insufficiency or redundancy, rotator cuff lesions, and superior labral anterior to posterior (SLAP) lesions.
All cases in which open surgery was chosen over arthroscopy were reviewed for the reason triggering this decision to analyze the possible influence of either imaging technique on pre-operative surgical planning. To analyze the accuracy of MRI and CT imaging in predicting whether an arthroscopic treatment approach would be sufficient or open surgery would be required, the treatment recommendation drawn from the results of either imaging technique in awareness of the patient history and clinical examination was compared with the treatment the patients ultimately received based on patient history, examination, CT, MRI, and intra-operative findings. Additionally, the medical history of all patients was reviewed regarding the cause of the shoulder instability, time elapsed since the first dislocation, number of instability episodes, previous surgical treatment, and affection of the contralateral shoulder.
Imaging modalities
All CT scans included multiple planes (axial, parasagittal, paracoronal and three-dimensional reconstruction) and were obtained at the author’s institution prior to surgery using a 64-slice CT scanner (Siemens Somatom Sensation 64, Siemens, Erlangen/Germany). MR images were obtained by the patients at 23 different radiological institutions. All images used for evaluation were generated with at least 1.5 T devices and included multiple planes (axial, parasagittal, and paracoronal) and at least two different sequences.
Surgical treatment
All 48 patients included in the present study underwent surgical stabilization at the author’s institution. All shoulder stabilization surgeries were performed in beach chair position under general anesthesia in combination with an interscalene nerve block. A standard arthroscopic capsulo-labral repair is performed to treat labral lesions. A posterior, antero-superior and antero-inferior portal has been used. Bony Bankart lesions with a significant fragment size have been addressed by arthroscopic or open screw fixation to restore the bony anatomy of the anterior glenoid rim.
Bone loss of the anterior glenoid exceeding 20 % of the glenoid width measured using the technique described by Sugaya et al. [34, 35]. on the socalled “en-face” view of the glenoid was deemed significant. Bony deficiency included complete bone loss at the anterior glenoid rim as well as those cases with a partially absorbed, medialized Bankart fragment. Surgical treatment was open bone grafting either using a J-bone graft [3], or a Latarjet procedure [40]. Concomitant soft tissue structural damages of the shoulder encountered during surgery such as capsular insufficiency or rotator cuff lesions are treated during both, arthroscopic or open surgery, depending on the operative-setting chosen. Exceptions are HAGL lesions which at our institution are only treated using open surgery and SLAP lesions which are preferably addressed arthroscopically.
Statistics
The statistical analysis was conducted using the Pearson’s Chi Square Test with the alpha level set to 0.05 and all p values being two tailed. If a contingency table contained cells with a value below 5 the Fisher’s Exact Test was utilized.
Results
Of the 48 patients included in this study 8 were females and 40 were males. The average age at the time of surgery was 30.8 years ranging from 20 to 78 years. In 81.3 % of the cases the recurrent shoulder instability resulted from a trauma, 14.6 % had an atraumatic instability, and 4.2 % an epileptic seizure. The number of experienced instability episodes ranged from 2 to 24 with an average of 9.1 episodes. In 23 patients the right shoulder was affected, in 20 patients the left shoulder, and 5 patients showed bilateral shoulder instability. The mean time elapsed between the first instability episode and the index procedure was 3 years with a range from 0.3 to 10 years. (Table 1) Seven patients presented with failed stabilization surgery (5 of them with arthroscopic Bankart repair, 2 with open Bankart repairs). As index procedures the following techniques have been performed: arthroscopic Bankart repairs (24), J-bone grafting (13), Latarjet procedure (2), HAGL repair (2), open bony fragment fixation (2), Eden-Hybinette procedure (1), open Bankart repair (1), capsular shift (2), and arthroscopic bony fragment fixation (1). The average time elapsed between imaging and surgery was 78.4 days for MRI (range 8–330) and 25.8 days for CT (range 1–133).
The most common intra-operative pathomorphological finding was labral damage (91.7 %), followed by Hill Sachs lesion (89.6 %), significant bony defect of the anterior glenoid (35.4 %), and capsular insufficiency (35.4 %) (Table 1). Pre-operative CT imaging had a sensitivity of 100 % for significant bony defects of the glenoid, while MRI only reached 35.3 %. The negative predictive value (NPV) of pre-operative MRI in the detection of significant bony glenoid defects was 73.8 % compared with the 100 % NPV of CT imaging. Both imaging techniques showed high sensitivity (CT 95.3 %, MRI 86.0 %) and specificity (CT 80.0 %, MRI 80.0 %) in the detection of Hill-Sachs lesions. While CT imaging rendered no information about damage to soft tissue structures of the shoulder, MRI had a high sensitivity and specificity for labral damage (90.9 and 75.0 %), rotator cuff tears (100 and 93.3 %), and a mediocre sensitivity for SLAP lesions (66.7 %), HAGL lesions (50.0 %), and capsular insufficiency (58.8 %). The positive predictive value for rotator cuff tears (50.0 %) was the lowest of all pathomorphological findings analyzed (Table 2).
The pre-operative planning to perform an open surgery was determined by findings of significant bony damage to the glenoid only detected in the CT images in 55.0 % of the cases, bony damage to the glenoid detected with both imaging techniques in 25 %, patient history of multiple failed previous surgeries in 15.0 %, and MRI evidence of HAGL lesions in 5.0 % (Fig. 1).
In predicting the need of open versus arthroscopic surgery pre-operative CT imaging rendered an inaccurate prediction in 4.8 % of the cases which is statistically significantly lower than the 25.0 % calculated for MRI (p = 0.019). A surgical plan merely based on the MRI findings would have resulted in 11 patients (22.9 %) being at least initially treated arthroscopically despite the presence of a significant bony defect of the glenoid and the necessity of open bone augmentation surgery. Vice versa, if only relying on CT findings for pre-operative planning two patients (4.2 %) would have at least initially been treated arthroscopically despite the need for open surgical repair of a HAGL lesion (Fig. 2).
Discussion
The use of MRI for pre-operative evaluation of recurrent anterior shoulder instability is widely accepted as imaging standard [29]. However, pre-operative CT imaging has gained interest due to the increasing awareness of undetected and untreated bony defects of the glenoid as a major factor for unsuccessful surgical stabilization [6, 37]. The purpose of this study was to evaluate the benefit and effectiveness of both imaging techniques in pre-operative surgical planning of recurrent anterior shoulder instability.
In contrast to CT imaging, MRI represents the gold standard to detect soft tissue injuries such as labral damage which represents the main factor in shoulder instability [39]. Given that labral damage is best assessable intra-operatively, the use of MRI for its pre-operative prediction seems to be redundant especially since according to our and other reported results [39] labral damage is present in nearly all patients who have clinically been diagnosed with recurrent anterior shoulder instability. The value of MRI in the pre-operative prediction of labral damage further diminishes when considering the 17 % chance for false-negative results reported in a recent study involving 3 T-MRI [21] and the low NPV found in the present study (42.9 %). In general, the capability of MRI in the evaluation of soft tissue injuries such as labral damage, capsular insufficiency, rotator cuff tears, or SLAP lesions is an apparent advantage over CT at first sight. However, according to our data, only the pre-operative detection of a HAGL lesion using MRI had an effect on the surgical planning because its repair required open surgery. In 80 % of the cases only the glenoid rim integrity determined the necessity of an open surgery since the concomitant soft tissue damages were addressable using both, arthroscopic or open surgery. Considering that HAGL lesions were only found in 4.2 % of the cases (which is still more than the 1.2 % prevalence reported elsewhere [39]) and MRI showed to have a limited sensitivity (50 %), and in another report even specificity [22] for the detection of a HAGL lesion the immediate necessity and value of pre-operative MRI evaluation of soft tissue injury in the case of recurrent anterior shoulder instability becomes questionable.
As expected CT imaging proved to have much higher sensitivity and specificity than MRI in the detection of bony defects of the humeral head (Hill-Sachs lesions) or the glenoid. Hill-Sachs lesions can cause recurrent instability sensation after surgical repair, whenever an engagement of the humeral bony defect and the anterior glenoid rim occurs in abduction and external rotation [6]. The pre-operative prediction of this engagement using CT imaging has recently been described by Cho et al. [9] and could be an additional benefit of pre-operative CT imaging in anterior shoulder instabilities. However, intra-operative verification of an occurrence of engagement still seems to be the easiest and most commonly used method.
As mentioned above, the finding of a significant bony glenoid defect accounted for 80 % of all decisions to perform an open surgery instead of arthroscopy. Considering the fact that missed glenoid rim defects are the primary cause of recurrence after surgical stabilization [37], pre-operative CT imaging seems to be an indispensable tool in drawing up the correct surgical treatment plan as already indicated by Burkhart et al. in a recent study [10]. In case attritional glenoid bone loss is present or the bony fragment is not visible due to medialization and soft tissue coverage [36], the intra-operative assessment can be difficult making it a frequently missed and untreated entity [6, 37]. Due to the unavailability of the contralateral side for comparison purposes, the intra-operative assessment of glenoid bone loss is usually performed using the bare spot method [5, 7] which, however, when applied in practice is associated with some limitations. First, the consistent position of the bare spot in the exact center of the glenoid is still under debate [16] and in some patients a bare area rather than a bare spot is present limiting its applicability as a reference point for measurement purposes [12]. Second, the calibrated probe inserted through the posterior portal needs to be aligned exactly perpendicularly to the long axis of the glenoid to avoid underestimation of glenoid bone loss [12]. Third, sometimes it can be difficult to arthroscopically count the millimeter-spaced lines along the calibration probe [23]. Therefore, to avoid misdiagnosis and mistreatment, glenoid bone loss should be assessed pre-operatively, as suggested by Bushnell et al. [8] in a recent current concepts article. In order to adequately plan surgical shoulder stabilization and to pre-operatively inform the patient about open or arthroscopic procedure, it is crucial to know about the presence of a significant anterior glenoid bone loss. Even if arthroscopic techniques of anterior glenoid bone grafting have been described [17, 30], this kind of procedure is a domain of open surgery at the present time. In contrast, all concomitant soft tissue injuries found in recurrent anterior shoulder instability as rotator cuff lesions, SLAP lesions, and capsulo-ligamentous laxity can be addressed arthroscopically and would not require an intra-operative switch from arthroscopy to open surgery, if not detected in the pre-operative field. Thus, despite the patient’s exposure to a certain amount of radiation, the preferred imaging method should be CT imaging rather than MRI. In addition to a higher sensitivity and specificity in the evaluation of glenoid damage, further arguments are lower cost, greater availability in many institutions, and the shorter imaging time which is especially welcomed by patients suffering from claustrophobia. Finally, metal implants in proximity to the focus area (which can often be the case in revision surgery) or MRI-incompatible devices in general [19] do not contraindicate CT examination.
SLAP lesions and rotator cuff tears are often more easily addressed arthroscopically than during open surgery. In general, SLAP lesions or rotator cuff tears can be assessed during clinical examination with the latter typically being more common in older patients. If the clinical examination suggests a concomitant soft tissue damage such as a rotator cuff tear and the treating surgeon wishes further pre-operative evaluation, sonography of the shoulder can be performed which typically is readily available [31], of high cost-effectiveness [31], and was proven to have high sensitivity (94 %) and specificity (94 %) in the detection of rotator cuff tears [28]. Alternatively, a CT arthrogram instead of mere CT imaging can be taken into consideration, which has been shown to have high sensitivity and specificity in the detection of both bony lesions and soft tissue injuries [25, 41]. MR arthrography has even higher sensitivity and specificity in the detection of soft tissue damage than MRI [21]; however, its sensitivity in the detection of bony glenoid damage is still rather low at 67 % [4]. Similar to CT arthrography, it is not always available and carries some risks including infection, bleeding, synovitis, allergy to the contrast media, delayed pain reaction due to capsule distension [33], and avascular necrosis of bones adjacent to the injected joint [14].
The fact that pre-operative CT imaging prevailed over MRI in predicting the necessity of open or arthroscopic surgery which ever was found to be adequate by the surgeon who had a synopsis of the MRI, CT, and intra-operative findings suggests that standard pre-operative CT imaging instead of MRI in patients with recurrent anterior shoulder instability not only could lower the recurrence rate by improving the detection of glenoid bone loss but also optimize surgical planning. Obviously, MRI still offers advantages in terms of pre-operative detection of concomitant soft tissue injuries which might be of interest for patient counseling; however, according to the findings of this study it should only be considered in the pre-operative imaging algorithm of recurrent anterior shoulder instability whenever the clinical examination indicates a tear of the rotator cuff or a SLAP lesion. According to these findings we propose the imaging algorithm shown in Fig. 3. In the case of an isolated HAGL lesion pre-operative CT imaging is of none and native MRI is of limited value due to its low sensitivity in addition to the low prevalence of the pathology itself.
A limitation of this study is that some of the results are determined by the surgical standards at our institution regarding the indication for open versus arthroscopic surgery and cannot directly be adopted by every other orthopedic department without proper adaptations. However, we believe that the standards at our institution reflect a surgical standard widely established in most orthopedic tertiary care centers, even though lately some successful attempts have been made to arthroscopically treat significant bone loss of the glenoid [17, 30] or HAGL lesions [15, 32] and some authors prefer to perform diagnostic arthroscopy prior to every open bone augmentation for further evaluation of the shoulder joint [2]. Another limitation of our study is that at the time of intra-operative evaluation of structural damages of the shoulder joint the surgeon was fully aware of the MRI and CT findings which could potentially have influenced the intra-operative assessment. As mentioned above, intra-operative glenoid assessment can be difficult and sometimes misleading. Therefore, surgeons intra-operatively often rely on the 3D CT measurements of the glenoid obtained before surgery. This explains the 100 % sensitivity and specificity of CT imaging in the detection of significant glenoid bone loss, but at the same time underlines the importance of pre-operative CT imaging. The fact that MRI images were obtained from 23 different institutions adds another limitation to this study since many different imaging modalities were used which raises concern for poor image quality and plane alignment in some cases. Due to the reason that MR images were obtained by the patients prior to the first visit at our department, the average time elapsed between MRI and surgery was longer than the average time between CT and surgery. This might have distorted the results in cases of redislocation and possible additional structural damage after MRI and before surgery. All MRI and CT images were assessed by a single radiologist for pathomorphological findings and no inter- or intraobserver reliability calculations were carried out. A further limitation might be the fact that the surgical treatment plan for the study patients was determined by four different surgeons; however, all treatment decisions were made according to the guidelines issued by the chairman of the department. Finally, it must be mentioned that the accuracy of the surgical treatment the patients eventually received can be disputed since there was no follow-up of the outcome; however, in all cases the treatment relied on the assessment of experienced surgeons based on a synopsis of all available findings including CT, MRI, patient history, and clinical examination.
Conclusion
Despite the advantages of MRI in the evaluation of soft tissue injuries, CT imaging seems to be sufficient and more effective in the pre-operative surgical planning in case of recurrent anterior shoulder instability.
References
Abboud JA, Armstrong AD (2011) Management of anterior shoulder instability: ask the experts. J Should Elb Surg 20(2):173–182
Arrigoni P, Huberty D, Brady PC, Weber IC, Burkhart SS (2008) The value of arthroscopy before an open modified latarjet reconstruction. Arthroscopy 24(5):514–519
Auffarth A, Schauer J, Matis N, Kofler B, Hitzl W, Resch H (2008) The J-bone graft for anatomical glenoid reconstruction in recurrent posttraumatic anterior shoulder dislocation. Am J Sports Med 36(4):638–647
Bitzer M, Nasko M, Krackhardt T et al (2004) Direct CT-arthrography versus direct MR-arthrography in chronic shoulder instability: comparison of modalities after the introduction of multidetector-CT technology. Rofo 176(12):1770–1775
Burkhart SS (2007) The bare spot of the glenoid. Arthroscopy 23(4):449 author reply 449–450
Burkhart SS, De Beer JF (2000) Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 16(7):677–694
Burkhart SS, Debeer JF, Tehrany AM, Parten PM (2002) Quantifying glenoid bone loss arthroscopically in shoulder instability. Arthroscopy 18(5):488–491
Bushnell BD, Creighton RA, Herring MM (2008) Bony instability of the shoulder. Arthroscopy 24(9):1061–1073
Cho SH, Cho NS, Rhee YG (2011) Preoperative analysis of the Hill-Sachs lesion in anterior shoulder instability: how to predict engagement of the lesion. Am J Sports Med 39(11):2389–2395
Chuang TY, Adams CR, Burkhart SS (2008) Use of preoperative three-dimensional computed tomography to quantify glenoid bone loss in shoulder instability. Arthroscopy 24(4):376–382
Griffith JF, Antonio GE, Tong CW, Ming CK (2003) Anterior shoulder dislocation: quantification of glenoid bone loss with CT. Am J Roentgenol 180(5):1423–1430
Griffith JF, Yung PS, Antonio GE, Tsang PH, Ahuja AT, Chan KM (2007) CT compared with arthroscopy in quantifying glenoid bone loss. Am J Roentgenol 189(6):1490–1493
Handoll HH, Almaiyah MA, Rangan A (2004) Surgical versus non-surgical treatment for acute anterior shoulder dislocation. Cochrane Database Syst Rev (1):CD004325
Hodler J (2008) Technical errors in MR arthrography. Skeletal Radiol 37(1):9–18
Kon Y, Shiozaki H, Sugaya H (2005) Arthroscopic repair of a humeral avulsion of the glenohumeral ligament lesion. Arthroscopy 21(5):632
Kralinger F, Aigner F, Longato S, Rieger M, Wambacher M (2006) Is the bare spot a consistent landmark for shoulder arthroscopy? A study of 20 embalmed glenoids with 3-dimensional computed tomographic reconstruction. Arthroscopy 22(4):428–432
Lafosse L, Boyle S (2010) Arthroscopic Latarjet procedure. J Should Elb Surg 19(2 Suppl):2–12
Lazarus MD, Sidles JA, Harryman DT 2nd, Matsen FA 3rd (1996) Effect of a chondral-labral defect on glenoid concavity and glenohumeral stability. A cadaveric model. J Bone Jt Surg Am 78(1):94–102
Lecouvet FE, Simoni P, Koutaissoff S, Vande Berg BC, Malghem J, Dubuc JE (2008) Multidetector spiral CT arthrography of the shoulder. Clinical applications and limits, with MR arthrography and arthroscopic correlations. Eur J Radiol 68(1):120–136
Magarelli N, Milano G, Sergio P, Santagada DA, Fabbriciani C, Bonomo L (2009) Intra-observer and interobserver reliability of the ‘Pico’ computed tomography method for quantification of glenoid bone defect in anterior shoulder instability. Skeletal Radiol 38(11):1071–1075
Magee T (2009) 3-T MRI of the shoulder: is MR arthrography necessary? Am J Roentgenol 192(1):86–92
Melvin JS, Mackenzie JD, Nacke E, Sennett BJ, Wells L (2008) MRI of HAGL lesions: four arthroscopically confirmed cases of false-positive diagnosis. Am J Roentgenol 191(3):730–734
Millett PJ, Clavert P, Warner JJ (2005) Open operative treatment for anterior shoulder instability: when and why? J Bone Jt Surg Am 87(2):419–432
Nofsinger C, Browning B, Burkhart SS, Pedowitz RA (2011) Objective preoperative measurement of anterior glenoid bone loss: a pilot study of a computer-based method using unilateral 3-dimensional computed tomography. Arthroscopy 27(3):322–329
Oh JH, Kim JY, Choi JA, Kim WS (2010) Effectiveness of multidetector computed tomography arthrography for the diagnosis of shoulder pathology: comparison with magnetic resonance imaging with arthroscopic correlation. J Should Elb Surg 19(1):14–20
Owens BD, Duffey ML, Nelson BJ, DeBerardino TM, Taylor DC, Mountcastle SB (2007) The incidence and characteristics of shoulder instability at the United States Military Academy. Am J Sports Med 35(7):1168–1173
Owens BD, Harrast JJ, Hurwitz SR Thompson TL, Wolf JM (2011) Surgical trends in Bankart repair: an analysis of data from the American Board of Orthopaedic Surgery Certification Examination. Am J Sports Med 39(9):1865–1869
Rutten MJ, Jager GJ, Kiemeney LA (2010) Ultrasound detection of rotator cuff tears: observer agreement related to increasing experience. Am J Roentgenol 195(6):W440–446
Sanders TG, Morrison WB, Miller MD (2000) Imaging techniques for the evaluation of glenohumeral instability. Am J Sports Med 28(3):414–434
Scheibel M, Kraus N, Diederichs G, Haas NP (2008) Arthroscopic reconstruction of chronic anteroinferior glenoid defect using an autologous tricortical iliac crest bone grafting technique. Arch Orthop Trauma Surg 128(11):1295–1300
Shahabpour M, Kichouh M, Laridon E, Gielen JL, De Mey J (2008) The effectiveness of diagnostic imaging methods for the assessment of soft tissue and articular disorders of the shoulder and elbow. Eur J Radiol 65(2):194–200
Spang JT, Karas SG (2005) The HAGL lesion: an arthroscopic technique for repair of humeral avulsion of the glenohumeral ligaments. Arthroscopy 21(4):498–502
Steinbach LS (2008) MRI of shoulder instability. Eur J Radiol 68(1):57–71
Sugaya H, Moriishi J, Dohi M, Kon Y, Tsuchiya A (2003) Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Jt Surg Am 85–A(5):878–884
Sugaya H, Moriishi J, Kanisawa I, Tsuchiya A (2005) Arthroscopic osseous Bankart repair for chronic recurrent traumatic anterior glenohumeral instability. J Bone Jt Surg Am 87(8):1752–1760
Sugaya H, Moriishi J, Kanisawa I, Tsuchiya A (2006) Arthroscopic osseous Bankart repair for chronic recurrent traumatic anterior glenohumeral instability. Surgical technique. J Bone Jt Surg Am 88 Suppl 1 Pt 2:159–169
Tauber M, Resch H, Forstner R, Raffl M, Schauer J (2004) Reasons for failure after surgical repair of anterior shoulder instability. J Should Elb Surg 13(3):279–285
Yamamoto N, Itoi E, Abe H et al (2009) Effect of an anterior glenoid defect on anterior shoulder stability: a cadaveric study. Am J Sports Med 37(5):949–954
Yiannakopoulos CK, Mataragas E, Antonogiannakis E (2007) A comparison of the spectrum of intra-articular lesions in acute and chronic anterior shoulder instability. Arthroscopy 23(9):985–990
Young AA, Maia R, Berhouet J, Walch G Open Latarjet procedure for management of bone loss in anterior instability of the glenohumeral joint. J Should Elb Surg 20(2 Suppl):S61–69
Zappia M, Negri G, Grassi S, Pecoraro C, Rotondo A (2008) The CT-arthrography in the antero-inferior glenoid labral lesion: pictorial presentation and diagnostic value. Int J Should Surg 2(1):7–12
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moroder, P., Resch, H., Schnaitmann, S. et al. The importance of CT for the pre-operative surgical planning in recurrent anterior shoulder instability. Arch Orthop Trauma Surg 133, 219–226 (2013). https://doi.org/10.1007/s00402-012-1656-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-012-1656-7