Abstract
Background
Fractures of the proximal tibia occur very often and are a great challenge for trauma surgeons to stabilize. Although locked nails were developed to stabilize these fractures, this technique has not been sufficiently investigated. The purpose of this study was to biomechanically assess the stability of locked intramedullary nailing compared to locked plating.
Methods
16 fresh frozen human cadaveric tibiae were osteotomized in the meta-diaphyseal intersection with an osteotomy gap of 10 mm and a single osteotomy through the medial epicondyle to simulate a 41-C.2 fracture. Stabilization was performed with an angle stable locked Targon-TX nail (n = 8) and two additional canulated screws. The other testing group (n = 8) was treated with two canulated screws and a five-hole LCP-PLT. The bones were tested in a cyclic testing protocol with increasing loads under compression and a load sharing of 60 % through the medial tibial plateau and 40 % to the lateral side. Stiffness and fracture gap movement were measured and failure mode was assessed.
Results
No significant differences were found between the two implants regarding load until failure. The stiffness of the intramedullary nailing group (927 N/mm) was statistically significantly higher than the stiffness of the plating group (564 N/mm). No differences were found for fracture gap movement in the z-axis. However, differences were found for dislocation of the proximal-lateral and proximal-medial fragments, with absolute values of 0.099 mm in the plate group and 0.66 mm in the nailing group at 800 N. Prior to failure, fracture gap movement was 0.22 mm for the plating group and 1.66 mm for the nailing group, a difference that was also statistically significantly different. The nailing group failed by screw cut-out while the plating group failed by screw breakage.
Conclusion
Nailing of proximal tibia fractures leads to a stiffer implant-bone construct than plating. Since no adverse effects were found after nailing it seems to be a good alternative to plating for intra-articular proximal tibia fractures, especially in patients with soft tissue problems.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fractures of the proximal tibia account for 5–11 % of all tibia fractures and are often a result of high energy trauma [1–3]. Because of misalignment in the knee joint, caused by traction of the tendon of the proximal third of the tibia, proximal tibia fractures are difficult to treat [1, 3–6]. Since the introduction of locked plating and development of biological fixation focusing on minimally invasive insertion techniques and preservation of soft tissue, a noticeable decrease of non-unions and soft tissue associated complications has occurred [7, 8]. Plate osteosynthesis enables simpler reduction and retention of the fragments than intramedullary nailing and are therefore primary choice. The treatment of proximal extra-articular tibia fractures with intramedullary devices is difficult because of various tendon tractions around the knee joint and should be performed only by an experienced surgeon to avoid malalignment. Thus, poller screws are often necessary to counteract the displacement of the fracture and insertion points can vary [9, 10]. By newer nail designs, biomechanical studies have shown that intramedullary nail fixation leads to significantly better results of proximal tibia fractures than plating [11, 12]. The reduction and stabilization of proximal tibia fractures using nails can be difficult. For a better control of reduction and nail entry point, a preoperative CT scan is necessary and intraoperatively performed arthroscopy is helpful to achieve a correct replacement of the intra-articular fragments.
According to the AO principles, C-type fractures have to be converted to A-type fractures. This can be achieved by screw fixation of the intra-articular fracture parts to gain correct articular alignment before fixation of the extra-articular fracture parts.
To the authors’ knowledge, no studies regarding the treatment of intra-articular fractures of the tibia plateau with single screws and intramedullary nails are available. Therefore, this study was designed to determine if complex intra-articular fractures of the proximal tibia can be stabilized with angular stable locked nailing combined with single screws. Our hypothesis was that intramedullary nailing leads to a stiffer implant-bone construct and less interfragmentary movement than locked plate osteosynthesis in intra-articular proximal tibia fractures.
Materials and methods
For this biomechanical study, 16 fresh frozen human cadaveric tibiae were used. Seven male and nine female tibiae were used with a mean age of 73 years (range 45–91 years). CT scans (Lightspeed, GE, USA) of all bones were made to exclude bone diseases such as M. Paget, metastasis, or earlier fractures.
As intra-articular fracture model, a medial 41-C.2 fracture was chosen and realized with an oscillating saw (Fig. 1). To produce a reproducible fracture parallel to the ventral ridge, an osteotomy was made through the deepest point of the medial tibial condyle followed by lag screw fixation and implantation of a nail or a plate.
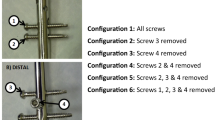
Two canulated screws (ASNIS III, Stryker, Mahwah, NJ, USA) were used for fracture stabilization of the intra-articular fracture part. The 5 mm canulated screws were inserted in a standardized fashion. The first screw was inserted 10 mm below and parallel to the tibial plateau at the height of the intercondylar eminentia. The second canulated screw was placed 10 mm anterior to the first screw and 10 mm below the joint plane. The length of the screws depended on the size of the bone. Then a locked nail (Targon TX, Aesculap, Tuttlingen, Germany) with angular stable locking screws and a locked plate (LCP-PLT-5-hole, Synthes, Paoli, PA, USA) were implanted according to the specific group design. All implants were applied according to the manufacturer’s standards. The nail was angular stable interlocked by three proximal screws and one screw directly under the meta-physeal gap and by one interlocking screw below the medullary isthmus in the distal tibia. Plate osteosynthesis was done with a five-hole LCP-PLT using five screws in the proximal fragment and four bicortical screws in the distal fragment. The distance of the screws next to the meta-physeal gap was the same for both treatment strategies.
Before biomechanical testing, an osteotomy gap of at least 10 mm was made 45 mm below the tibia plateau, according to a 41-A3 AO-classification fracture (Fig. 2).
Biomechanical testing was performed with a servohydraulic test machine (Instron 8874 Fa, Instron, Pfungstadt, Germany) under cyclic testing conditions. The tibiae were fixed distally in 15° flexion. The load was applied axially through the femoral component of a knee prothesis. Axial load sharing was set at 60 % on the medial plateau and 40 % on the lateral plateau side, similar to physiological loading conditions commonly known as the Miculicz line [13] (Fig. 3). Cyclic loading was performed starting with a load range from 50 to 150 N and the upper load level was increased with increments of 50 N until failure was reached. For each load, step 1,000 cycles were performed.
To measure fracture gap movement and fragment displacement an optoelectric measurement device with an accuracy of 0.1 mm was used (Pontos, Fa. GOM, Braunschweig, Germany). On each fragment at least four markers were placed next to the fracture gap. At the beginning and at the end of each load step pictures were taken to calculate the fragment displacement.
The characteristics of the different implants were analyzed by determining construct stiffness, fragment movement and displacement, and failure mode. Construct stiffness was calculated for stiffness at 800 N load, because all specimen passed this stage.
Statistics were performed by SPSS using a t test with Bonferroni adjustment. The level of significance was defined with a p value < 0.05.
Results
Load and cycles to failure
The median number of cycles to failure was 26,360 (range 18.472–38.193) for the plate group and 21.941 (range 14.447–36.944) for the nail group. The respective levels of load to failure were 1,350 N for the plate group and 1,200 N for the nail group. The differences were not statistically significant (p = 0.35) (Fig. 4).
Stiffness
For implant-bone constructs, a significantly higher stiffness at 800 N was found for the nail group (p = 0.046). The median stiffness values were 535 N/mm (range 352–831) for the plate group and 784 N/mm (range 495–1,800) for the nail group (Fig. 5).
Fragment displacement in z-axis
At 800 N and at failure load, no significant differences were recorded between the groups (p = 0.29) for displacement in the z-axis between the articular fragments and the diaphysis. For fracture gap movement at load to failure again no significant differences were found between the nailing and plating group (p = 0.12) except for displacement of the medial to lateral fragment (Table 1).
Clinical failure
Reasons for failure were screw breakage and loosening. Screw breakage occurred more often in the plate group than in the nailing group while slot holes were observed in the nail group (Table 2).
Discussion
The findings of our study suggest that stabilization of proximal tibial fractures (AO-C.2) can be achieved with comparable mechanical performance using either locked plating or angular stable nailing in combination with lag screw fixation, respectively. Load until failure and cycles until failure were similar for plating and nailing. Due to the central placement of the nailing, construct vertical displacements were lower after nailing compared to plating. In contrast relative proximal fragment displacement was reduced by plating due to the number of screws fixing the proximal fragments. Ultimate strength of plating and nailing appeared to be comparable. The load until failure was 1,350 N for the LCP-PLT and 1,200 N for the Targon-TX. An investigation of Jiang et al. [14] showed failure loads of about 2,500 N for the LISS-PT in artificial tibiae. These higher loads can be explained by the higher density of artificial bones. In the present protocol, the mean age of the specimen was 73 years. Therefore an osteoporosis has to be assumed which explains the lower loads until failure. Load until failure and bone mineral density are known as correlating factors [15, 16].
While ultimate strength of osteosynthesis construct determines load bearing capacity, construct stiffness determines the amount of interfragmentary movement, which is essential for the progress of successful fracture healing. Construct stiffness was significantly higher for nailing in comparison to plating. This can be explained by the central position of the nail and the resulting reduction of bending moment. The moment of inertia of the plate is rather small in comparison to the nail even while the load was applied in axial direction. Even higher differences regarding stiffness under axial load were found by Hansen et al. [4] under static testing conditions with 265 % higher stiffness values for the intramedullary nail compared to the LISS construct. But the direct comparison to the current literature [4, 11, 12, 17] is not possible because of different testing set ups, implants, and recorded values. Muller [11], for example, did not record stiffness values.
Regarding fracture gap movement along the bone axis during the elastic range at 800 N and at load to failure, no significant differences were noticed. These findings are contrary to the results of Mueller et al. [11]. He found significantly lower fragment movement along the z-axis for intramedullary devices. These findings can be addressed to the different loading scenarios. In our study, testing was performed under cyclic conditions and in 15° bending of the knee joint, which reflects the maximum stress at the proximal tibia during the gait cycle. Under this kind of positioning and load application, the nail is not placed in the center of applied load and therefore load is transduced through a bending moment. The role of the direction in which the load is applied is crucial. In findings of Laflamme et al. [18], testing was performed under bending and torsional conditions, without axial load. In these testings, lower displacement values were found for the plating group in comparison to the nailing groups. This might be an unrealistic scenario, while main forces during gait cycle are applied in axial direction [19] and not under torsional load.
Fracture gap movement of the medial and lateral proximal fragments was significantly increased for the nail in comparison to the plate at 800 N and at load to failure. An explanation might be the central position of the nail and the higher stiffness of the nail which is not able to allow a movement of the whole articular block to the medial side like the plate. The stored energy is now conferred to the junction of the proximal fragments which are held by one interlocking bolt and the two cannulated screws. The absolute values are rather small and appear at 1 mm for 800 N. At load to failure, 1 mm for the plate and 1.6 mm for the nail were detected, so no clinical relevance is expected. The movement of medial to distal fragment and lateral to distal fragment did not show any significant differences in the sample groups. The mean fragment deviation was lower than 3 mm medially and lower than 1 mm laterally. These differences are explained by the position of the implants and by distribution of the load with 60 % on the medial side.
Results of construct stiffness have shown significant differences between the groups, but fracture gap movement did not. This can be explained by the moment of inertia and the different positioning of the implants. The plate contains a broadness of about 5 mm and the nail a diameter of 10 mm. Because the plate is fixed on the lateral side and the load is applied to the medial side by 60 % the bending angle on the plate is times higher than for the nail which is positioned centrally. Therefore, the lever arms are different for plates and nails. At 800 N the constructs are loaded under elastic conditions. Therefore the plates move back to their initial position and no plastic deformation can be observed.
Implant failure was influenced by the bone stock quality but also by the design of the implant. Screw subsidence was observed more often in the nailing group, while screw breakage was noticed more often in the plating group. No failure was seen on site of the single screw fixation with the ASNIS III screws except one case of screw subsidence of the dorsally implanted screw in a specimen with bad bone stock quality. The implant failure can be explained by the position of the nail and the plate, as well as the position of the ASNIS III screws. Depending on the large lever-arms in plate osteosynthesis a maximum load is applied to the junction of screw heads and the plate. This is a reasonable explanation why screw breakage is often observed in this region. The relatively high occurrence of screw subsidence and screw breakage must be considered as a problem of biomechanical testing [20], because in clinical investigations these findings are very rare or not even described [7, 8, 21, 22]. An explanation for this effect is the load sharing process during bone healing, which reduces load from the interface between bone and implant.
Conclusion
Angular stable locking nails provide significantly higher implant-bone construct stiffness in proximal tibia fractures compared with locked plating. Evaluation of load to failure and fragment displacement in the intramedullary nailing group showed no adverse effects. Clinically, treating intra-articular proximal fractures with intramedullary nailing is challenging to the surgeon because muscle traction leads to a dislocation of the fragments and reduction requires sound anatomical knowledge. However, the smaller incisions that intramedullary nailing allows can be advantageous for the patient.
References
Cole JD (1998) Intramedullary fixation of proximal tibia fractures. Tech Orthop 13:27–37
Dendrinos GK, Kontos S, Katsenis D et al (1996) Treatment of high-energy tibial plateau fractures by the Ilizarov circular fixator. J Bone Joint Surg Br 78:710–717
Lang GJ, Cohen BE, Bosse MJ et al (1995) Proximal third tibia fractures. Should they be nailed? Clin Orthop Relat Res 315:64–74
Hansen M, Blum J, Mehler D et al (2002) Intramedullary osteosynthesis of metadiaphyseal proximal tibial fractures: an optimized implant geometry can help to solve the problem. Osteosynth Trauma Care 10:188–191
Buehler KC, Green J, Woll TS, Duwelius PJ (1997) A technique for intramedullary nailing of proximal third tibia fractures. J Orthop Trauma 11:218–223
Schandelmeier P, Krettek C, Rudolf J et al (1997) Superior results of tibial rodding versus external fixation in grade 3B fractures. Clin Orthop 342:164–172
Haidukewych G, Sems SA, Huebner D, Horwitz D, Levy B (2007) Results of polyaxial locked-plate fixation of periarticular fractures of the knee. J Bone Joint Surg Am 89(3):614–620
Nikolaou VS, Tan HB, Haidukewych G, Kanakaris N, Giannoudis PV (2011) Proximal tibial fractures: early experience using polyaxial locking-plate technology. Int Orthop 35(8):1215–1221
Lembcke O, Rüter A, Beck A (2001) The nail-insertion point in unreamed tibial nailing and its influence on the axial malalignement in proximal tibial fractures. Arch Orthop Trauma Surg 121:197–200
Konrad G, Südkamp N (2007) Proximale extraartikuläre Tibiafraktur. Chirurg 78(161):175
Mueller CA, Eingartner C, Schreitmueller E et al (2005) Primary stability of various forms of osteosynthesis in the treatment of the proximal tibia. J Bone Joint Surg Br 87:426–432
Hansen M, Mehler D, Hessmann MH et al (2007) Intramedullary stabilization of extraarticular proximal tibial fractures: a biomechanical comparison of intramedullary and extramedullary implants including a new proximal tibia nail (PTN). J Orthop Trauma 21:701–709
Morrison JB (1970) The mechanics of the knee joint in relation to normal walking. J Biomech 3:51–61
Jiang R, Luo CF, Zeng BF (2008) Biomechanical evaluation of different fixation methods for fracture dislocation involving the proximal tibia. Clin Biomech 23:1059–1064
Brown SJ, Pollintine P, Powell DE, Davie MW, Sharp CA (2002) Regional differences in mechanical and material properties of femoral head cancellous bone in health and osteoarthritis. Calcif Tissue Int 71:227–234
Sommers MB, Fitzpatrick DC, Madey SM, Vande Zanderschlup C, Bottlang M (2007) A surrogate long-bone model with osteoporotic material properties for biomechanical testing of fracture implants. J Biomech 40:3297–3304
Hansen M, Blum J, Mehler D, Hessmann MH, Rommens PM (2009) Double or triple interlocking when nailing proximal tibial fractures? A biomechanical investigation. Arch Orthop Trauma Surg 129:1715–1719
Laflamme GY, Heimlich D, Stephen D, Kreder HJ, Whyne CM (2003) Proximal fracture stability with intramedullary nail fixation using oblique interlocking screws. J Orthop Trauma 17(7):496–502
D’Lima DD, Patil S, Steklov N, Slamin JE, Colwell CW (2006) Tibial forces measured in vivo after total knee arthroplasty. J Arthroplasty 21(2):255–262
Gollwitzer H, Karampour K, Hauschild M, Diehl P, Busch R, Mittelmeier W (2004) Biomechanical investigation of the primary stability of intramedullary compression nails in the proximal tibia: experimental study using interlocking screws in cryopreserved human tibias. J Orthop Sci 9(1):22–28
Lindvall E, Sanders R, Dipasquale T, Herscovici D, Haidukewych G, Sagi C (2009) Intramedullary nailing versus percutaneous locked plating of extra-articular proximal tibial fractures: comparison of 56 cases. J Orthop Trauma 23(7):485–492
Hansen M, El Attal R, Blum J, Blauth M, Rommens PM (2009) Intramedullary nailing of the tibia with the expert tibia nail. Oper Orthop Traumatol 21(6):620–635
Acknowledgments
This study was sponsored by Aesculap. No influence on the results was taken by the industrial partners. We would like to thank Kevin Burfeind for his translational work as an American native speaker.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Högel, F., Hoffmann, S., Panzer, S. et al. Biomechanical comparison of intramedullar versus extramedullar stabilization of intra-articular tibial plateau fractures. Arch Orthop Trauma Surg 133, 59–64 (2013). https://doi.org/10.1007/s00402-012-1629-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-012-1629-x