Abstract
Introduction
It is not known how the described methods of reduction and dynamic hip screw (DHS) fixation of displaced intracapsular femoral neck fractures translate into proper assessment of the postoperative radiographs. At teaching or evaluation sessions in daily practice, frequent discussion arises about postoperative technical assessment. The assessment of correct reduction and DHS fixation using the described methods in the literature may be subject to differences between observers. The aim of this study was to assess the extent of inter- and intraobserver agreement on technique, based on the methods in the literature, in a simulated daily practice setting.
Materials and methods
The postoperative anteroposterior (AP) and lateral radiographs of 35 randomly selected patients aged 60–90 years were rated twice, 2 months apart, by six surgical observers from three institutions with similar views on reduction and DHS fixation for this fracture type. The radiographs were of sufficient quality for proper assessment. Criteria for reduction and fixation could be rated as either adequate or inadequate. An adequate rating was assigned if in the observer’s opinion, regardless of likely outcome, technical perfection according to the described methods had been achieved. The kappa statistic was calculated as a measure of agreement.
Results
Fracture reduction on the AP view approached a good kappa value (0.54). Poor to moderate interobserver agreement was found for fracture reduction on the lateral view and aspects of DHS fixation (kappa 0.10–0.36). Intraobserver agreement was good for five out of six observers for reduction and DHS fixation aspects (kappa 0.51–0.81).
Conclusion
During routine practice six surgical observers can nearly agree on adequate fracture reduction on the AP view, but do not agree on adequate reduction on the lateral view and adequate DHS fixation on the postoperative radiographs of displaced intracapsular femoral neck fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
When the choice is made to treat a displaced femoral neck fracture with internal fixation, there are two essential technical prerequisites to fracture healing: adequate reduction and adequate internal fixation [10, 15, 17, 19]. In closed reduction and fixation, both of these aspects are determined by the surgeon intraoperatively using image intensification.
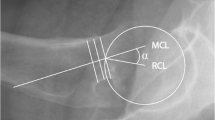
Before internal fixation, adequate reduction of displaced fractures of the femoral neck must take place. Inadequate reduction is a major risk factor for avascular necrosis and unstable fixation [10, 11]. After proper reduction, the Garden Index on the intraoperative image-intensified anteroposterior (AP) view should be between 160 and 180 deg [10], which corresponds to a CCD (caput-collum-diaphysis) angle between 130 and 150 deg. Valgus reduction of the femoral head on the AP view is acceptable up to 20 deg. Any degree of varus reduction of the femoral head on the AP view is unacceptable [6, 17]. On the lateral view, the alignment of the femoral head to the shaft should be as close as possible to 180 deg, with 10 deg retroversion being acceptable [4, 9, 17].
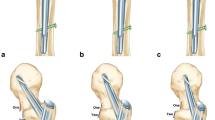
The dynamic hip screw (DHS, Mathys Medical, Bettlach, Switzerland) is one of many possible implants when performing internal fixation for displaced femoral neck fractures. In our hospital, the fixed-angle DHS is preferred if the fracture line is steeper than 50 deg (Pauwels 3 type fracture), measured intraoperatively with fluoroscopy. Correct insertion of the screw of the DHS for fractures of the femoral neck relies on the three-point fixation method described for cannulated screws: the screw should be inserted over the inferior calcar and in the lower half of the reduced femoral head. Following plate attachment, the first point of fixation is the inherent fixed angle of the DHS, the second point is the inferior calcar of the collum femoris, and the third point lies within the femoral head [2, 4, 5, 13, 17]. On the lateral view, the screw should be positioned in the center, or slightly in the dorsal part, of the femoral head and through the central part of the femoral neck [4].
Reduction and fixation aspects of displaced femoral neck fractures on postoperative radiographs are a frequent source of discussion amongst surgeons and their residents during teaching or evaluation sessions in routine clinical practice. Although the described methods of correct reduction and DHS fixation of displaced femoral neck fractures are clearly described in the literature, they may be subject to differences in observer agreement. The extent of this possible difference in observer agreement has not been reported, and it would be useful to know this during teaching sessions in daily practice.
The main aim of this study was to assess the intra- and interobserver agreement in routine clinical practice on reduction and DHS fixation aspects of displaced intracapsular femoral neck fractures.
Patients and methods
We randomly selected 35 patients between 60 and 90 years of age with displaced intracapsular fractures of the femoral neck who were being analysed in a larger multicenter study in the Netherlands. Patients were treated in three institutions (MST, AMC and SLH) with experience in DHS and cannulated screw fixation of displaced femoral neck fractures. The fractures selected for this study were reduced in a closed way and internally fixated with a DHS.
The observers’ group consisted of a staff general surgeon with trauma/orthopaedic surgery as a subspecialty and an orthopaedic resident from the same institution and four staff orthopaedic surgeons from two other institutions. All the surgical observers had experience with sliding hip screw placement for displaced fractures of the femoral neck and uniformly understood the described methods in the literature.
To omit the confounding factor of personal preference, it was checked that all observers preferred femoral head reduction in 0–20 deg of valgus on the AP view and preferred the head-shaft alignment to be close to 180 deg on the lateral view [4, 9, 10, 17]. All observers had incorporated the following DHS insertion method into their practice: placement of the screw over the inferior calcar and into the lower part of the femoral head on the AP view, and placement in the central or dorsal half of the femoral head on the lateral view [4, 17].
To simulate routine clinical practice, detailed instructions for reduction and fixation using exact measurements between predetermined reference points were omitted on purpose, as these measurements are not performed routinely.
Each observer received a list of criteria, as shown in the first column of Table 1. Any unclear issues about the list of criteria were resolved before the rating sessions started. The observers were only shown the postoperative radiographs, which were taken on the first postoperative day before weight-bearing.
Rating sessions
The quality of the AP and lateral postoperative hip radiographs was representative of those available in daily hospital routine. All 35 pairs of radiographs were judged to be clear enough for rating by all observers. Each observer then proceeded to rate reduction and fixation criteria as either adequate or inadequate on the separate views. At the end of the criteria list, the overall opinion of fracture reduction and DHS fixation on both views was rated. A rating of adequate was assigned if in the observer’s opinion the technical perfection according to described methods in the literature had been achieved for a particular criterion, regardless of the likelihood of clinical success or failure.
Each observer independently reviewed the radiographs of all 35 patients, with the identification labels covered and numbered in random order, once in the first session. As much time as needed for accurate assessment was provided. No feedback was given after this first session, and observers from the same clinic were blinded to each other’s findings.
For intraobserver variance the radiographs were reorganized, and each observer performed the same rating session again 2 months later.
Statistical analysis
Statistical analysis was done by calculating the kappa values using SPSS statistical software for intraobserver agreement [1]. For interobserver agreement a multiple rater formula for calculating the kappa value between more than two observers as described by Fleiss was used [8]. The result of this formula correlates with the average kappa value of each possible observer combination.
The kappa value was interpreted by Altman to represent the ‘chance corrected proportional agreement’ and can vary from -1 (complete disagreement) through 0 (agreement no better than chance) to +1 (complete agreement) [1]. No guidelines exist as to which level of agreement is acceptable. Altman after Landis and Koch recommends a kappa value of above 0.60 as good and above 0.80 as very good [1, 12]. The kappa value is sensitive to an extreme distribution of the two-by-two table, as the calculation produces a lower than expected kappa value. If the distribution is extreme, Altman recommends showing the two-by-two table for better interpretation [1]. No clear guidelines could be found regarding minimum number of ratings for proper kappa calculation. In this study, 70 ratings per criterion were performed between each possible pair of six observers. This number of ratings is sufficient for kappa calculation, given that no extreme distributions in the two-by-two tables were found [1].
Results
Each observer completed the criteria lists of all 35 AP and lateral radiographs fully without disturbance and blinded to the rating sessions of other observers. This was performed once in the first and once in the second rating sessions.
Intraobserver agreement
The intraobserver kappa values of the six observers for fracture reduction and DHS fixation methods are shown in Table 1.
The average intraobserver kappa values shown in the middle column of Table 2 vary from 0.48 to 0.77, indicating moderate to good intraobserver agreement according to Altman. Observer number 3 was noted to have disproportionally low kappa values for nearly all criteria. Average intraobserver kappa values were recalculated omitting the ratings of this observer. This is shown in the last column of Table 2, in which the average intraobserver kappa values improved for all criteria.
Interobserver agreement
In Table 3, kappa values for all criteria of fracture reduction and DHS fixation on separate and both AP and lateral views were below 0.60. This indicated poor to moderate interobserver agreement according to Altman. When omitting the rating of observer number 3, who had disproportionally low intraobserver agreement, the kappa values improved, but not above 0.60, for fracture reduction and DHS fixation on both AP and lateral views (Table 3, last column). Only fracture reduction on the AP view approached a good kappa value (0.54±0.09).
Figures 1 and 2 show characteristics of radiographs in which good interobserver agreement was found, and Figures 3 and 4 show characteristics of radiographs for which poor interobserver agreement was found.
Discussion
During closed reduction and DHS fixation of displaced femoral neck fractures, the surgeon interprets the described methods in the literature subjectively using image intensification. No exact measurements are routinely performed. The objective result is the postoperative radiograph. A radiologist was not included in the observers’ group as decision-making about the correct application of reduction and fixation methods is performed intraoperatively by surgeons.
To increase stability and reduce the risk of avascular necrosis, the principle of femoral head reduction in valgus on the AP view has been known for well over 30 years [4, 6, 9, 10, 11, 14, 17, 18]. Compared to the other criteria of reduction and fixation, a relatively high kappa value of 0.54 was found for this particular criterion. In Bjorgul and Reikeras’s study of interobserver agreement of radiographic signs predicting healing disturbance, a similar kappa value of 0.53 was found for the varus/valgus aspect of reduction [3]. The latter study also showed that comminution of the calcar and small size of the femoral head, suggested to be predictive factors of healing failure, had low interobserver agreement [3].
On the lateral view, the near 180-deg alignment of the head to the femoral shaft is an accepted reduction principle [4]. However, the available trauma and radiology literature is deficient in defining correct implant positioning in the femoral head with this view. This may clarify the poor interobserver agreement in this study.
Biomechanically, sliding hip screws maintained a significantly high peak force during cyclic loading compared with cannulated screws [7]. This supports fixing steep, Pauwels 3 type fractures with a fixed-angle implant, such as the DHS. However, randomized studies with a higher level of evidence have shown no advantage of one single internal fixation implant for displaced femoral neck fractures. Meta-analysis data show that sliding hip screws, pins and cannulated screws all performed similarly when considering the clinical outcome [16].
Low interobserver kappa values were found for the criteria concerning DHS fixation [2, 4, 5, 13, 17]. No specific studies concerning correct positioning of implants over the inferior calcar were found. For positioning of the screw within the femoral head in peritrochanteric fractures, Baumgaertner advocated a distance of the screw tip to the femoral head apex (tip-apex distance, TAD) of 25 mm or less [2].The femoral apex was defined as the point of intersection between the subchondral bone and a line in the center of and parallel to the femoral neck. Baumgaertner et al. stated that instructed observers familiar with the TAD measurement formula could reproduce the measurement correctly [2].In our study design simulating routine clinical practice, we found only moderate agreement (0.28–0.38) of screw positioning within the femoral head and TAD on the AP view. This demonstrates that the TAD cannot be reproduced without specific instruction.
On the lateral view, interobserver agreement was poor for screw position within the femoral head (0.19). This also reflects the paucity of literature describing optimal implant positioning with this view.
The intraobserver agreement for nearly all aspects of fracture reduction and fixation and overall technical opinion ranged from moderate to very good. The finding of good intraobserver agreement is important, as it indicates that the rating of reduction and fixation technique is consistently reproducible by the same person in daily practice. Only observer number 3, a staff orthopaedic surgeon, was less consistent, and we deemed it necessary to recalculate the average intra- and interobserver kappa values by omitting this observer’s ratings.
In conclusion, it seems that surgeons with similar views on how to correctly reduce and internally fixate a displaced femoral neck fracture with a DHS can nearly agree on what should be considered a good reduction on the AP view, but cannot agree on what should be considered a good reduction on the lateral view and a good DHS fixation in routine clinical practice. Each individual surgeon was rather consistent in his own opinion. This finding is interesting for the discussion of this subject at teaching or evaluation sessions. Based on Garden’s original study [10] and a reasonable interobserver agreement, we strongly recommend that proper reduction of the femoral head on the AP view should be in 5-20 deg of valgus, corresponding to a Garden index of 165-180 deg.
Given the differences in femoral neck fracture patterns, it could well be impossible to establish a classification system for reduction and fixation techniques on which surgeons completely agree. In the long term, we are working towards comparable clinical protocols and broadly accepted clinical practice guidelines based on high-level evidence, which will help generate more agreement in routine clinical practice on the correct treatment of this increasingly common fracture type. When good agreement is achieved, a technical assessment will have clinical consequences.
References
Altman DG (1999) Practical statistics for medical research. Chapman and Hall, London
Baumgaertner MR, Curtin SL, Lindskog DM et al (1995) The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am 77:1058–1064
Bjorgul K, Reikeras O (2002) Low interobserver reliability of radiographic signs predicting healing disturbance in displaced intracapsular hip fracture of the femoral neck. Acta Orthop Scand 73:307–310
Bosch U, Schreiber T, Krettek C (2002) Reduction and fixation of intracapsular fractures of the proximal femur. Clin Orthop 399:59–71
Bout CA, Cannegieter DM, Juttman JW (1997) Percutaneous cannulated screw fixation of femoral neck fractures: the three point principle. Injury 28:135–139
Chua D, Jaglal SB, Schatzker J (1998) Predictors of early failure of fixation in the treatment of displaced subcapital hip fractures. J Orthop Trauma 12:230–234
Deneka DA, Simonian PT, Stankewich CJ et al (1997) Biomechanical comparison of internal fixation techniques for the treatment of unstable basocervical femoral neck fractures. J Orthop Trauma 11:337–343
Fleiss JL (2000) Statistical methods for rates and proportions. John Wiley, New York, pp 212–36
Garden RS (1961) Low-angle fixation in fractures of the femoral neck. J Bone Joint Surg Br 48:647–663
Garden RS (1971) Malreduction and avascular necrosis in subcapital fractures of the femur. J Bone Joint Surg Br 53:183–197
Gomez-Castresana F, Caballer AP, Portal LF (2002) Avascular necrosis of the femoral head after femoral neck fracture. Clin Orthop 399:87–109
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Luitse JSK, Dunki Jacobs PB, Hart CP van der (1993) The Dynamic Hip Screw; golden standard in the treatment of pertrochanteric fractures? In: Marti RK, Dunki Jacobs PB (eds) Proximal femoral fractures. Medical Press, London, pp 409–22
McElvenny RT (1945) Roentgenographic interpretation of what constitutes adequate reduction of femoral neck fractures. Surg Gyn Obst 80:97–106
Parker MJ (1994) Prediction of fracture union after internal fixation of intracapsular femoral neck fractures. Injury 25:3–6
Parker MJ, Blundell C (1998) Choice of implant for internal fixation of femoral neck fractures. Acta Orthop Scand 69:138–143
Parker MJ (2000) The management of intracapsular fractures of the proximal femur. J Bone Joint Surg Br 82:937–941
Pauwels F (1935) Der schenkelhalsbruch. Ein mechanisches problem. Supplement to Z Orthop Chir 63. Enke Stuttgart
Swiontkowski MF (1994) Current concepts review: intracapsular fractures of the hip. J Bone Joint Surg Am 76:129–138
Acknowledgements
We wish to thank our observers and reviewers: William Ertl, MD, Ian Harris, FRACS (Orth), Sean E. Nork, MD, R.P. Poolman, MD, and Professor DJ Gouma, PhD.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Heetveld, M.J., Raaymakers, E.L.F.B., van Walsum, A.D.P. et al. Observer assessment of femoral neck radiographs after reduction and dynamic hip screw fixation. Arch Orthop Trauma Surg 125, 160–165 (2005). https://doi.org/10.1007/s00402-004-0780-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-004-0780-4