Abstract
Introduction
In the 1970s and 1980s, uncemented, threaded acetabular components with smooth surface treatment were widely used in continental Europe for arthroplasty of the hip to overcome the high rate of aseptic loosening in cemented hip arthroplasty in young patients. There were several reports on short- and intermediate-term results, but information on survival in the longer term is not available at present.
Materials and methods
In a consecutive series of 320 patients, 348 threaded cups with smooth surface treatment (221 Mecring and 127 Weill) had been implanted in combination with one type of uncemented stem. Patients were followed clinically and radiographically. The mean time of follow-up was 12.4 (range 10–15) years (Mecring 11.9 years, Weill 13.3 years).
Results
In 76 hips the acetabular component had been revised (Mecring 56, Weill 20): 7 hips for infection and 69 for aseptic loosening. Of the remainder, the cup had migrated in 55 hips, and 32 hips were awaiting revision. Survival at 14 years was 63.8% (95%CI: 52.5–75.0%) for the Mecring and 76.2% (95%CI: 65.6–86.7%) for the Weill component. Radiolucent lines were present in 59 hips (31.9%). The median Harris Hip Score at follow-up was 84 points (Mecring 85, Weill 82). Radiographic loosening did not correlate with clinical outcome.
Conclusion
These results support the view that smooth, threaded acetabular components do not provide satisfactory long-term fixation and should be abandoned.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several methods of uncemented acetabular fixation are available for total hip arthroplasty (THA). Stable primary fixation can be achieved with threaded or hemispherical press-fit components with or without additional screws [32]. Most cups now have a grit-blasted surface treatment, porous coating or optional HA coatings for enhanced bone ingrowth.
In the late 1970s various designs of threaded, uncemented cups were introduced, achieving initial stability by interference of the threads with acetabular bone. Threaded components have been advocated because of their high primary stability which is a prerequisite factor for bone ongrowth and long-term fixation [15, 23, 25]. Different design criteria, i.e. spherical or conical shape, have been the subject of debate [15, 32]. The surface treatments of these implants were smooth in most cases. Threaded designs lead to rigid primary fixation, but long-term secondary fixation without bone ingrowth is unlikely to occur,and consequently high rates of mid-term loosening and failure were reported [7, 17, 37]. Even though this type of fixation was very popular in the 1980s, only short- to mid-term results have actually been published in the literature. Few long-term results of threaded cups have been reported in the literature, with a great variability in survival (Table 1) [10, 19, 24, 26, 39]. The surface treatment seems to have a major effect on the incidence of radiographic loosening and survival in the longer term [11]. Although inferior results have already been reported for Mecron and Weill acetabular components with a high rate of catastrophic failures at 5–7 years [17, 37], it is important to follow these patients regularly in the long term, as a high rate of painless migration has been reported [2, 3]. The aim of our study was to determine the long term (>10 years) outcome in this group with smooth, threaded cups. Therefore, we evaluated the clinical and radiographic outcome of a consecutive multisurgeon series of our first 320 consecutive patients treated with smooth acetabular components.
Patients and methods
Two different designs of uncemented, threaded, screw-in components with smooth surface treatment were investigated. Both components have a central opening, which enables visualization of the fit.
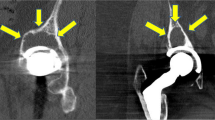
In 221 hips a Mecring A (Mecron Medizinische Produkte, Berlin, Germany) cup made of titanium alloy (Ti6Al14V) was used (Fig. 1). It consists of a matte, spherical, threaded, titanium shell and a polyethylene (PE) liner without metal backing. After hemispherical reaming, the metal shell is screwed into the acetabulum.
Weill cups (Protek AG, Berne, Switzerland) made of pure titanium were implanted in 127 hips (Fig. 1). This implant consists of a smooth, threaded, conical ring and a PE liner. For acetabular reaming a conical reamer is used, and the threads are precut by a thread-cutting device.
In both components the posterior opening is closed by the PE liner. In all cases 32 mm ceramic heads (Biolox, Ceramtec) were used. The acetabular component was implanted in combination with one type of uncemented, straight, collarless component in all patients. It was made from Ti6Al7Nb alloy (Protasul 64) with a microporous surface treatment (Ra=4.4 µm) according to ISO 5832-11 (CLS, Sulzer Orthopedics). It had a wedge-shaped taper in all three planes with proximal, anterior and posterior located ribs/flutes.
This study comprised a consecutive series of 320 patients with 348 hips implanted between January 1985 and December 1989. During the follow-up period, 52 patients with 55 hips died, and 8 patients (8 hips) could not be located (Figs. 2, 3). Follow-up data were obtained for 209 hips; of which 141 hips were collected by the first author. The remainder was seen by their local orthopaedic surgeon. Standard radiographs were taken and sent to our institution for evaluation (44 hips). A standardized questionnaire including the items of the Harris Hip Score was used and evaluated. Clinical data but no radiographs could be obtained for 24 hips. The 10–15 year follow-up rate was 82% for the entire patient group and 96% for the patients still alive at the time of the follow-up evaluation. The operations were performed by 23 different surgeons in one institution. Patient demographics and diagnoses are listed in Table 2.
Either a modified Watson-Jones or a transgluteal lateral Bauer approach with the patient in supine position was used. The acetabular bone was reamed and an attempt made to preserve the subchondral bone in the acetabular roof. Preparation of the acetabulum for Mecring components was performed using a hemispherical powered reamer increasing in size. The cups were screwed into the acetabulum until adequate interlock was achieved by self-tapping. The threads were not precut. For the Weill components, a conical powered reamer was used, and the threads were precut using a hand-driven thread-cutting device. Postoperative partial weight-bearing was encouraged for 6 weeks in all patients. The use of crutches was encouraged for 3 months. No regular prophylaxis (irradiation or non-steroidal anti-inflammatory drugs) for the prevention of heterotopic ossification was given at this time.
At follow-up, a standardized questionnaire including the items of the Harris Hip Score was given to each patient/hip [20]. The clinical assessment included limp, range of motion and pain. Patients assessed their pain in the operated hip at the time of follow-up on a visual analogue scale (range 0–10). For pain calculations the pain score according to Harris was used. The radiographs were examined by two independent experienced orthopaedic surgeons for cup migration, radiolucent lines, osteolysis and acetabular loosening.
Acetabular loosening was defined as continuous migration >5 mm or tilting >5° compared with baseline radiographs or bone resorption (>5 mm). The threshold loosening of the acetabular component was chosen to be 5 mm because of the inaccuracy of simple measurements on plain radiographs. Radiolucent lines were determined according to DeLee and Charnley [12]. Osteolysis was determined as regional, progressive bone changes on serial radiographs.
Statistical analysis
Kaplan-Meier survival analyses were calculated using revision for aseptic loosening, revision of the cup for any cause, and all revisions plus patients awaiting revision as endpoint to plot the cumulative survival rate [33].
Results
In 264 hips (78%), the acetabular prosthesis had not been revised. In 76 hips (22%), the cup had been revised. Seven hips were revised because of a deep infection (2%; 2 acute, 5 late) (Figs. 2, 3). A total of 69 acetabular implants (20%) were revised for aseptic loosening.
The median Harris Hip Scores, Harris Pain Scores, pain levels on a visual analogue scale, and Charnley class are shown in Table 3. No correlation between radiographic loosening and pain was found. Most patients with acetabular migration had only mild or moderate pain. No leg length discrepancies were found in 71% of patients. In 18% a leg length difference of 0.5–1.5 cm was found; in 5% a difference of 1.5–2.5 cm; and in 6% a difference of >2.5 cm was measured.
Survival estimate
The Kaplan-Meier analyses showed an increasing annual failure rate over time for both components, with an increase in revision after 8 years (Fig. 4, 5, 6). In years 10 to 15, survival was significantly inferior for the Mecring cup. The survival rate was 63.8% (95% confidence limits: 52.5–75.0%) for the Mecring and 76.2% (95%CI: 65.6–86.7%) for the Weill components at 14 years. Survival with acetabular revision for aseptic loosening as an endpoint was 65.4% (95%CI: 53.9–76.8%) and 77.5% (95%CI: 66.9–88.0%) for Mecring and Weill cups, respectively, at 14 years. The worst-case scenario including hips awaiting revision was 19.8% (95%CI: 0–48.0%) for Mecring and 48.1% (95%CI: 27.2–69.0%) for Weill components at 14 years.
The Kaplan-Meier analysis of the stem showed a low annual failure rate and a survival rate of 91.7% for femoral components after 13 years (95%CI: 88.4%–95.0%) without revision (for any reason). Survival with femoral revision for aseptic loosening as an endpoint was 94.9% (95%CI: 92.1%–97.7%) after 13 years, with no more revisions until year 15. The survival rate remained unchanged until year 15 as no more revisions occurred in this period [2, 4].
A total of 52 patients (55 hips) had died before the most recent follow-up less than 10 years postoperatively. The mean age of these patients at the time of the operation was 62.1 years (range 41–81 years), and the mean duration of follow-up was 7.7 years (range 0–14 years). Fifty patients were followed for a minimum of 1 year.
Radiographic findings
Acetabular component: 22% of acetabular cups [56 Mecring (25%), 20 Weill (16%)] had been revised prior to the most recent follow-up. Of the 209 unrevised hips available for follow-up, 32 cups (15%) had migrated and are awaiting revision (23 Mecring and 9 Weill). Radiolucent lines (>2 mm) were found in zones 1–3 according to Charnley and DeLee in 59 hips (32%) (Table 4).
Femoral component: Radiographic loosening with a continuous radiolucent line was found in one stem without clinical symptoms. Distal cortical hypertrophy or femoral osteolysis was not observed in any case. Stress shielding (2–4 deg) with atrophy of the proximal femoral region was not detected [2, 3, 4].
Discussion
Aseptic loosening after THA over time remains a problem, especially in young patients [18]. Some uncemented acetabular components rely on biological fixation and have achieved lower rates of aseptic loosening at 10 years compared with cemented acetabular components in younger patients (Table 1) [6, 9, 38]. However, revision rates for uncemented cups are higher because of accelerated PE wear and osteolysis [21, 38].
In the past, two main factors affecting the long-term survival of uncemented implants were identified: (1) primary stability with stable bone-implant interlock and minimal micromotion and (2) secondary osseointegration for long-term stability. An adequate surface finish, most commonly by porous coating, hydroxyapatite or grit-blasted titanium, is considered important for bone ongrowth or ingrowth [32]. As the human acetabulum is hemispherical in shape, most acetabular components are hemispherical for preservation of bone stock providing initial stability by the insertion of screws, press-fit, threads or pegs. However, conical implants providing initial fixation using a threaded design have been promoted in the past because of their rigid initial fixation and resistance to tilting forces. Just recently, long-term studies of uncemented, threaded, conical (grit-blasted) components have been published, proving a long-term survival equal to the rates of hemispherical press-fit cups (Table 1) [1, 10, 19, 39].
As contemporary implants provide a 10-year survival rate of well over 90%, it is difficult to prove a superior design as numbers would exceed the scope of most clinical studies [33], and differences may only be discerned in national registers with larger numbers [22]. In contrast, the long-term results of smooth acetabular components have been reported to be inferior, with high rates of loosening and failure (Table 1) [26, 27]. In our study only threaded acetabular components with a smooth surface treatment were used. The survival was considerably lower compared with contemporary designs with rough surface treatment [10, 19, 39]. We discontinued the use of smooth, threaded components in 1993.
The most likely cause of the high failure rates was insufficient biologic fixation due to the smooth surface treatment and a lack of osseointegration [11, 35]. Because revision rates were high for both study groups, we found a significant difference in the survival of the two implants. However, there were no differences with regard to femoral head diameter and material, patient age, gender, diagnosis and postoperative treatment. Thus, the differences in survival can be attributed mainly to the implant design. The most striking difference is the outer geometry of the two implants involved in this study. The conical design of the Weill components seems to provide better long-term stability, even if no regular bone ingrowth occurs [11]. Increased primary stability of conical threaded cups compared with spherical cups has been found in experimental in vitro studies [32]. Our results suggest that the tapered shape seems to enhance the long-term stability, and the survival rates correspond well to the results reported for other conical threaded components at >10 years (Table 4) [26, 27]. The shape and the distance between threads might also have influenced survival [15]. Another difference is the shape of the PE insert inside the metal shell, which might have an effect on PE wear. Theoretically, under physiological loading the PE liner can be pressed into the posterior opening of the metal shell, thus creating a locking effect of the prosthetic head, which may then lead to increased rotational forces and consecutive loosening. Certainly, more attention should be paid to the possibility of backside wear caused by direct PE (of the non-metal-backed insert) to bone contact, and it was indeed regularly documented at revision. Unfortunately, we did not have the facilities to measure particulate wear in this study, as commonly used wear programs did not support the analysis of these types of metal shells [13, 30].
Surprisingly, only a weak correlation between aseptic loosening, migration and pain was found. A considerable number of patients even with severe bone loss complained of only slight pain and noticed leg length discrepancy. This scenario is particularly worrisome, and therefore with this type of acetabular component, regular radiographic follow-up seems advisable to detect painless migration before severe bone loss can occur, necessitating more demanding revision surgery.
To date, there are only a few published long-term results for smooth, hemispherical, threaded cups. Even though the short-term results have been promising [28], mid-term results have shown high rates of failure [7, 8, 17, 37]. Our results show that in the 7th postoperative year, revision rates rise, and maintaining annual radiographic follow-up is vital to prevent bone loss due to osteolysis and migration as seen in Fig. 7. This finding is comparable to the phenomenon reported by Morscher and Schmassmann [31]. We conclude that smooth, threaded sockets do not provide a satisfactory long-term outcome and should be abandoned.
References
Aigner C (1998) 10 year results with the corund-blasted Zweymuller titanium alloy threaded acetabular cup (in German). Z Orthop 136:110–114
Aldinger PR, Breusch SJ, Lukoschek M, Mau H, Ewerbeck V, Thomsen M (2003) A ten- to 15-year follow-up of the cementless spotorno stem. J Bone Joint Surg Br 85:209–214
Aldinger PR, Sabo D, Pritsch M, Thomsen M, Mau H, Ewerbeck V, Breusch SJ (2003) Pattern of periprosthetic bone remodeling around stable uncemented tapered hip stems: a prospective 84-month follow-up study and a median 156-month cross-sectional study with DXA. Calcif Tissue Int 73:115–121
Aldinger PR, Thomsen M, Mau H, Ewerbeck V, Breusch SJ (2003) Cementless Spotorno tapered titanium stems: excellent 10–15-year survival in 141 young patients. Acta Orthop Scand 74:253–258
Bertram R, Muller RT (1998) Intermediate-term results with the Mecron screw cup acetabulum—a follow-up study (in German). Z Orthop 136:317–320
Bohm P, Bosche R (1998) Survival analysis of the Harris-Galante I acetabular cup. J Bone Joint Surg Br 80:396–403
Bruijn JD, Seelen JL, Feenstra RM, Hansen BE, Bernoski FP (1995) Failure of the Mecring screw-ring acetabular component in total hip arthroplasty. A three to seven-year follow-up study. J Bone Joint Surg Am 77:760–766
Capello WN, Colyer RA, Kernek CB, Carnahan JV, Hess JJ (1993) Failure of the Mecron screw-in ring. J Bone Joint Surg Br 75:835–836
Crowther JD, Lachiewicz PF (2002) Survival and polyethylene wear of porous-coated acetabular components in patients less than fifty years old: results at nine to fourteen years. J Bone Joint Surg Am 84:729–735
Delaunay C, Kapandji AI (2001) Survival analysis of cementless grit-blasted titanium total hip arthroplasties. J Bone Joint Surg Br 83:408–413
Delaunay CP, Kapandji AI (1997) Acetabular screw rings and surface treatment. Clin Orthop 340:130–141
DeLee JG, Charnley J (1976) Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop 121:20–32
Devane PA, Robinson EJ, Bourne RB, Rorabeck CH, Nayak NN, Horne JG (1997) Measurement of polyethylene wear in acetabular components inserted with and without cement. A randomized trial. J Bone Joint Surg Am 79:682–689
Effenberger H, Weber M, Dorn U, Hofer H (1997) Roentgen criteria and radiologic results of the Hofer-Imhof (H-I) threaded acetabulum cup in first time implantation (in German). Z Orthop 135:434–443
Effenberger H, Witzel U, Lintner F, Rieger W (2001) Stress analysis of threaded cups. Int Orthop 25:228–235
Fernandez-Gonzalez J, Canosa Sevillano R, Garcia-Araujo C (1997) Cementless total hip arthroplasty with a threaded acetabular cup. Int Orthop 21:327–331
Fox GM, McBeath AA, Heiner JP (1994) Hip replacement with a threaded acetabular cup. A follow-up study. J Bone Joint Surg Am 76:195–201
Garcia-Cimbrelo E, Cruz-Pardos A, Cordero J, Sanchez-Sotelo J (2000) Low-friction arthroplasty in patients younger than 40 years old: 20- to 25-year results. J Arthroplasty 15:825–832
Grubl A, Chiari C, Gruber M, Kaider A, Gottsauner-Wolf F (2002) Cementless total hip arthroplasty with a tapered, rectangular titanium stem and a threaded cup: a minimum ten-year follow-up. J Bone Joint Surg Am 84:425–431
Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 51:737–755
Havelin LI, Espehaug B, Engesaeter LB (2002) The performance of two hydroxyapatite-coated acetabular cups compared with Charnley cups. From the Norwegian Arthroplasty Register. J Bone Joint Surg Br 84:839–845
Herberts P, Malchau H (2000) Long-term registration has improved the quality of hip replacement: a review of the Swedish THR Register comparing 160,000 cases. Acta Orthop Scand 71:111–121
Huiskes R (1987) Finite element analysis of acetabular reconstruction. Noncemented threaded cups. Acta Orthop Scand 58:620–625
Inoue S, Kubo T, Maeda T, Hirakawa K, Koshino T, Wu Y, Ueshima K, Ogura T, Hirasawa Y (2001) Minimum ten-year follow-up clinical and radiographic results of Mark I and Mark II Lord type femoral component in total hip arthroplasty. J Orthop Sci 6:327–332
Kody MH, Kabo JM, Markolf KL, Dorey FJ, Amstutz HC (1990) Strength of initial mechanical fixation of screw ring acetabular components. Clin Orthop 257:146–153
Kubo T, Inoue S, Maeda T, Arai Y, Hirakawa K, Wu Y, Suehara H, Ogura T, Hirasawa Y (2001) Cementless Lord total hip arthroplasty: cup loosening common after minimum 10-year follow-up of 103 hips. Acta Orthop Scand 72:585–590
Malchau H, Herberts P, Wang YX, Karrholm J, Romanus B (1996) Long-term clinical and radiological results of the Lord total hip prosthesis. A prospective study. J Bone Joint Surg Br 78:884–891
Mallory TH, Vaughn BK, Lombardi AV Jr, Reynolds HM Jr, Koenig JA (1988) Threaded acetabular components. Design rationale and preliminary clinical experience. Orthop Rev 17:305–314
Manley MT, Capello WN, D’Antonio JA, Edidin AA, Geesink RG (1998) Fixation of acetabular cups without cement in total hip arthroplasty. A comparison of three different implant surfaces at a minimum duration of follow-up of five years. J Bone Joint Surg Am 80:1175–1185
Martell JM, Berdia S (1997) Determination of polyethylene wear in total hip replacements with use of digital radiographs. J Bone Joint Surg Am 79:1635–1641
Morscher E, Schmassmann A (1983) Failures of total hip arthroplasty and probable incidence of revision surgery in the future. Calculations according to a mathematical model based on a ten years’ experience in total hip arthroplasty. Arch Orthop Trauma Surg 101:137–143
Morscher EW (1992) Current status of acetabular fixation in primary total hip arthroplasty. Clin Orthop 274:172–193
Murray DW, Carr AJ, Bulstrode C (1993) Survival analysis of joint replacements. J Bone Joint Surg Br 75:697–704
Pandit HG, Hand CJ, Ramos JL, Pradham NS, Boyd NA (1999) Middle-term results of a cementless threaded self-tapping acetabular cup. J R Nav Med Serv 85:174–177
Pupparo F, Engh CA (1991) Comparison of porous-threaded and smooth-threaded acetabular components of identical design. Two- to four-year results. Clin Orthop 271:201–206
Rokkum M, Brandt M, Bye K, Hetland KR, Waage S, Reigstad A (1999) Polyethylene wear, osteolysis and acetabular loosening with an HA-coated hip prosthesis. A follow-up of 94 consecutive arthroplasties. J Bone Joint Surg Br 81:582–589
Simank HG, Brocai DR, Reiser D, Thomsen M, Sabo D, Lukoschek M (1997) Middle-term results of threaded acetabular cups. High failure rates five years after surgery. J Bone Joint Surg Br 79:366–370
Udomkiat P, Dorr LD, Wan Z (2002) Cementless hemispheric porous-coated sockets implanted with press-fit technique without screws: average ten-year follow-up. J Bone Joint Surg Am 84:1195–1200
Xenakis TA, Gelalis J, Koukoubis TA, Zaharis KC, Soucacos PN (2001) Cementless hip arthroplasty in the treatment of patients with femoral head necrosis. Clin Orthop 386:93–99
Yahiro MA, Gantenberg JB, Nelson R, Lu HT, Mishra NK (1995) Comparison of the results of cemented, porous-ingrowth, and threaded acetabular cup fixation. A meta-analysis of the orthopaedic literature. J Arthroplasty 10:339–350
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aldinger, P.R., Thomsen, M., Lukoschek, M. et al. Long-term fate of uncemented, threaded acetabular components with smooth surface treatment: minimum 10-year follow-up of two different designs. Arch Orthop Trauma Surg 124, 469–475 (2004). https://doi.org/10.1007/s00402-004-0709-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-004-0709-y