Abstract
Introduction
Complex femoral fractures pose considerable therapeutic challenges to orthopedic surgeons. We present a retrospective review of 25 patients with complex femoral fractures treated with intramedullary locked nailing and supplemental screw fixation.
Materials and methods
Fifteen patients with ipsilateral femoral neck and shaft fractures (group 1) and 10 patients with ipsilateral femoral shaft and distal femur fractures (group 2) were treated from 1990 to 1998. High-energy injuries occurred in all patients. There were 4 open fractures. Antegrade, locked nailing of diaphyseal fractures was performed in all cases. Supplemental screws for the neck were used in all patients in group 1 and in 3 patients in group 2.
Results
All of the fractures united during the follow-up. Five patients in group 1 underwent reoperation (33.3%): one due to a delayed union, the second due to an implant failure, the third due to a nonunion of a neck fracture, and the last two because of an initially missed femoral neck fracture. None of the patients in group 2 underwent reoperation. Angular malalignment of the shaft was found in 6 fractures in group 1 (average 4.8o, range 3o–11o) and in 4 fractures in group 2 (average 6o, range 3o–12o). Shortening of the limb occurred in 3 patients in group 1 (average 1.4 cm, range 1–1.8) and in 1 patient in group 2 (2 cm). Loss of fixation was seen in 1 patient in each group. Avascular necrosis and infection were not seen in any case in both groups.
Conclusion
Femoral intramedullary nails with antegrade or retrograde options for insertion and different locking possibilities have extended the indications to include both diaphyseal and metaphyseal fractures. New nail designs, usually more expensive than the conventional nails, have been introduced into the market for this purpose. One has to keep in mind that antegrade, locked nailing of femoral shaft fractures combined with neck or distal femur fractures is a technically demanding but efficacious procedure. The success rate is high when the technique is meticulously implemented.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ipsilateral fractures of the femoral shaft and neck or shaft and distal part of the femur are rare but challenging combinations of injuries [5, 28, 29]. The choice of treatment should be early fracture stabilization, especially in patients with polytrauma [15]. The rare occurrence of these concomitant fractures creates a dilemma concerning the ideal fixation method. There are nearly 60 recommended methods of treatment for this type of fracture in the literature [9, 28], but no method has been established as the gold standard [10, 32]. Ideally, adequate stabilization of this type of fractures should be achieved by stable internal fixation devices [2, 12, 14, 20, 35].
The choice of treatment at our institutions for shaft fractures of the femur and tibia involves closed reduction and intramedullary nailing. In the beginning, a conventional 'Küntscher nail' with reaming was used. This nailing technique was changed to closed, reamed, locked intramedullary nailing as popularized by Kempf et al. [19]. We still treat isolated femoral or tibial shaft fractures using this technique, but in cases of polytrauma or multiple fractures, we prefer unreamed intramedullary nailing.
The efficacy of closed, locked, intramedullary nailing in patients with complex fractures of the femoral shaft has been well established [3, 18, 19]. Thus, we considered this technique as appropriate for the stabilization of femoral shaft fractures combined with neck or distal femur fractures at the beginning of 1990.
This retrospective study reports the results of these uncommon fracture combinations, treated with the standard technique of antegrade, locked, femoral nailing with supplemental screw fixation of the neck or distal femur.
Patients and methods
During the 9-year period from January 1990 to December 1998, 144 complex femoral shaft fractures in 140 patients were treated with locked intramedullary nailing at the Department of Orthopaedics & Traumatology of Ege University, Medical Faculty, İzmir, Turkey.
Among them, 18 patients (12.5%; group 1) also had a femoral neck fracture, and 11 (7.6%; group 2) had a concomitant supracondylar or intercondylar fracture. A total of 28 patients who had an ipsilateral femoral shaft and neck fracture or femoral shaft and distal femur fracture fulfilled the entry criteria and were subsequently enrolled in the study between 1990 and 1998. All skeletally mature patients with nonpathologic fractures were considered for the study after obtaining the approval of the ethical committee for this clinical trial. The Injury Severity Score (ISS) was used to estimate the severity of trauma in both groups [4]. Prospective data collection in both patient groups was aborted due to the limited number of patients. Data were processed retrospectively from their medical records and radiographs. One patient died in group 1 before review because of a head injury, 2 patients in group 1 and 1 patient in group 2 could not be traced because they changed addresses and telephone numbers. Therefore, a total of 4 patients were excluded from the study, leaving 15 patients in group 1 and 10 patients in group 2 for analysis. All preoperative and postoperative radiographs were reviewed by us to classify the fractures using the AO Comprehensive Classification of Fractures of Long Bones [23] and also to identify instances of loss of reduction, loss of fixation, and malunion. The patients were reexamined by one of the authors (KA) at the last follow-up.
Group 1 consisted of 14 men and 1 woman with an average age of 36.2 years (range 22–57 years). The left side was involved in 11 cases and the right side, in 4 (Fig. 1). The mechanism of injury in all patients was high-energy trauma: 12 were injured in motor vehicle accidents, 1 was injured in a motorcycle accident, and 2 were injured due to a fall from a height. Eight patients sustained associated injuries, including 3 upper extremity fractures, 1 contralateral femur fracture, 2 contralateral tibia fractures, 1 ipsilateral tibia fracture, 1 thoracic vertebra fracture, 1 pelvic fracture, 2 major head injuries, and 1 thorax injury (Table 1).
In group 2 (7 men and 3 women), the average age was 34.7 years (range 16–44 years). The left side was involved in 7 cases and the right side, in 3 (Fig. 2). All injuries also resulted from high-energy trauma: 8 were injured in motor vehicle accidents, 1 was injured in a motorcyle accident, and the last one fell from a height. All patients sustained associated injuries including 6 upper extremity fractures, 4 ipsilateral tibia fractures, 1 contralateral femur fracture, 1 contralateral ankle fracture, 1 contralateral talus fracture, 1 head injury, 1 facial injury, and 1 thorax injury (Table 2).
Anteroposterior radiograph showing a fracture of the femoral shaft and ipsilateral distal part of the femur. b Anteroposterior radiograph taken 21 months after interlocking nailing with supplemental screws showing union of diaphyseal fracture. c Anteroposterior radiograph taken 21 months after interlocking nailing with supplemental screws showing union of distal femoral fracture
There were two open diaphyseal fractures in each group; one of the fractures in group 1 was Gustilo-Anderson type I and the other type II, while both open fractures in group 2 were type I [16]. After initial resuscitation, the open fractures were treated with immediate debridement and irrigation. The fractures were placed on skeletal traction upon admission in patients whose medical condition was unstable until definitive surgical stabilization, which was accomplished in 72 h after injury in all patients. Locked nailing was the only method of treatment employed in the patients. One of the authors (KA) performed all the operations in both groups.
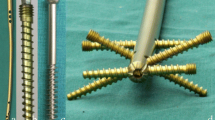
All patients in group 1 underwent closed, antegrade intramedullary nailing of the shaft before the stabilization of the neck. The surgeon preferred to fix shaft fractures prior to neck fractures . In five patients, a Grosse-Kempf (Howmedica International, London, UK) reamed, locked nail was used to stabilize the shaft fracture and then two or three 6.5 mm, partially threaded, cannulated, self-cutting and self-tapping, cancellous screws (Howmedica) were put around the nail to fix the neck fracture. In 10 patients, stabilization of the shaft fracture was achieved with a standard antegrade, unreamed, femoral nail (Mathys Osteosynthesis, Bettlach, Switzerland) first, and then the neck fracture was fixed by placing two 6.5 mm, partially threaded, cannulated, self-cutting and self-tapping, cancellous screws around the nail, except for 1 patient who required three screws to provide adequate stability. All nailings were performed using a fracture table under fluoroscopic control. Reductions were achieved in the standard closed fashion in all patients without performing a capsulotomy for the neck fracture. The starting hole for the nail was placed as posteriorly as possible in order to be able to insert two screws anteriorly through the neck. Prior to insertion of the locking screws, the length and rotation of the femur were assessed clinically and radiographically in all patients. The proximal locking screws of the nail were inserted by using the manufacturer's proximal targeting devices. The distal screws and femoral neck screws were inserted by 'free-hand technique' under fluoroscopic control. All the nails were statically locked. Two distal screws and one proximal oblique screw were used for the Grosse-Kempf nail, and two transverse proximal and distal screws were used for the unreamed femoral nail.
In group 2, patients were positioned supine on a radiolucent operating table. A rolled sheet was placed under the sacrum and the lumbar spine as well as under the ipsilateral shoulder to elevate the affected hip by 20–40o. The entire limb was then draped free and included in the sterile field. In the case of an intraarticular distal femoral fracture, adequate visualization of the alignment of the articular cartilage was obtained through a small lateral parapatellar arthrotomy. Two 6.5 mm, partially threaded, cannulated, self-cutting and self-tapping, cancellous lag screws with washers were used for preliminary fixation of the femoral condyles. Care was taken to insert these screws into the anterior and posterior portion of the condyles to prevent them from impeding the insertion of the nail into the distal fragment of the femur. Then, an assistant reduced the shaft fracture using manipulation and longitudinal traction and maintained fracture reduction throughout the nailing procedure. We had to cut off the distal tip of the nail to allow for more distal placement of the locking screws in one patient. For an extraarticular distal femoral fracture, stabilization was achieved with closed, static locked nailing like a segmental fracture. In group 2, antegrade, unreamed, femoral nails with two transverse screws proximally and distally were used in all patients (Mathys Osteosynthesis).
Open reduction was not necessary for any shaft fracture in either group. All patients received perioperative and postoperative antibiotics for 2 days. Postoperatively, isometric quadriceps strengthening, active and passive range-of-motion exercises were started as early as possible in all patients. The patients were encouraged to walk with toe-touch weight-bearing using crutches if their physical condition permitted, followed by progressive weight-bearing depending on the assessment of the stability of the fixation. Full weight-bearing was initiated when bridging callus was visible on two orthogonal radiographs. In group 2, continuous passive motion was used additionally for the knee for a period of 5–7 days. Follow-up was done at 4, 8, and 12 weeks and 6 and 12 months during the 1st year. The patients were evaluated regarding fracture union and function of the limb. The range of movement of the hip and knee was measured each time and at the last follow-up. The functional assessment of the patients in group 1 was done according to the rating system of Friedman and Wyman [12] and in group 2, according to the rating system of Sanders et al. for distal femoral fractures [26]. Union was defined as a bridging callus on two orthogonal radiological views with no pain on standing and no tenderness to palpation. Shortening was assessed radiologically by scanogram, with a radioopaque ruler being placed between the limbs, from which direct measurement of both femoral lengths was made. For malunion, goniometric measurements were made on anteroposterior weight-bearing radiographs to determine coronal plane angulation and on weight-bearing lateral radiographs to determine sagittal plane angulation. Contralateral femur radiographs were used as a template.
Results
All fractures were followed to union. The mean ISS of group 1 was 12.4±3.1. The mean operative time was 141.6±20.2 min (range 115–180 min), and the mean fluoroscopy time was 60.3±7.7 s (range 45–72 s) in group 1. The mean follow-up period was 78 months (range 52–150 months). The average time from injury to fixation of the neck fractures was 3 days. The mean time to radiographic union was 4.8±0.77 months in the neck. All but one of the neck fractures united after the primary fixation. One patient with nonunion of the neck healed eventually with intertrochanteric valgus osteotomy after nail removal which was performed at 12 months post-injury. Avascular necrosis of the femoral head was not seen during the follow-up period. Fixation failure of the neck occurred in only 1 patient who had varus nonunion. The mean time to union for the shaft fracture was 6.1±2.1 months. In two patients, the fractures failed to unite after the primary fixation. In one patient, nail breakage occurred at the end of the 3rd month. This was managed by removal of the broken nail and replacement with a new and thicker, reamed, femoral nail. In the other, delayed union occurred in the shaft at the end of 5th month; this was managed by reaming the medullary canal and exchanging the nail. Both fractures subsequently united without requiring dynamization of the nail. Angulation in the coronal or sagittal planes of less than 5° was noted in 5 patients (average 4o, range 3–5o). One patient had 11° of angulation in the sagittal plane. Three patients had limb shortening of 1, 1.4, and 1.8 cm, respectively (average 1.4 cm).
The latest follow-up examination revealed that in 14 patients the average hip and knee motion was at least 80% of that of the opposite side and pain-free. Fourteen patients were graded as 'good'. The patient with varus nonunion of the neck had a fair outcome. He was also managed by below-knee amputation because of a failed reconstruction of a contralateral type III-C open tibial fracture. Excluding this patient, all patients regained their pre-injury level of independence.
In 4 patients, the femoral neck fracture was initially unrecognized in the emergency department (26.6%). In 1 of them, the fracture was recognized intraoperatively on the fracture table while trying to reduce the shaft fracture and was treated with additional screws. Postoperative radiographs revealed the neck fracture in a second patient on the 2nd postoperative day, while in a third, CT scans taken to evaluate hip pain revealed it on the 3rd postoperative day. Both patients were reoperated to place additional screws around the 'in situ' nail. In the last patient, the neck fracture was detected incidentally on a preoperative CT scan of the pelvis that was obtained to assess the pelvic fracture.
The mean ISS of group 2 was 12±2.8. The mean operative time was 125.2±24 min (range 90–162 min), and the mean fluoroscopy time was 55.7±14.2 s (range 42–81 s). The mean follow-up period was 53.8 months (range 36–72 months). All of the shaft and condylar fractures united after primary stabilization. No further operative procedures was performed in any patient. The average time to union was 4.6±1.1 months in the distal femur and 5.4±1.3 months in the shaft.
Angulation of the shaft in the coronal and sagittal planes measured less than 5° in 3 patients (average 4o, range 3–5o). There was one patient who had 12° of angulation of the shaft in the sagittal plane. One patient had a limb shortening of 2 cm. Complications like loss of fixation, loss of reduction, or malunion occurred in only 1 patient in the distal femur. This patient, with a T-shaped condylar fracture of the distal femur, had had an anatomical reduction during fixation. However, he lost this reduction because of loosened cancellous screws and eventually healed with 3 mm of articular cartilage 'step-off'. One patient had a cancellous screw of the inappropriate length, resulting in irritation of the medial collateral ligament and soft tissues; it was removed immediately after union. Three patients had 3–5 mm backing-out of the most distal screw, used to lock the nail, and 1 patient had a nail breakage at the most distal locking hole. Since the stability of the bone-nail complex was preserved in both cases, the fractures healed free of complications.
According to Sanders et al., two patients had an excellent result, seven had a good result, and only the patient with the T-shaped intercondylar fracture was rated as fair [26]. There was no poor functional result.
At latest follow-up examination, the range of motion was 90° in one knee, 100° in five knees, and 120° or more in four knees. There was no ligament instability nor flexion contracture of the knee. All but one patient had no pain during daily activities. One patient had mild pain around the knee, but it was not severe enough to necessitate the use of analgesics. No posttraumatic arthritis of the knee has been noted to date.
No case of deep infection was seen in this series. No cases of fat embolism syndrome or adult respiratory distress syndrome arose. Appropriate surgical stabilization of the associated long-bone fractures was done in all patients.
Discussion
Complex femoral fractures continue to be problematic for the treating surgeon and the patient. There is no doubt that these fractures are best managed by surgical stabilization [2, 5, 9, 12]. Early stabilization of long-bone fractures followed by early mobilization has been shown to decrease morbidity and mortality, especially in polytrauma patients [6, 15]. However, controversies still remain regarding the most appropriate internal fixation device and which fracture should be given surgical priority [25, 32]. Several investigators recommend immediate reduction and stabilization of the femoral neck fracture, as an orthopedic emergency, because of serious potential consequences of femoral neck fractures such as avascular necrosis, nonunion, and secondary displacement [9, 14, 29]. However, a delay in fixation of days to weeks does not seem to increase the complication rate [5, 7, 32, 34, 35].
Controversy also exists as to which internal fixation device to use for stabilization of the shaft fractures [25, 32]. The key for union is to obtain stable fixation regardless of the type of fixation technique used [2, 5, 9]. Several authors recommend plating the shaft, while others propose fixing it by retrograde intramedullary nailing [11, 13, 14, 30]. Avoiding possible complications of plate fixation like a large surgical dissection and significant soft-tissue trauma, considerable blood loss, potentially higher infection risk, refracture, and implant failure, antegrade, locked nailing still seems to be a logical option to stabilize the shaft fracture [1, 2, 3]. Among 33 cases reported by Wu et al., the shaft fracture was plated in a group of 10, and all major complications occurred in this group. He stressed the technique of closed, antegrade, locked nailing of the shaft fracture followed by screw fixation of the neck [34].
Leung et al. reported 16 cases treated by antegrade, locked nailing with supplemental screw fixation of the neck fracture. In his series, all the shaft and neck fractures healed uneventfully with no evidence of avascular necrosis, and there was only one delayed union of a neck fracture [22]. Wiss et al. treated 33 cases with antegrade, reamed nailing combined with cancellous screw fixation of the neck. He concluded that this method had not produced uniformly reliable results as attributable to higher rates of varus nonunion of the neck fracture. However, he utilized a reversed Grosse-Kempf nail in 13 patients, and virtually all of the nonunions were noted in this group, probably related to the fracture-distracting effect of the proximal locking screw [31].
Another option for fixation of both fractures is a second-generation interlocking nail; however, this technique may compromise the reduction and fixation of the femoral neck and may lead to complications. It is very critical to determine the rotational alignment of this construct to avoid malalignment of the proximal locking screws across the femoral neck [7, 24, 31, 32].
The standard regimen of treatment for distal femoral fractures, with or without intraarticular extension, involves open reduction and internal fixation with plates and screws [17, 27]. However, if a fracture of the distal part of the femur occurs in conjunction with an ipsilateral shaft fracture, simultaneous fixation of this rare fracture combination will pose a challenging situation to the surgeon. Open plating of both fractures with a long side-plate or multiple plates is a possible choice for this rare injury. But one should take the possible complications into account when considering this type of fixation. In 10 of the 13 cases treated by Wood et al. with plates, 6 major complications were encountered [33].
Antegrade, closed, locked nailing of this type of fracture combined with the placement of cancellous lag screws for the intercondylar portion of these injuries is another possible choice [8, 21]. Butler et al. presented a series of 23 patients who had a fracture of the femoral shaft with an accompanying ipsilateral supracondylar or intercondylar fracture. All of the fractures were treated with antegrade, locked nailing and supplemental screw fixation whenever the distal fracture was intraarticular. The complication necessitating reoperation was an initially unrecognized fracture of the femoral condyle in the frontal plane in two patients. None of the patients experienced an implant failure [8]. It is well recognized that fixation with two lag screws, without buttress plating, has not been considered an appropriate stabilization for intraarticular distal femoral fractures. However, avoidance of metaphyseal-diaphyseal soft-tissue stripping and devitalization of the metaphysis by large surgical incisions are the major advantages of locked nailing. Besides, stable but not necessarily rigid fixation connecting the distal femur to the proximal femur usually allows early rehabilitation. Union of all fractures with good or excellent motion of the knee in 9 of our 10 patients led us to prefer antegrade, locked nailing in these concomitant fractures.
Although this study is limited by its retrospective nature, the findings suggest that the management of femoral shaft fractures combined with neck or distal femur fractures can be accomplished very successfully with antegrade, locked nails.
References
Aktuglu K, Oncag H, Alin G (1995) Ipsilateral fractures of the femoral neck and shaft (in Turkish). J Arthroplasty Arthrosc Surg 6:32–35
Alho A (1997) Concurrent ipsilateral fractures of the hip and shaft of the femur. A systematic review of 722 cases. Ann Chir Gynaecol 86:326–336
Alho A, Ekeland A, Grogaard B et al (1996) A locked hip screw–intramedullary nail (cephalomedullary nail) for the treatment of fractures of the proximal part of the femur combined with fractures of the femoral shaft. J Trauma 40:10–16
Baker SP, O'Neill B, Haddon W Jr, Long WB (1974) The Injury Severity Score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 14:187–196
Bennett FS, Zinar DM, Kilgus DJ (1993) Ipsilateral hip and femoral shaft fractures. Clin Orthop 296:168–177
Bone LB, Johnson KD, Weigelt J, Scheinberg R (1989) Early versus delayed stabilization of femoral fractures. A prospective randomized study. J Bone Joint Surg Am 71:336–340
Bose WJ, Corces A, Anderson LD (1992) A preliminary experience with the Russell-Taylor reconstruction nail for complex femoral fractures. J Trauma 32:71–76
Butler MS, Brumback RJ, Ellison S et al (1991) Interlocking intramedullary nailing for ipsilateral fractures of the femoral shaft and distal part of the femur. J Bone Joint Surg Am 73:1492–1502
Casey MJ, Chapman MW (1979) Ipsilateral concomitant fractures of the hip and femoral shaft. J Bone Joint Surg Am 61:503–509
Chaturvedi S, Sahu SC (1993) Ipsilateral concomitant fractures of the femoral neck and shaft. Injury 24:243–246
Chen CH, Chen TB, Cheng YM, Chang JK, Lin SY, Hung SH (2000) Ipsilateral fractures of the femoral neck and shaft. Injury 31:719–722
Friedman RJ, Wyman ET Jr (1986) Ipsilateral hip and femoral shaft fractures. Clin Orthop 208:188–194
Geissler WB, Savoie FH, Culpepper RD, Hughes JL (1989) Operative management of ipsilateral fractures of the hip and femur. J Orthop Trauma 2:297–302
Gill SS, Nagi ON, Dhillon MS (1990) Ipsilateral fractures of the femoral neck and shaft. J Orthop Trauma 4:293–298
Goris RJA, Gimbrere JSF, Van Niekerk JL et al (1982) Early osteosynthesis and prophylactic mechanical ventilation in the multiple trauma victim. J Trauma 22:895–903
Gustilo RB, Anderson JT (1976) Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones. Retrospective and prospective analyses. J Bone Joint Surg Am 58:453–458
Johnson KD, Hicken G (1987) Distal femoral fractures. Orthop Clin North Am 18:11–132
Johnson KD, Tencer AF, Blumenthal S et al (1986) Biomechanical performance of locked intramedullary nail systems in comminuted femoral shaft fractures. Clin Orthop 206:151–161
Kempf I, Grosse A, Beck G (1985) Closed locked intramedullary nailing. J Bone Joint Surg Am 67:709–720
Lambiris E, Megas P, Karioris G, Giannikas D (2000) Combined femoral shaft and proximal femur fractures treated with intramedullary nailing. Osteosyn Int [Suppl 1] 8:155–157
Leung KS, Shen WV, So WS, Mui LT, Grosse A (1991) Interlocking intramedullary nailing for supracondylar and intercondylar fractures of the distal part of the femur. J Bone Joint Surg Am 73:332–340
Leung KS, So WS, Lam TP, Leung PC (1993) Treatment of ipsilateral femoral shaft fractures and hip fractures. Injury 24:41–45
Murphy WM, Leu D (2000) Fracture classification: biological significance. In: Rüedi TP, Murphy WM (eds) AO principles of fracture management. Thieme, Stuttgart, pp 45–58
Parfenchuck TA, Carter LW, Young TR (1993) Ipsilateral fractures of the femoral neck and shaft. Orthop Rev 22:356–363
Plancher KD, Donshik JD (1997) Femoral neck and ipsilateral neck and shaft fractures in the young adult. Orthop Clin North Am 28:447–459
Sanders R, Swiontkowski MF, Rosen H, Helfet D (1991) Double-plating of comminuted, unstable fractures of the distal part of the femur. J Bone Joint Surg Am 73:341–346
Schatzker J, Lambert DC (1979) Supracondylar fractures of the femur. Clin Orthop 138:77–83
Swiontkowski MF (1987) Ipsilateral femoral shaft and hip fractures. Orthop Clin North Am 18:73–83
Swiontkowski MF, Hansen ST, Kellam J (1984) Ipsilateral fractures of the femoral neck and shaft. J Bone Joint Surg Am 66:260–268
Wellin DE, Galloni L, Gelb RI (1984) Ipsilateral intertrochanteric diaphyseal femoral fractures. Four patients treated by one technique. Clin Orthop 183:71–75
Wiss DA, Sima W, Brien WW (1992) Ipsilateral fractures of the femoral neck and shaft. J Orthop Trauma 6:159–166
Wolinsky PR, Johnson KD (1995) Ipsilateral femoral neck and shaft fractures. Clin Orthop 318:81–90
Wood EG, Savoie FH, Vander Griend RA (1991) Ipsilateral supracondylar and shaft fractures of the femur. J Orthop Trauma 5:177–183
Wu CC, Shih CH (1991) Ipsilateral femoral neck and shaft fractures. Acta Orthop Scand 62:346–351
Zettas JP, Zettas P (1981) Ipsilateral fractures of the femoral neck and shaft. Clin Orthop 160:63–73
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Okcu, G., Aktuglu, K. Antegrade nailing of femoral shaft fractures combined with neck or distal femur fractures. Arch Orthop Trauma Surg 123, 544–550 (2003). https://doi.org/10.1007/s00402-003-0584-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-003-0584-y