Abstract
Purpose
Sufficient anchoring of intramedullary osteosynthesis in the femoral head in a femoral neck fracture is a challenge with increasing age of the patients and decreasing bone quality. For older patients with inferior bone quality, it has not been investigated whether the application of an intramedullary force carrier, as a minimally invasive and rapid intervention, can provide a considerable benefit and reduce the postoperative complication and lethality rate. This retrospective study aimed to investigate the stability and functionality after the acute treatment of a femoral neck fracture in osteoporotic bone using an intramedullary force carrier even with higher grade fracture types.
Material and Methods
The retrospective analysis was based on a collective of 82 patients over 60 years of age with a femoral neck fracture treated with a gliding nail in our centre between 1999 and 2006.
Results
The average time to follow-up was 69.05 months (median 71.0; minimum 27.0–maximum 108.0). Female patients made up more than two-thirds of the patient collective at 63 of the 82 patients (76.83%). The average age of the patients was 77.76 years (median 78.00; range 60.00–93.00).
In 66 patients (80.49%), the implantation showed good results and no complications or further treatments. 24/82 patients of our collective had died in our re-evaluation. In no case, a pseudarthrosis or severe impaction with neck shortening occurred (loss of offset).
11/82 patients had femoral head necrosis which led to total hip replacement in 8 cases, a hemiarthroplasty in 2 cases and in 1 case a remaining Girdlestone situation because of a deep infection. Another five patients also had to undergo a total hip replacement because of a central perforation of the blade in one case, breakout of the blade after another fall in another two cases and a lateral dislocation of the blade in two cases.
Conclusion
The use of an intramedullary force carrier in the osteoporotic bone can mean distinct advantages for the selected patient as a minimally invasive and rapid surgical method compared to extensive surgery, even in the case of severe injuries. However, the advantages and disadvantages for the patient should be considered critically.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Femoral neck fracture is one of the most common fractures in older people, with an incidence of around 100,000 per year in Germany, and approximately 30% of all the women are affected [1, 2]. Due to an increase in the elderly population, there is an associated increase in osteoporosis and subsequent loss of stability in the proximal femur, hence, this injury will increase in importance in the coming years [3,4,5].
To the best of our knowledge, femoral neck fracture has always been one of the most problematic fractures; therefore, research is continuously focused on its adequate therapy. The goal of such therapy is a fast, load-bearing, anatomical restoration of hip joint functionality, as well as early mobilisation to avoid immobility and the consecutively increasing risk of further illness. Even though there are modern treatment methods, postoperative complications are still prevalent, and there still remains an applicable rate of postoperative mortality which increases with any delay in the operative treatment [6,7,8,9,10,11]. For this reason, within the quality management criteria in Germany there is a recommendation that a patient who is to receive treatment with osteosynthesis should be operated on within the first 24 h.
It was already demonstrated in the past century that the correct surgical therapy is superior to non-operative therapy for proximal complex fractures of the femur [12,13,14,15]. There is a consensus that less displaced fractures and femoral neck fractures with less displacement in younger patients and patients with a high activity level should receive treatment with osteosynthesis, while preserving the head. In recent decades, various implants have been developed and continuously improved upon for this purpose Noteworthy implants in recent years are dynamic hip screws (DHSs) and intramedullary implants with neck screws [16,17,18,19,20] and these have been established as effective and safe implants for the treatment of femoral neck fractures. However, complications are also known regarding these implants; e.g. femoral head necrosis, non-unions, and displacements, as well as implant-specific and biomechanical complications.
Alternatively, as early as 1992, the gliding nail (GN) with the unique feature of an impacting blade was introduced as an intramedullary top weighting arm with increased surface area and rotational stability using a double-T cutting edge. The advantages of a higher load capacity, combined with higher rotational stability and a lower cut-out rate than the gamma nail, should lead to the optimal treatment of patients and a lower postoperative rate of complications and mortality [21]. This advantage of the gliding nail has already been demonstrated in per- and subtrochanteric fractures and in experimental settings [21, 22].
For this reason, the following questions arise: (1) can the indication for the use of an implant, with such high rotational stability and impact, also be extended to the femoral neck fracture in older patients and osteoporotic bone after individual consideration; (2) what outcome can be expected?
Patients and Methods
82 patients over 60 years of age with a femoral neck fracture were treated with a gliding nail in our centre between 1999 and 2006 and they were eligible for inclusion in this retrospective study. The re-examination was in 2008. The average time of follow-up was 69.05 months (median 71.0; minimum 27.0–maximum 108.0). Out of 82 patients, 63 were female thus constituting the majority portion of the patient collective (76.83%). The average age of the patients was 77.76 years (median 78.00; range 60.00–93.00). Of the total data, parts were previously published in 2005 during an earlier study [23].
Criteria for Inclusion
Criteria for inclusion in the study were the following: all patients over 60 years of age who were treated with an intramedullary nail with Garden I and II fractures; as well as Garden III and IV fractures [24, 25]. Patients with cervical base fractures, lateral femoral neck fractures, and femoral neck non-unions were also included. Patients who had contraindications against a therapy to preserve the femoral head via treatment with osteosynthesis were not included. All patients were asked for their permission regarding the evaluation of their data, and they all gave their approval. All data were archived anonymously.
Indication
In our trauma centre, patients over 65 years of age, or elderly patients having an assessment of their biological age, receive surgical treatment for a femoral neck fracture according to their individual injury, their individual state of health, and their activity level. Usually, active elderly patients with a non- or slightly displaced fracture were treated with osteosynthesis. Elderly patients with a displaced fracture were usually treated with a hemi- or total endoprosthesis. If the patient is at the age limit or biologically younger (i.e. very good general condition, few previous illnesses, and good mobility), in some cases we also use the intramedullary nail for impacted and non-displaced medial femoral neck fractures (Garden I and II). In the case of a non-active patient in combination with a displaced medial femoral neck fracture (Garden III and IV), we use the intramedullary nail only as a stabilising operation if a major operation, such as implantation of a prosthesis, would be detrimental to a patient’s health or the surgical risk is too high; so that stability in the bone is achieved and the patient can be properly positioned and provided with healthcare.
Data Evaluation and Ethical Approval
Data evaluation in 2008 was performed based on collected patient data, such as medical history, imaging results, anaesthesia protocols, surgery reports, nurse reports, physiotherapy protocols, and the corresponding admission notes. Patients were also contacted after treatment and asked to participate in a standardised questionnaire which included questions about their daily life activities, pain, mobility, other operations, or medication.
Due to the international usage of these systems, fractures were classified according to Garden [24, 25] and Pauwels [26]. Displacement in the frontal and sagittal plane was evaluated using deep pelvis radiography and axial hip radiography. A supplementary CT scan was only necessary in a few cases.
This study was approved by the Ethics Committee of the Medical Faculty at the University of Heidelberg, Germany. Hence, the study was approved by the review board and conducted according to the review board guidelines and within the bounds of good clinical practice, according to the ethical principles that have their origin in the Declaration of Helsinki in its current form. As aforementioned, all patients were asked for permission for evaluation of their data, and they all gave their approval. All data were archived anonymously. Data analyses were performed using IBM SPSS® Statistics 25.
Implants Used
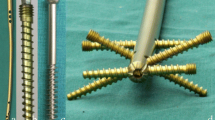
The gliding nail (GN) is an implant that combines: (1) the advantages of the locking nail system and the flap gliding principle, and (2) the dynamisation in the thighward direction as well as in the direction of the femoral shaft, with (3) the advantages of the double-T profile of the femoral neck load bearer (Figs. 1a, b, 2). The double-T profile of the blade has the highest moment of resistance for a given cross-sectional area (Fig. 2). Further, the rotation of the head-neck fragment with a screw breakout from the cranial fragment is effectively prevented by the double-T profile of the blade design; in that, a rotation of the proximal fragment around the blade is not possible. A further decisive advantage is that the blade, in a similar manner to a nail, is driven into the bone. This results in additional bone impaction and thus there is no loss of bone substance in a similar manner to local spongiosaplasty.
Postoperative Rehabilitation Protocol
On the first day after the surgery, physiotherapy under full load was started for all patients with a Garden I or II fracture. According to the current therapy recommendation of a relief in displaced femoral neck fracture in younger patients, we also recommend a temporary partial load of 20 kg in the first 6 weeks for patients with Garden III and IV fractures. Complete healthcare and bedding were permitted for those patients requiring comprehensive nursing care.
Results
Fracture and Age Distribution
In our collective of 82 patients, the mean age of patients was 77.76 years (median 78.00, range 60.00–93.00); as aforementioned, female patients made up the majority of the collective with 63 out of a total of 82 patients. We divided our collective into three groups based on their injuries: group A corresponds to Garden I and II (Pauwels 1/2) fractures, group B corresponds to Garden III and IV (Pauwels 2/3), and group C corresponds to base cervical/lateral femoral neck fractures. Distribution of patients in the groups was as follows: group A included 69 patients with an average age of 77.64 years (median 78.00, range 62.00–93.00), of whom 14 were male and 55 were female. Group B consisted of eight patients with an average age of 75.38 years (median 76.50, range 60.00–92.00) and gender distribution of three men and five women. Group C consisted of five patients with an average age of 83.20 years (median 83.00, range 77.00–90.00) and gender distribution of two men and three women. The characteristics of the collective are provided in Tables 1 and 2.
Complications
In 66 patients (80.49%), the implantation showed good results and no complications or further treatments. In none of the cases, a pseudarthrosis or severe impaction with neck shortening had been detected (i.e. loss of offset). 24/82 patients of our collective had died, according to our re-evaluation in 2008.
11/82 patients had femoral head necrosis which led to total hip replacement in 8 cases, a hemiarthroplasty in 2 cases, and in 1 case a remaining Girdlestone situation because of a deep infection.
Another five patients also had to undergo a total hip replacement because of a central perforation of the blade in one case, breakout of the blade after another fall in another two cases, and a lateral displacement of the blade in twocases.
Regarding the three individual groups, the following distribution was observed:
In group A, 21/69 patients (30.4%) had died; 9/69 patients developed femoral head necrosis, which led to a total hip replacement in 8 cases and a hemiarthroplasty in 1 case; 3 further patients also had to undergo total hip replacement, 1 patient because of a breakout after a new fall and 2 patients because of a lateral blade displacement.
In group B, 1/8 patients (12.5%) had died; 2/8 patients developed a femoral head necrosis, which led to a hemiarthroplasty in one case and one further patient was left with a Girdlestone situation because of a deep infection after an arthroplasty was attempted; one patient received a total hip replacement because of a breakout of the blade after another fall.
In group C, 2/5 (40%) patients had died at the time of follow-up; one patient required a total hip replacement due to a central blade perforation.
Detailed characteristics are given in Table 3 and Fig. 3.
Discussion
Medial femoral neck fractures have always been problematic. The general medical consensus is to conserve the femoral head, in the case of [1] impacted and non-displaced medial femoral neck fractures (Garden I and II) as well as [2] displaced medial femoral neck fractures in younger patients. Non-displaced fractures of the elderly can be treated in individual cases with head-preserving therapy whereas an intramedullary treatment for older patients with displaced fractures is not recommended by some authors [27,28,29]. It is recommended by some authors that an endoprosthetic restoration should, not only be sought at some stage for fractures of the femoral neck of a higher degree, but that this should actually occur right from the start.
As early as 2002, McKinley et al. were able to show that patients with primary endoprosthetic treatment had a better outcome than patients who had undergone joint conserving surgery and subsequently received endoprosthetic replacement [30]. Osteosynthesis is not recommended and especially if the patient is already suffering from severe osteoarthritis. After an endoprosthetic restoration, the patient can be fully loaded again after a brief time and can also be fully mobilised. This makes it easier to prevent subsequent complications such as pneumonia or a similar condition.
However, there are also borderline cases in which a comprehensive intervention with prolonged anaesthetic guidance and increased blood loss must be critically evaluated. This raises the question of whether the use of an intramedullary force carrier such as the gliding nail (GN) can create a better perioperative outcome for the patient. The gliding nail (GN) is an implant that can be inserted quickly and with minimum invasion. The operation has a significantly lower blood loss than an endoprosthetic replacement operation and even after this the patient can again fully load. It must also be taken into account that there are frail patients who have already undergone nursing case before their injury or who have only been able to lie in bed. For these patients, it may be favourable to have a smaller and rapid intervention for the perioperative outcome, rather than an extensive endoprosthetic treatment, hence the patients can be safely positioned and cared for again.
Generally, the use of an intramedullary implant, firm fracture impaction, tilting of the femoral head, and implant breakouts have led to a high rate of implant failure rates of up to 30% [31]. Furthermore, 10–15% of cases develop femoral head necrosis or non-union, caused by the initial damage to the vascularisation, perhaps also because the instability of the osteosynthesis [32, 33]. Those cases can be recognised by the often very strong impaction with protruding screw heads and corresponding high bone resorption in the fracture zone.
Our results show that the majority of fractures that are treated with a GN, heal without complications (see Figs. 4a, b, 5a–d). None of the cases has a pseudarthrosis or severe impaction with neck shortening occurred (i.e. loss of offset). The overall rate of the secondary prosthesis was 15/82 in total (18.29%). But, prosthesis implantations after another fall were also counted (2 patients), but this should not be considered as implant failure.
Dividing information into the three collectives has shown that 12/69 of patients in group A, 2/8 of patients in group B, and 1/5 patients (20.0%) in group C required hip replacements.
However, if we take a closer look at the corresponding prosthetic indications, it can be seen that there is a significantly lower number of femoral head necrosis cases in our collective than in the comparative literature [31,32,33,34]. The main indication for hip replacement in group A was femoral head necrosis in nine cases. Three further patients also had to undergo total hip replacement, one patient because of a breakout after a new fall and two patients because of a lateral blade displacement. Our results show an overall rate of femoral head necrosis of 9/69 in group A (13.04%) and 1/8 in group B (12.5%). Lu-Yao et al. describe a non-union rate of 33% and a rate of femoral head necrosis of 16% in the results of their meta-analysis of displaced femoral neck fractures [34].
In group C, 1/5 patients required a total hip replacement due to a central blade perforation. Similarly, the other authors also note 10–20% of avascular femoral head necrosis cases after displaced femoral neck fractures [32, 33]. Some authors even note < 30% of femoral head necrosis cases [31]. Regarding our collective, we also recorded avascular necrosis—the incidence is lower than the risk described by the other authors; but the small collective of group B must be taken into account. This also reflects the consensus to treat higher grade femoral neck fractures with a prosthetic device.
To prevent femoral head necrosis, a fast operation within the “6-h window”, as an emergency operation in younger patients with a displaced fracture, is recommended; if it is not possible to treat a patient within 6 h or at least within 24 h, an endoprosthetic treatment is also recommended [6,7,8, 35,36,37].
An operative treatment and an urgent operation according to the above criteria will not only improve the local outcome of the fracture but will also lower the in-hospital mortality of the patients and the postoperative mortality, in general, as the other authors have shown in their respective studies [15, 38].
Our collective showed a total complication rate of 12/69 (17.4%) for fracture healing and fracture stabilisation in group A. Group B showed a total complication rate of 3/8 (37.5%). The size of the collective, especially regarding group B, is also a limiting factor here. Eschler et al. reported a “Cut-Out” (i.e. femoro-acetabular penetration) in 8 patients (32%) treated with a DHS and 4 patients (15%) treated with a Targon®-FN in a study of 52 patients [39]. In our collective, none of the patients showed signs of a typical “Cut-Out.”
Using a very stable implant, such as the GN, which allows an impaction of the fracture while eliminating rotational movements, which minimises the risk of breakout, results in a lower rate of complication in the femoral head, thus conserving treatment of medial femoral neck fractures. The danger of femoral head necrosis is not only dependent on the age of the patient and the resulting remaining vascularity and bone quality, but also is also especially dependent on trauma-induced damage. In our collective, group A had an incidence of femoral head necrosis of 9/69, compared to 1/8 in group B. Sometimes it is stated that medial femoral neck fractures are nothing but a sign of physical deterioration. Since our data show that patients over 60 years of age also develop femoral head necrosis in cases of a simple, non-displaced fracture, there must be various influencing factors. The solid, rotation-free fracture retention of the GN enables a revitalisation of the femoral head, and even in patients with vascularisation damage caused by the fracture.
Generally, a low rate of complication and early fully load-bearing treatment should be the goal. Moreover, older patients often have a significant number of additional risk factors, often due to pre-existing comorbidities, all of which affect outcome and postoperative mortality [40]. Medial femoral neck fractures should only be treated with an osteosynthesis in the case of fracture impaction, non-displacement, and younger patients. In older patients with a higher grade of displacement, in general, treatment with osteosynthesis is not recommended; the other authors agree [27]. However, the advantages and disadvantages for the patient should be critically considered. Thus, the life situation before the fracture event, as well as the individual state of health and the associated surgical risk, must be taken into account. Therefore, every decision should take into account not only the risk of the operation but also the risk of postoperative complications and, as aforementioned, the risk of the care of these.
Strengths and Limitations
One strength of this study is the detailed clinical documentation and data collection as well as the large size of the patient collective. However, a small number of patients in the individual groups can be considered a weakness. Other weaknesses of the study are a missing prospective collective for comparison, the single-centre study, and the retrospective design.
Conclusion
The treatment of displaced medial femoral neck fractures in older patients is generally the domain of treatment with endoprosthesis. However, there are also borderline indications where rapid, minimally invasive surgery is required to stabilise the fracture.
The use of a very stable implant, such as the GN, which enables impaction of the fracture with the elimination of rotational movements and minimises the risk of an outbreak, leads to a lower complication rate in the femoral head and thus to gentle treatment of medial femoral neck fractures. The GN is a safe, easy-to-use implant with a low perioperative lethality that provides a major benefit to patients in the treatment of femoral neck fractures. However, its application must be critically considered and the individual risk and benefit of each patient must be taken into account.
References
Jordan, K. M., & Cooper, C. (2002). Epidemiology of osteoporosis. Best Practice and Research Clinical Rheumatology, 16(5), 795–806.
Smektala, R., Grams, A., Pientka, L., & Raestrup, U. S. (2008). Guidelines or state civil codes in the management of femoral neck fracture? An analysis of the reality of care provision in North Rhine-Westphalia. DeutschesÄrzteblatt International, 105(16), 295–302.
Frerichmann, U., Raschke, M. J., Stockle, U., Wohrmann, S., & Lohmann, R. (2007). Proximal femoral fractures in the elderly. Data from health insurance providers on more than 23 million insured persons—part 2. Unfallchirurg., 110(7), 610–616.
Lindahl, H. (2007). Epidemiology of periprosthetic femur fracture around a total hip arthroplasty. Injury, 38(6), 651–654.
Lohmann, R., Frerichmann, U., Stockle, U., Riegel, T., & Raschke, M. J. (2007). Proximal femoral fractures in the elderly. Analysis of data from health insurance providers on more than 23 million insured persons—part 1. Unfallchirurg., 110(7), 603–609.
Liem, I. S., Kammerlander, C., Raas, C., Gosch, M., & Blauth, M. (2013). Is there a difference in timing and cause of death after fractures in the elderly? Clinical Orthopaedics and Related Research, 471(9), 2846–2851.
Siegmeth, A. W., Gurusamy, K., & Parker, M. J. (2005). Delay to surgery prolongs hospital stay in patients with fractures of the proximal femur. Journal of Bone and Joint Surgery. British Volume, 87(8), 1123–1126.
Rosso, F., Dettoni, F., Bonasia, D. E., Olivero, F., Mattei, L., Bruzzone, M., et al. (2016). Prognostic factors for mortality after hip fracture: Operation within 48 hours is mandatory. Injury, 47(Suppl 4), S91–S97.
Andruszkow, H., Scharff, B., Zapf, A., Klein, M., Lechler, P., Hildebrand, F., et al. (2013). Influence of comorbidities and delay in surgical treatment on mortality following femoral neck fracture. Zeitschrift fur Orthopadie und Unfallchirurgie, 151(4), 338–342.
Blomfeldt, R., Tornkvist, H., Ponzer, S., Soderqvist, A., & Tidermark, J. (2005). Internal fixation versus hemiarthroplasty for displaced fractures of the femoral neck in elderly patients with severe cognitive impairment. Journal of Bone and Joint Surgery. British Volume, 87(4), 523–529.
Keating, J. F., Grant, A., Masson, M., Scott, N. W., & Forbes, J. F. (2006). Randomized comparison of reduction and fixation, bipolar hemiarthroplasty, and total hip arthroplasty. Treatment of displaced intracapsular hip fractures in healthy older patients. Journal of Bone and Joint Surgery American, 88(2), 249–260.
Ludolph, E., & Hierholzer, G. (1979). Fractures of the femoral neck in old aged people (author’s transl). Zentralblatt fur Chirurgie, 104(23), 1565–1572.
Xu, D. F., Bi, F. G., Ma, C. Y., Wen, Z. F., & Cai, X. Z. (2017). A systematic review of undisplaced femoral neck fracture treatments for patients over 65 years of age, with a focus on union rates and avascular necrosis. Journal of Orthopaedic Surgery and Research, 12(1), 28.
Broderick, J. M., Bruce-Brand, R., Stanley, E., & Mulhall, K. J. (2013). Osteoporotic hip fractures: The burden of fixation failure. Scientific World Journal, 2013, 515197.
Chlebeck, J. D., Birch, C. E., Blankstein, M., Kristiansen, T., Bartlett, C. S., & Schottel, P. C. (2019). Nonoperative geriatric hip fracture treatment is associated with increased mortality: A matched cohort study. Journal of Orthopaedic Trauma, 33(7), 346–350.
Ateschrang, A., & Dittel, K. K. (2007). Osteosynthetically-treated intracapsular femoral neck fractures. Zentralblatt fur Chirurgie, 132(1), 44–48.
Bonnaire, F., Kuner, E. H., & Lorz, W. (1995). Femoral neck fractures in adults: Joint sparing operations. II. The significance of surgical timing and implant for development of aseptic femur head necrosis. Unfallchirurg, 98(5), 259–264.
Bertelink, B. P., Stapert, J. W., & Vierhout, P. A. (1993). The dynamic hip screw in medial fractures of the femoral neck: Results in 51 patients. NederlandsTijdschriftvoorGeneeskunde, 137(2), 81–85.
Valverde, J. A., Alonso, M. G., Porro, J. G., Rueda, D., Larrauri, P. M., & Soler, J. J. (2003). Use of the gamma nail in the treatment of fractures of the proximal femur. 1998. Journal of Orthopaedic Trauma, 17(8 Suppl), S51–S56.
Bojan, A. J., Beimel, C., Speitling, A., Taglang, G., Ekholm, C., & Jonsson, A. (2010). 3066 consecutive Gamma nails. 12 years experience at a single centre. BMC Musculoskeletal Disorders, 11, 133.
Friedl, W., & Clausen, J. (2001). Experimental examination for optimized stabilisation of trochanteric femur fractures, intra- or extramedullary implant localisation and influence of femur neck component profile on cut-out risk. Chirurg, 72(11), 1344–1352.
Friedl, W. (1996). The gliding nail. A new implant for complication-free primary load-bearing management of per- and subtrochanteric femoral fractures. LangenbecksArchiv fur Chirurgie. Supplement, 113, 970–973.
Friedl, W., Hilsenbeck, F., & Stürzenhofecker, P. (2005). Joint preserving treatment of medial femoral neck fractures with the small gliding nail {Article in German}. CHAZ, 6(9), 375–380.
Garden, R. S. (1961). Low angle fixation in fractures of the femoral neck. Journal of Bone and Joint Surgery. British Volume, 43, 647–663.
Garden, R. S. (1964). Stability and union in subcapital fractures of the femur. Journal of Bone and Joint Surgery. British Volume, 46, 630–647.
Pauwels, F. (1935). The femoral neck fracture. A mechanical problem {Article in German}. ZeitschriftfürorthopädischeChirurgie, 63(3), 1–138.
Mir, H. R., Edwards, P., Sanders, R., & Haidukewych, G. (2011). Results of cephallomedullary nail fixation for displaced intracapsular femoral neck fractures. Journal of Orthopaedic Trauma, 25(12), 714–720.
Park, B. J., Cho, H. M., & Min, W. B. (2015). Surgical treatment of undisplaced femur neck fractures in dementia patients using proximal femoral nail antirotation. Hip Pelvis, 27(3), 164–172.
Heetveld, M. J., Rogmark, C., Frihagen, F., & Keating, J. (2009). Internal fixation versus arthroplasty for displaced femoral neck fractures: What is the evidence? Journal of Orthopaedic Trauma, 23(6), 395–402.
McKinley, J. C., & Robinson, C. M. (2002). Treatment of displaced intracapsular hip fractures with total hip arthroplasty: Comparison of primary arthroplasty with early salvage arthroplasty after failed internal fixation. Journal of Bone and Joint Surgery. American Volume, 84(11), 2010–2015.
Gurusamy, K., Parker, M. J., & Rowlands, T. K. (2005). The complications of displaced intracapsular fractures of the hip: The effect of screw positioning and angulation on fracture healing. Journal of Bone and Joint Surgery. British Volume, 87(5), 632–634.
Manninger, J., Kazar, G., Fekete, G., Nagy, E., Zolczer, L., & Frenyo, S. (1985). Avoidance of avascular necrosis of the femoral head, following fractures of the femoral neck, by early reduction and internal fixation. Injury, 16(7), 437–448.
Schmidt, A. H., & Swiontkowski, M. F. (2002). Femoral neck fractures. Orthopedic Clinics of North America, 33(1), 97–111. ((viii)).
Lu-Yao, G. L., Keller, R. B., Littenberg, B., & Wennberg, J. E. (1994). Outcomes after displaced fractures of the femoral neck. A meta-analysis of one hundred and six published reports. Journal of Bone and Joint Surgery American, 76(1), 15–25.
Manninger, J., Kazar, G., Fekete, G., Fekete, K., Frenyo, S., Gyarfas, F., et al. (1989). Significance of urgent (within 6h) internal fixation in the management of fractures of the neck of the femur. Injury, 20(2), 101–105.
Parker, M. J., & Blundell, C. (1998). Choice of implant for internal fixation of femoral neck fractures. Meta-analysis of 25 randomised trials including 4,925 patients. ActaOrthopaedicaScandinavica, 69(2), 138–143.
Szita, J., Cserhati, P., Bosch, U., Manninger, J., Bodzay, T., & Fekete, K. (2002). Intracapsular femoral neck fractures: The importance of early reduction and stable osteosynthesis. Injury, 33(Suppl 3), C41–C46.
Uzoigwe, C. E., Burnand, H. G., Cheesman, C. L., Aghedo, D. O., Faizi, M., & Middleton, R. G. (2013). Early and ultra-early surgery in hip fracture patients improves survival. Injury, 44(6), 726–729.
Eschler, A., Brandt, S., Gierer, P., Mittlmeier, T., & Gradl, G. (2014). Angular stable multiple screw fixation (Targon FN) versus standard SHS for the fixation of femoral neck fractures. Injury, 45(Suppl 1), S76-80.
Hu, F., Jiang, C., Shen, J., Tang, P., & Wang, Y. (2012). Preoperative predictors for mortality following hip fracture surgery: A systematic review and meta-analysis. Injury, 43(6), 676–685.
Acknowledgements
We acknowledge Raben Heller (Heidelberg Trauma Research Group, University of Heidelberg) for statistical advisory.
Funding
Manuscript creation did not involve any funding sources.
Author information
Authors and Affiliations
Contributions
All the authors, TFR, WF and AM, declare that they have made a substantial contribution to the collection of data, the evaluation and the preparation of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Dr. med. Tim Friedrich Raven and Prof. Dr. Arash Moghaddam declare that they have no conflict of interest. The presentation of the topic is independent and the presentation of the contents product-neutral. One of the authors, Prof. Dr. med. Dr. h.c. mult. Wilhelm Friedl, is the inventor of the gliding nail and works as a development consultant for Intercus GmbH.
Ethics approval
This study was approved by the Ethics Committee of the medical faculty Heidelberg. Hence, the study was approved by the review board and conducted according to the guidelines of the review board and within the bounds of good clinical practice according to the ethical principles that have their origin in the Declaration of Helsinki in its current form.
Consent to participate
All the patients were asked for permission for data evaluation and they gave their approval. All data were archived anonymously.
Consent for publication
All the patients were asked for permission for data evaluation and they gave their approval. All data were archived anonymously.
Availability of data and material
All data were archived anonymously.
Code availability
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Wilhelm Friedl: Inventor of the Gliding Nail.
Rights and permissions
About this article
Cite this article
Raven, T.F., Friedl, W. & Moghaddam, A. Treatment of Traumatic Femoral Neck Fractures with an Intramedullary Nail in Osteoporotic Bones. JOIO 55, 621–628 (2021). https://doi.org/10.1007/s43465-020-00292-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-020-00292-3