Abstract
Background
Stress fracture of the femoral neck (SFFN) is one of the severe complications of military training. Displaced SFFN may result in avascular necrosis of the femoral head (AVNFH). The purpose of this study was to evaluate the results of surgical treatment of the displaced SFFN.
Methods
Forty-two patients with displaced SFFN requiring internal fixation were treated with compression hip screw (17 cases) or multiple cancellous screws (25 cases). Forty-two patients were followed for an average of 5.6 years after operation. At the follow-up evaluation, routine radiographs were used to evaluate the fracture alignment and healing, and bone scan was used for fractures that were suspected of AVNFH. The functional assessments described by Arnold et al. were used to evaluate the functional results of surgical treatment.
Results
Seven (28%) of the 25 patients treated with multiple cancellous screws developed AVNFH during the period of follow-up. Of these seven patients, five were treated with prosthetic replacement and two treated with core decompression and bone graft. Three (17.6%) of the 17 patients treated with compression hip screw had AVNFH, and they were all treated with prosthetic replacement. The mean duration between fracture and surgery was significantly longer in patients with AVNFH (5.9 days) than in patients without AVNFH (1.9 days)(P<0.05). Five (71.4%) of the seven patients who presented a varus alignment of the femoral neck developed AVNFH later, and only five (14.3%) of the 35 patients who presented with anatomic or valgus alignment of the femoral neck developed AVNFH during the period of follow-up. Of the 42 patients, 30 (71.4%) had good functional results, four (9.5%) had acceptable and eight (19%) had poor results at the end of evaluation.
Conclusion
Delayed treatment and postoperative varus alignment were major factors contributing to AVNFH in our series. Early treatment and anatomical fixation of displaced SFFN are essential for diminishing the risk of AVNFH development.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A stress or fatigue fracture in a bone may occur in an otherwise healthy young individual because of repetitive overloading during training or exercise [8]. Stress fracture of the femoral neck (SFFN) is a rare but severe injury occurring most frequently in long-distance runners [5, 6, 13], professional athletes [12], ballet dancers [6], and military recruits [11, 16, 17, 18, 19]. Complications following SFFN, including delayed union, nonunion, and avascular necrosis of the femoral head (AVNFH), occurred in 10% to 40% of SFFN patients [9, 16, 18, 21]. Variables such as reduction alignment, time between fracture occurrence and treatment, and type of implant used can affect the probability of post-SFFN complications. However, the impact of such variables in the treatment of SFFN in military recruits remains untested. We examined the effects of the type of implants used and the morbidity and SFFN-related complications in young military recruits.
Patients and methods
Between June 1989 and July 1999, 66 patients suffering 77 incidences of SFFN were diagnosed and treated in our hospital. All were young male military trainees with a mean age at time of injury of 20.4 years (range 18–23 years). Fifty-one demonstrated a displaced fracture. SFFN was diagnosed because fractures occurred while running, marching, or jumping during the course of the patients' military training. No patient reported that a traffic accident or fall contributed to his fracture. During the course of the study, five patients left the country, and contact was lost with four others; 42 SFFN-qualified participants were included in the final evaluation.
The mean follow-up period was 5.6 years (range 2–10 years). During their period of military service, military recruits engage in rigorous physical training, including daily 5-km endurance runs, twice monthly 500-meter obstacle races, and monthly forced marches of up to 20 km while carrying packs weighing up to 15 kg. Fractures involved 31 right and 11 left hips, and all were treated with surgical reduction and internal fixation. All SFFN were completely displaced, and all patients received emergency surgery immediately after their hospital admission.
The patient (under spinal anesthesia) was placed in a supine position on a fracture table, and a closed reduction of the fracture under traction and internal rotation of the lower limb was performed. Post-reduction alignment was checked using a C arm fluoroscope. Acceptable alignment was defined as either an anatomical or mild valgus position. Implants used included compression hip screws (CHS) in 17 cases and multiple 6.5-mm cancellous screws (MCS) in 22 cases. For three patients, 5 or more days had passed between time of injury and surgery. These patients, under general anesthesia, were placed in a prone position on a fracture table; open reduction internal fixation with MCS and a quadratus femoris muscle pedicle bone graft were performed.
The patients received check-ups every 2 weeks during the first postoperative month and then once every month until fracture union. Physicians monitored the fracture site using standard radiographs (anteroposterior pelvis and true lateral hip) on the second day, first month, third month, and sixth month after surgery. Afterward, the two radiographic analyses were performed annually. Technetium-99m- methylenediphosphonate scintimetry was conducted when patients were suspected of AVNFH. The criteria for this study included (1) the patients suffered from persistent hip pain but the radiographs did not show the obvious signs of AVNFH such as sclerosis, crescent sign or segmental collapse and (2) the postoperative period was more than 8 months according to the research of Stromqvist et al. [20]. We calculated the femoral neck-shaft angle using radiographs and defined a valgus reduction as anything greater than and a varus reduction as anything less than a 135° standard anatomical reduction angle. We conducted a functional assessment of patient hips using an evaluation form developed by Arnold et al. [1]. Results were graded as "good" for no pain, full mobility, and full return to pre-injury walking ability and daily activities; "acceptable" for occasional pain, mildly impaired mobility and walking ability, and mild limitation of daily activity, with no indication for additional surgical intervention; and "poor" for significant pain, restricted range of mobility, walking ability, and daily activity, with additional surgical intervention indicated.
We performed an unpaired Student's t-test using the SPSS/PC computer program to determine whether statistically significant differences could be found between patients with and without post-operative AVNFH complications in terms of the following variables: duration of symptoms, duration of military service, and duration between time of fracture and time of operation. Statistical significance was set at P<0.05.
Results
Running was the primary cause of injury (73.8% of cases). The mean duration of military training prior to the occurrence of symptoms was 3.5 months (range 1–7 months), mean duration between hip pain onset and fracture was 15.8 days (range 4–45 days), and mean time between fracture and surgery was 2.9 days (range 1–10 days). During the period immediately following surgery to treat SFFN, no major complications or cases of mortality were reported among the 42 patients. The one case of superficial wound infection was successfully treated after local debridement and antibiotic administration. No case showed implants failure or screw migration. Of the 42 fractures, 36 (85.7%) united successfully and six (14.3%) showed delayed union.
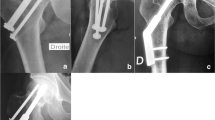
Over an average of 5.6 years (range 2–10 years) of follow-up examinations, 32 (76%) of the survey patients healed well (30 "good" and two "acceptable") and did not experience further complications (Table 1 and Fig. 1A–D). The mean time lag between fracture and surgery was 1.9 days (range 1–4 days). Of the 32 fractures, 30 (93.7%) demonstrated anatomical or 5–10 deg valgus reduction alignment. Varus alignment was evident on two patients' late follow-up radiographs due to delayed unions; their fractures eventually united within 1 year (Table 1, cases 13 and 24). Implants used in the treatment of these 32 fractures included 18 multiple cancellous screws and 14 compression hip screws.
Complete displaced stress fracture of the femoral neck with a fragment on the medial calcar region (black arrow) was noted in a recruit following a 3-month running training. B Postoperative anteroposterial view showed an acceptable alignment with three cancellous screws fixation. A bony defect over compression side and a reduced calcar fragment (black arrow) were noted. C Postoperative lateral view showed a good reduction and screws fixation. D A radiograph taken at 3 months follow-up showed the fracture site united well. No complication of avascular necrosis of the femoral neck was found for 3 years follow-up
AVNFH developed in ten (23.8%) of the survey patients during a period of between 6 and 28 months (mean 14.6 months) following the initial surgery (Table 2). For these ten patients, the mean duration between fracture and surgery was 5.9 days (range 4–10 days). This duration was significantly longer (P<0.05) than that for the group of 32 whose fractures united well and without AVNFH. No significant differences were identified between the two groups in terms of duration of symptoms and military service.
The final alignment positions of fractures with AVNFH included five varus, three valgus, and two anatomical. Of the ten AVNFH fractures, seven received multiple cancellous screws, and three received compression hip screws. AVNFH developed by the final check-up in all three fractures treated by open reduction and muscle pedicle bone grafts.
Segmental collapse of the femoral head occurred in eight of the ten AVNFH cases; two had total hip replacement and six had bipolar hemiarthroplasty. We noted a crescent sign on radiographs from the two patients who showed no obvious segmental collapse (Table 2, cases 1 and 7). These patients' screws were removed, and they received core decompression and an autogenous cancellous bone graft to the femoral head. They responded well to this treatment, and hip joint replacement was not recommended. However, one of the two patients developed hip joint osteoarthritis during the eighth year of follow-up examinations (Table 2, case 1).
In follow-up radiographs of the 42 fractures, three of 22 (13.6%) fractures repaired with CHS (Fig. 2A–E) and three of 17 (17.6%) fractures repaired with MCS showed progressive loss of reduction and varus deformity (Table 3). Thirty-five (83%) of the 42 SFFN occurrences appeared to be reduced in an anatomical or valgus alignment. Seven (17%) of the 42 displaced SFFN patients showed varus alignment on follow-up radiographs; five (71.4%) were diagnosed with AVNFH on the final follow-up.
Complete displaced stress fracture of the femoral neck noted in a recruit following a 2-month running training with a 5-day delayed arrival to hospital. B Postoperative anteroposterial view showed an acceptable alignment but a bony defect over medial compression side. C A radiograph taken at 6 months after operation showed the fracture site united well but presented a varus deformity 5 deg. D One year after operation, avascular necrosis of the femoral head with collapse and screws protruding were found. E Bipolar hemiarthroplasty was performed
At the end of the follow-up period, functional results were "good" in 30 (71.4%) of the 42 patients, "acceptable" in four (9.5%), and "poor" in eight (19%).
Discussion
Although stress fracture of the femoral neck (SFFN) in young military recruits is not a common injury, the incidence of displacement is high once it occurs. A wide range of SFFN incidence (0.36 to 11%) has previously been reported [3, 5, 8, 9]. Fullerton and Snowdy [9] reported that six (12.3%) of 49 patients with SFFN experienced complete displacement. Conversely, we found that 51 (66.2%) of the 77 SFFN were displaced fractures. This high incidence may be attributed to muscle strain caused by an undiagnosed tension side stress fracture [13] or to the continuation of rigorous training despite SFFN. Because of the potential for severe complications that may result from a displaced femoral neck fracture, a physician should take special note when examining and treating patients who sustained injury during strenuous activities, particularly mandatory exercises demanded of military recruits.
The injury mechanism underlying SFFN remains controversial. From a biomechanical standpoint, muscle fatigue clearly plays an important role in the onset of SFFN [8]. The gluteal medius muscle fatigue that follows repetitive exercise can reduce the muscle's shock absorbing capacity and increase stress over the superior aspect of the femoral neck [8]. The result is increased risk for stress fracture of the femoral neck. Overloading of the bone, repetitive exercise, and muscle fatigue are the most important factors contributing to SFFN genesis [8].
After radiographs are analyzed, SFFN may be categorized as either displaced or non-displaced, which may present as a tension or compression type. In 1965, Devas [7] classified SFFN into transverse and compression types. In 1966, Blickenstaff and Morris [3] described three types of SFFN: Type I, an endosteal or periosteal callus without an overt fracture line; Type II, a non-displaced fracture line in the calcar region or across the neck; and Type III, a displaced fracture. Fullerton and Snowdy [9] categorized SFFN as tension, compression, and displaced. The tension type occurred in the superolateral region of the femoral neck and carried the risk of fracture displacement; the compression type occurred on the inferomedial aspect of the femoral neck and was typically stable; the displaced type likely resulted from a non-displaced tension fracture under persistent stress loading and typically had a high complication rate [3, 9].
The prognosis following femoral neck fractures is poor in young adults; the incidence of AVNFH (20 to 86%) is particularly high in this group [15, 17]. The cause of femoral neck fracture in young adults is nearly always related to a high kinetic energy trauma such as a high-velocity vehicular accident or a fall from some height [17]. Although the severity of trauma in the patients with SFFN was reported to be low, the AVNFH incidence in SFFN patients remained high. In two previous studies, five of 12 (42%) young adults [21] and three of ten (30%) young adults [13] with displaced SFFN developed AVNFH. We found that 23.8% of patients developed AVNFH after SFFN displacement within the mean 5.6-year follow-up time.
The likelihood of developing AVNFH following SFFN displacement may be related to fracture displacement grade, type of implant used, time elapsed between fracture and operation, and reduction alignment. The cause of AVNFH may be rooted in the displacement with comminution of the posterior cortex of the femoral neck [21]. Circulation to the femoral head within the lateral epiphyseal (intraosseous) and posterior superior retinecular vessels (extraosseous) may be disrupted. The process of nailing the femoral neck may induce an additional trauma; rotation of the capital fragment during the nailing process has been observed under magnification [10, 17]. Inserting a large nail or lag screw into the dense bone of a young patient can be difficult; if femoral head rotation or heating occur, the head can be damaged. Multiple pins or screws are often recommended over central fixation devices because multiple screws provide peripheral fixation, which more effectively prevents rotation and allows impaction [10, 14, 15, 17]. However, from a biomechanical point of view, the sliding hip screw has been recommended instead of the multiple cancellous screws for treating basicervical femoral neck fractures because the sliding hip screw has a significantly higher axial load to failure ratio [2]. Using cyclic load tests, Clark et al. [4] demonstrated that levels of CHS and MCS fixation were essentially equal and that the quality of a patient's bone was the single most important factor determining bone implant stability. In our study, fractures treated either by CHS or MCS reached a rigid fixation and healed well except for the six fractures with a delayed union.
Johansson et al. [13] also pointed out that delay in diagnosis and management of displaced SFFN may result in a significantly higher incidence of AVNFH. In their series, three of ten patients with displaced SFFN who had delayed treatment by 4 to 52 weeks developed AVNFH following internal fixation. Manninger et al. [14, 15] found that patients with femoral neck fractures who had surgery within 6 h of the injury had an AVNFH incidence of 10.5 to 20%. However, when surgery was delayed for more than 24 h, the incidence of AVNFH increased to 31.8 to 34%. They suggested that early reduction might relieve blood vessel occlusion in the femoral neck caused by the displaced fracture [14, 15]. In our study, the mean time between fracture occurrence and surgery for patients with AVNFH was 5.9 days. This time period was significantly longer than the period of 1.9 days for those who did not develop AVNFH. Our research supports the hypothesis that delays in operating expediency increase AVNFH incidence.
Malreduction or varus alignment also predisposes patients to the development of AVNFH. In our present series, five (71%) of the seven varus alignment cases showed AVNFH in follow-up radiographs. Healing of a fracture in the varus position may facilitate femoral head collapse [10]. Manninger et al. [15] evaluated 323 fractures; 26 (100%) of 26 varus reductions developed AVNFH with segmental collapse.
Our study confirms that successful treatment of displaced SFFN includes effective reduction, early surgical intervention, and rigid fixation. The procedure to reduce the fracture may be most effective if the femoral head is placed in an anatomical or slight valgus position to allow impaction. A poor reduction, such as occurs with the varus position, may elicit delayed union and development of AVNFH.
References
Arnold WD, Lyden JP, Minkoff J (1974) Treatment of intracapsular fractures of the femoral neck. J Bone Joint Surg [Am] 56:254–262
Blair B, Koval KJ, Kummer F, Zuckerman JD (1994) Basicervical fractures of the proximal femur. A biomechanical study of 3 internal fixation techniques. Clin Orthop 306:256–263
Blickenstaff LD, Morris JM (1996) Fatigue fracture of the femoral neck. J Bone Joint Surg [Am] 48:1031–1047
Clark DI, Crofts CE, Saleh M (1990) Femoral neck fracture fixation. Comparison of a sliding screw with lag screws. J Bone Joint Surg [Br] 72:797–800
Daffner RH (1978) Stress fractures: current concepts. Skeletal Radiology 2:221–229
Daffner RH, Pavlov H (1992) Stress fractures: current concepts. AJR 159:245–252
Devas MB (1965) Stress fractures of the femoral neck. J Bone Joint Surg [Br] 47:728–738
Egol KA, Koval KJ, Kummer F, Frankel VH (1998) Stress fractures of the femoral neck. Clin Orthop 348:72–78
Fullerton LR, Snowdy HA (1988) Femoral neck stress fractures. Am J Sports Med 16:365–377
Garden RS (1971) Malreduction and avascular necrosis in subcapital fractures of the femur. J Bone Joint Surg [Br] 53:183–197
Greaney RB, Gerber FH, Laughlin RL (1983) Distribution and natural history of stress fractures in U.S. marine recruits. Radiology146:339–346
Hajek MR, Noble HB (1982) Stress fractures of the femoral neck in joggers. Case reports and review of the literature. Am J Sports Med 10:112–116
Johansson C, Ekenman I, Tornkvist H, Eriksson E (1990) Stress fractures of the femoral neck in athletes: the consequence of a delay in diagnosis. Am J Sports Med 18:524–528
Manninger J, Kazar GY, Fekete GY, Nagy E, Zolczer L, Frenyo S (1985) Avoidance of avascular necrosis of the femoral head following fractures of the femoral neck, by early reduction and internal fixation. Injury 16:437–448
Manninger J, Kazar G, Fekete G, Fekete K, Frenyo S, Gyarfas F, Salacz T, Varga A (1989) Significance of urgent (within 6 h) internal fixation in the management of fractures of the neck of the femur. Injury 20:101–105
Mendez AA, Eyster RL (1992) Displaced nonunion stress fracture of the femoral neck treated with internal fixation and bone graft. A case report and review of the literature. Am J Sports Med 20:230–233
Protzman RR, Burkhalter WE (1976) Femoral-neck fractures in young adults. J Bone Joint Surg [Am] 58:689–695
Sjolin SU, Eriksen C (1989) Stress fracture of the femoral neck in military recruits. Injury 20:304–305
Stoneham MA, Bchir MB, Morgan NV (1991) Stress fractures of the hip in Royal Marine recruits under training: a retrospective analysis. Br J Sports Med 25:145–148
Stromqvist B, Brismar J, Hansson LI, Palmer J (1984) Technetium-99m-methylenediphosphonate scintimetry after femoral neck fracture. A three-year follow-up study. Clin Orthop 182:177–189
Visuri T, Vara A, Meurman K (1988) Displaced stress fractures of the femoral neck in young male adults: a report of twelve operative cases. J Trauma 28:1562–1569
Acknowledgements
No author or related institution has received any financial benefit from research in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, CH., Huang, GS., Chao, KH. et al. Surgical treatment of displaced stress fractures of the femoral neck in military recruits: a report of 42 cases. Arch Orthop Trauma Surg 123, 527–533 (2003). https://doi.org/10.1007/s00402-003-0579-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-003-0579-8