Abstract
Pediatric glioblastoma (pedGBM) is amongst the most common malignant brain tumors of childhood and carries a dismal prognosis. In contrast to adult GBM, few molecular prognostic markers for the pediatric counterpart have been established. We, therefore, investigated the prognostic significance of genomic and epigenetic alterations through molecular analysis of 202 pedGBM (1–18 years) with comprehensive clinical annotation. Routinely prepared formalin-fixed paraffin-embedded tumor samples were assessed for genome-wide DNA methylation profiles, with known candidate genes screened for alterations via direct sequencing or FISH. Unexpectedly, a subset of histologically diagnosed GBM (n = 40, 20 %) displayed methylation profiles similar to those of either low-grade gliomas or pleomorphic xanthoastrocytomas (PXA). These tumors showed a markedly better prognosis, with molecularly PXA-like tumors frequently harboring BRAF V600E mutations and 9p21 (CDKN2A) homozygous deletion. The remaining 162 tumors with pedGBM molecular signatures comprised four subgroups: H3.3 G34-mutant (15 %), H3.3/H3.1 K27-mutant (43 %), IDH1-mutant (6 %), and H3/IDH wild-type (wt) GBM (36 %). These subgroups were associated with specific cytogenetic aberrations, MGMT methylation patterns and clinical outcomes. Analysis of follow-up data identified a set of biomarkers feasible for use in risk stratification: pedGBM with any oncogene amplification and/or K27M mutation (n = 124) represents a particularly unfavorable group, with 3-year overall survival (OS) of 5 %, whereas tumors without these markers (n = 38) define a more favorable group (3-year OS ~70 %).Combined with the lower grade-like lesions, almost 40 % of pedGBM cases had distinct molecular features associated with a more favorable outcome. This refined prognostication method for pedGBM using a molecular risk algorithm may allow for improved therapeutic choices and better planning of clinical trial stratification for this otherwise devastating disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastoma (GBM) is the most common primary malignant brain tumor and has an extremely dismal prognosis, with fewer than 5 % of patients surviving beyond 5 years after diagnosis [28, 30]. It remains incurable with current treatment strategies, which typically consist of surgical tumor removal followed by radiotherapy in combination with concurrent and maintenance temozolomide (TMZ) [10, 44, 51]. Incidence of GBM increases with age, accounting for about half of all malignant brain tumors in adults, but 10–15 % of pediatric CNS tumors (when also considering DIPG and high-grade glioma NOS) [30]. Although childhood and adult GBM share a related histopathological appearance and comparable clinical outcomes, it is now becoming apparent that these tumors are molecularly distinct entities with differing genomic and epigenomic landscapes [5, 15, 20, 21, 33, 45, 46]. For example, recently identified recurrent somatic mutations in H3F3A (encoding the histone variant H3.3) and H3.1 genes (HIST1H3B and HIST1H3C) are frequent in pediatric GBM (approximately 40 % of tumors) but rare in adults [1, 7, 14, 22, 27, 41, 46, 48, 52, 53]. Conversely, prototypic alterations of adult primary GBM (e.g., EGFR amplification, CDKN2A/B homozygous deletions, PTEN mutations) are very infrequent in childhood [4, 5, 25, 32–34, 36, 37, 39, 45]. In addition, IDH1 and IDH2 mutations, which are found in ~90 % of secondary GBM, are also rare in pediatric tumors [31, 33, 46, 54].
While a multitude of molecular prognostic markers have been proposed for adult GBM (e.g., [50]), prognostic factors for their pediatric counterpart are yet to be precisely elaborated. Studies investigating pediatric GBM (pedGBM) for the prognostic value of mutations, gene expression patterns and copy number aberrations have tended to be inconsistent or contradictory, which may be explained by the relatively small cohort sizes and/or heterogeneity of the applied treatment modalities [4, 8, 11, 13, 16, 25, 26, 34, 36, 42, 47]. Cohort size is of particular importance in light of the extensive biological heterogeneity of these tumors, as highlighted by a recent methylome analysis of a pedGBM series that found distinct subgroups correlating with specific genetic alterations and clinical patterns [46], and by further recent in-depth genomics studies (e.g., [14, 53]). In the current study, we investigated the prognostic significance of genomic and epigenetic events assessed through a comprehensive molecular analysis of 202 pedGBM uniformly treated with surgery and radio-chemotherapy, and identified a robust set of markers that may improve the future clinical stratification of pedGBM patients.
Materials and methods
Patient population
Tissue samples (mostly formalin-fixed paraffin-embedded) were obtained from 202 pediatric patients (age 1–18 years) with a histological diagnosis of “glioblastoma, WHO grade IV” (Table 1). The median age was 12 years/months (95 % CI Y–Z), and the median follow-up was 16 months. At the time of this analysis, 133 patients (66 %) have died. None of these patients had a clinical history of previous gliomas, and most were treated in the Burdenko Neurosurgical Institute (Moscow) between 1998 and 2013. Informed consent was obtained from all patients or parents. According to neuroradiological and intraoperative data, just over half of the tumors was located in the cerebral hemispheres (112, 55 %), with 83 tumors (41 %) in the thalamus/basal ganglia region and seven (3 %) in the pons/brain stem (i.e., diffuse intrinsic pontine gliomas). Patients older than 3 years (n = 187) were treated with surgery (gross total or subtotal tumor resection) followed by radiotherapy (limited field fractionated external beam radiotherapy with a dose 54–59.4 Gy on the tumor bed) and adjuvant chemotherapy with TMZ [10]. Fifteen patients 3 years or younger were treated initially with chemotherapy alone after surgery, on the basis of the Baby POG protocol [12]. Recurrent tumors were treated with polychemotherapy using various regimens. Patients receiving biopsy only were not included in this study, since sufficient material for molecular analysis was a prerequisite. Histological diagnosis was based on the current WHO criteria for GBM—an astrocytic glioma with brisk mitotic activity, microvascular proliferation and/or necrosis [28]. Full details of the cohort are given in Supplementary Table 1.
Molecular analysis
DNA was extracted from tumors and analyzed for genome-wide methylation patterns using the Illumina HumanMethylation450 BeadChip (450k) array as previously described [17, 46]. Processing of DNA methylation data and detection of copy number aberrations were performed with custom approaches described in Sturm et al. [46]. For unsupervised hierarchical clustering we selected the most variably methylated probes across the dataset (according to standard deviation thresholds). Samples were clustered using 1-Pearson correlation coefficient as the distance measure and average linkage (x-axis). Methylation probes were reordered by hierarchical clustering using Euclidean distance and average linkage (y-axis).
To evaluate the methylation status of the MGMT promoter region, we used the MGMT_STP27 logistic regression model [2]. For a small number of cases that did not have sufficient DNA remaining for 450k analysis (n = 12), MGMT promoter methylation was measured using the CpG WIZ™ MS-PCR Kit (Merck Millipore, Germany). In addition, mutational analysis for H3F3A (H3.3), HIST1H3B and HIST1H3C (H3.1), IDH1, and BRAF genes was performed using targeted Sanger sequencing. Primer sequences are available on request. FISH analyses were performed using commercially available probes to human oncogenes EGFR, MYC, MYCN, PDGFRA, CDK4 (all from Abbott), and MET, CDK6, CCND1 and CCND2 (all from Abnova; Supplementary Table 2).
Statistics
The distribution of overall survival (OS) was calculated according to the Kaplan–Meier method. OS was calculated from the date of diagnosis until death of patient from disease or last contact for patients who were still alive. For multivariate analysis, Cox proportional hazards regression models were used. Estimated hazard ratios are provided with 95 % confidence intervals and a p value from the Wald test. Tests with a p value below 0.05 were considered significant.
Results
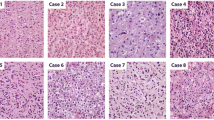
Hierarchical clustering of genome-wide DNA methylation data showed four tumor subsets within the overall patient cohort (Fig. 1). Three of these clusters were defined by K27M or G34R mutations in H3.3 (or rarely H3.1 for K27M) or IDH1 mutations, as expected [46]. None of the IDH1-mutant tumors showed evidence for a precursor lesion, unlike in adults where these mutations typically arise in secondary GBM. The group of samples lacking any of these mutations, however, showed a much greater degree of heterogeneity in their methylome profiles. We, therefore, re-analyzed the H3/IDH wild-type (wt) tumors, to delineate potential additional subgroups. Given the unexpectedly long survival of some of the patients in this cohort and the broad histological spectrum of pediatric gliomas, we additionally included 10 low-grade gliomas (LGGs; namely pilocytic astrocytoma) and 10 pleomorphic xanthoastrocytomas, as well as 12 normal brain samples, for comparison. A notable fraction of tumors with a histological appearance of GBM was found to more closely resemble either the PXAs or LGGs (27/202 with PXA, 13 % and 13/202 with LGG, 6 %; Supplementary Figure 1). A blinded review of 18 of these tumors by an experienced neuropathologist (A. Perry) confirmed their histological appearance as GBM in 15 cases, with only three tumors thought to have features of PXA or LGG upon re-examination (example histologies per group shown in Supplementary Figure 2). Tumors with DNA methylation patterns similar to those of low- or intermediate-grade lesions typically occurred in younger patients (median age 7 vs. 12 years; p = 0.0005, two-tailed t test), including 10 of the 15 patients aged 3 years or younger (a full list of tumor and patient characteristics is given in Supplementary Table 1). The genomic alterations observed in these two subsets also stood out compared with the remainder of the samples. In the molecularly LGG-like group, 4/13 tumors (31 %) harbored a BRAF V600E mutation, and all showed generally balanced genomes in terms of copy number (no focal oncogene amplifications detected, and no loss of the CDKN2A/B locus at 9p21). In the group resembling PXA on the basis of DNA methylation, 13/27 tumors (48 %) displayed a V600E mutation, and 8/27 (30 %) showed homozygous 9p21 deletion, with three carrying both lesions. Both genetic alterations have previously been described as frequent events in PXA [24, 49]. Only four of the remaining 162 samples (2 %) were BRAF V600E mutant. Importantly, tumors displaying a molecularly lower grade signature carried a much more favorable prognosis than those with molecular high-grade features, with 3-year OS of 91 % for the LGG-like samples and 70 % for the PXA-like tumors (Fig. 2).
Unsupervised hierarchical clustering of DNA methylation of the full tumor cohort based on the 1043 most variable methylation probes (SD > 0.30). Black bars positive for given variable; white bars negative for given variable. ‘Amplifications’ the presence of any oncogene amplification as detailed in the text. IDH1, H3 K27 and H3 G34-mutant groups are clearly distinguished, with a more heterogeneous H3/IDH wild-type group on the right-hand side
Survival analysis for various molecular tumor subsets defined by DNA methylation profiling in histologically diagnosed glioblastoma. Tumors with methylation patterns more closely matching low-grade glioma (LGG-like) or pleomorphic xanthoastrocytoma (PXA-like) have a significantly better prognosis. OS overall survival
Our further analyses focused on the 162 tumors with pedGBM molecular signatures based on 450k array profiling. These could be further classified into four distinct methylation subgroups: H3.3 G34-mutant (n = 24, 15 %), H3.3/H3.1 K27-mutant (n = 69, 43 %), IDH1-mutant (n = 10, 6 %), and H3/IDH wt-GBM (n = 59, 36 %). The predicted mutations by DNA methylation subgrouping were confirmed in all cases by direct sequencing of H3F3A, HIST1H3B/HIST1H3C and IDH1, with G34R, K27M (65 H3.3 and four H3.1), and IDH1-mutant tumors exclusively distributed to the corresponding methylation subgroups. Eighty-four pedGBM (52 %) disclosed amplifications of one or more oncogenes, with higher frequency in wt-GBM (71 vs. 46 % in G34, 42 % in K27 and 20 % in IDH1 mutants, respectively) and differences in the types of amplifications observed in different molecular subgroups (Table 1). The most commonly amplified gene was PDGFRA (30/162, 19 %), followed by EGFR (26/162, 16 %) and MYCN (17/162, 10 %). The overall frequency of selected oncogene amplifications is listed in Supplementary Table 3. In addition to focal amplification, deletions of the CDKN2A/B locus and of chromosome arm 10q were also examined. Homozygous 9p21 deletion was found in 25 tumors overall (15 %), and was more frequent in IDH1-mutant pedGBM (6/10, 60 %) but very rare in K27M tumors (1/69, 1 %). Heterozygous loss of 10q was found in 42 % of pedGBM (68/162), and was distributed across all molecular subtypes.
MGMT promoter methylation was found in 40/162 pedGBM (25 %), with a marked variability amongst the molecular subgroups. This epigenetic event was most frequently found in IDH1- (90 %) and G34-mutant (75 %) subtypes and occasionally in wt tumors (19 %), whereas K27 tumors very rarely showed MGMT methylation (3 %).
In line with previous reports, the pedGBM subgroups showed specific patterns of tumor location in the CNS. K27 tumors were almost exclusively located in midline structures (thalamus and brain stem, with only one exception), whereas the other tumor subgroups arose almost exclusively in the cerebral hemispheres, with the exception of a small subset of wt-GBM detected in the basal ganglia or pons. Over half of K27-mutant GBM developed post-treatment CNS tumor dissemination, whereas for other pedGBM molecular subsets the frequency of craniospinal metastases was much lower. No tumors displayed evidence of gross metastatic spread at initial presentation.
Correlation of pedGBM subgroups and other clinical or molecular parameters with patient outcome revealed a number of significant associations. IDH1-mutant tumors showed a significantly longer survival than the other subgroups (p = 6.5 × 10−5), while K27M GBM showed a significantly worse outcome (p = 7.6 × 10−13) (Fig. 3a). G34R-mutant tumors showed a trend towards increased survival, but this was not significantly different from WT tumors (p = 0.16). Univariate overall survival analysis for various clinical and molecular parameters revealed that midline tumor location, K27M mutation and presence of oncogene amplification(s) were each associated with poor outcome, whereas male gender, presence of G34 or IDH1 mutations, 9p21 deletion and MGMT promoter methylation were associated with a more favorable clinical course (Table 2). Some variables were also found to be significant within particular GBM subsets. For G34-mutant tumors, male gender was associated with a significantly better prognosis (p = 0.04), while presence of an oncogene amplification was a negative prognostic marker (p = 0.001). Amplifications were also associated with poor outcome in wt tumors (p = 0.002; Supplementary Table 4). None of the tested clinical or molecular variables were significantly associated with outcome within the K27 or IDH1 pedGBM groups. A small proportion of patients were found to survive ≥36 months after diagnosis, which would be considered as relatively ‘long-term’ survival with GBM. The clinical patient data and molecular features of these tumors are summarized in Supplementary Table 5.
a Survival analysis for molecular subtypes of 162 pediatric glioblastomas according to IDH1 and Histone 3 mutation status. Tumors with LGG-like or PXA-like profiles were excluded from this analysis. b Molecular stratification of pedGBM. pedGBM with K27 mutation and/or oncogene amplification (n = 124) were designated ‘high’ risk, while those lacking these features were considered ‘intermediate’ risk (n = 38). OS overall survival
Multivariate analysis identified the presence of amplified oncogene(s) and K27M mutation as independent significant prognostic markers for poor outcome amongst the overall pedGBM cohort (each at p < 0.01), while IDH1 mutation (p = 0.03) was a significant independent marker of longer survival (Table 2).
The above analyses together led us to propose a model for stratification of pedGBM into high- or intermediate-risk groups, based on the presence of K27 mutation and/or oncogene amplifications. In this, tumors harboring any of the focal oncogene amplifications assessed by FISH, or with a K27M mutation would be considered as high risk, while tumors lacking these markers may be considered as intermediate risk. Applying this model, the high-risk group displayed a 3-year overall survival of 5 %, while in the intermediate group it was 72 % (p = 7.55 × 10−15; Fig. 3b), suggesting potential clinical utility of this classification. The intermediate-risk group showed an enrichment for male patients, hemispheric location, G34/IDH1 mutations and MGMT methylation, while >90 % of cases displaying tumor dissemination through the CNS at recurrence were found in the high-risk group (Table 3). Therefore, together with the PXA/LGG-like cases, 78/202 (39 %) pedGBM had distinct molecular features associated with a more favorable clinical outcome.
Discussion
Given that pediatric GBMs are clinically and biologically heterogeneous, improvements in therapy will require patient stratification based upon their molecular hallmarks. In the current study, we have investigated a representative cohort of homogeneously treated primary pedGBM using genome-wide DNA methylation profiling and other targeted methods for verification. Array-based DNA methylation analysis has significant potential for modern molecular pathology, because it is technically applicable for everyday practice using small amounts of DNA extracted from routine FFPE samples [17]. Moreover, this analysis allows the simultaneous evaluation of various components of a tumor’s molecular signature, including the global methylome (which may correlate with specific point mutations in, e.g., IDH1 or H3F3A), target gene promoter methylation status (e.g., MGMT) and DNA copy number alterations [46].
Application of this technique allowed us to identify a set of tumors (almost 20 %) originally diagnosed as “GBM” (confirmed upon blinded histological re-evaluation in most cases), but which more closely resembled either PXA or LGG in terms of their DNA methylation profile. Patients suffering from these tumors showed significantly better OS in comparison to molecularly confirmed GBM, suggesting a distinct origin and less malignant nature of these tumors. There is known morphological overlap between GBM and ‘anaplastic’ PXA (aPXA) in particular, with anaplastic features portending a poorer prognosis [18]. There are currently no highly sensitive, specific and reproducible morphological criteria for the distinction of aPXA from other malignant gliomas. Some studies have shown that neuroimaging and histological characteristics of ‘epithelioid’, ‘rhabdoid’, and/or giant cell GBM overlap greatly with those described in aPXA [6, 23]. The frequency of BRAF V600E mutation in ‘true’ GBM vs. PXA is also currently unclear, although it is reported as a much more common feature in the latter group [40]. It is notable that very few molecular GBMs in our series harbored this alteration (4/162, 2 %), while roughly half of the molecularly PXA-like tumors were V600E mutant (13/27, 48 %). Although their outcome was significantly better in terms of overall survival, the PXA-like tumors still exhibited a high rate of recurrence (18/27, 67 %, recurred within the follow-up period), which calls into question the efficacy of current GBM treatment protocols for these lesions. Since therapy with targeted BRAF and/or MEK inhibitors may represent a more rational regime for these (BRAF-mutated) PXA-like cases, it is very important to identify them accurately, regardless of their histological appearance [38]. Interestingly, a recent report highlighted a similar subset of patients with secondary high-grade glioma (sHGG) arising from a lower grade precursor lesion, that were enriched for BRAF V600E mutations and CKDN2A deletion [29]. These tumors showed a longer latency to malignant transformation and a better prognosis relative to BRAF-wild-type sHGG. We believe it likely that this group of tumors is biologically related to what we define as PXA-like tumors, with frequent BRAF V600E mutation and 9p21 deletion and intermediate outcomes between WHO Grade I lesions and clear molecular GBM. Further clarification as to the nature of this apparently distinct subset through detailed analysis of additional cohorts would, therefore, be of significant value.
Tumors with GBM histology but an LGG molecular signature were highly enriched in infants, and were also associated with favorable overall survival. Some previous studies have shown that congenital and infant GBMs are chemotherapy-sensitive tumors and associated with good outcomes [10, 35]. In contrast, infant LGGs are often reported as having a markedly inferior prognosis compared with their older counterparts [3, 43]. These observations may indicate a distinct biological behavior of LGG and high-grade glioma (HGG) in infants compared with older children. It may also be the case, however, that there is simply a much higher degree of diagnostic uncertainty in gliomas of all grades in very young children, as tumors of infancy are diagnosed at an earlier, less differentiated growth phase. For example, it has been reported that more malignant-looking ‘pilomyxoid’ astrocytomas often display a more differentiated appearance upon recurrence [9]. Chemotherapy-induced differentiation of infant ‘GBM’ into histologically low-grade glioma has also previously been reported [19]. The mixing of true biological LGG and HGG into different histological grades could result in the observed discrepancies in terms of clinical outcome in infants. Our data indicate that a ‘low-grade’ epigenetic signature is a hallmark of some GBM-like infantile tumors, which could be used to identify a set of patients with a more favorable prognosis. Closer examination of such infant gliomas with high-grade histology yet low-grade molecular signature (and vice versa) is clearly warranted in future clinical trials.
Exclusion of the above tumors enabled us to further characterize the subset of pedGBM with molecular high-grade signatures, where previous studies looking at prognostic markers may have been somewhat hampered by cohort sizes; heterogeneous treatment; a lack of stratification into biological subgroups, and potentially also by intermixing with unidentified molecularly lower grade lesions [4, 8, 11, 13, 16, 25, 26, 34, 36, 42, 47]. Median overall survival in this group was only 14 months, comparable to their adult GBM counterparts. We also confirmed the presence of four biological subgroups of GBM based on their global DNA methylation patterns, which strongly correlate with genomic alterations. More than half of pedGBM had hotspot mutations in histone H3-encoding genes, thus confirming their prominent biological significance in pedGBM tumorigenesis. Tumors allocated to the various molecular subgroups also showed clear differences in clinical features, including tumor location and prognosis, as previously reported (e.g., reviewed in [45]). In keeping with earlier reports, the current study confirmed K27 pedGBM as the most unfavorable molecular variant [46]. These tumors: (1) are associated with deep midline locations and, as a consequence, have limited options for tumor resection; (2) develop frequent craniospinal tumor dissemination after treatment and (3) lack MGMT promoter methylation in almost all cases, implying a low efficacy of TMZ-based therapy. While the frequency of tumor dissemination in the K27 group is not yet fully understood (it may, for example, be related to their close contact with the ventricular system), it suggests that these highly aggressive lesions will remain a particular clinical challenge, even if better methods for local tumor control are identified. This subset may, therefore, warrant further intensified craniospinal therapy, with the addition of targeted epigenetic modifiers as they become available. On the other end of this clinical spectrum are G34- and IDH1-mutant tumors, which carried a more favorable prognosis, as previously described [46]. It is possible to speculate that the almost universal MGMT methylation identified in these groups may correlate with enhanced responsiveness to TMZ and thus better outcomes. Particularly for G34-mutant GBM, where this link has not previously been established, assessment in future clinical trials is of critical importance. Wild-type GBMs occupy an intermediate prognostic niche with a wide range of clinical outcomes, where various oncogene amplifications could portend especially unfavorable prognosis and resistance to standard treatment modalities. A low proportion of MGMT methylation in the wt group (19 %) further suggests that TMZ may be of limited benefit, with targeted RTK/MAPK/mTOR inhibitors possibly representing a more rational alternative.
In conclusion, this study demonstrates the significant molecular heterogeneity of histologically similar pediatric gliomas, as detected by global DNA methylation analysis. The recognition of a significant subset of tumors (particularly in infants) which are histologically malignant but molecularly and prognostically lower grade, is an important issue to be further assessed in additional cohorts. The utility of array-based DNA methylation profiling or other markers to identify such cases also requires further validation. Subgroups of true molecular high-grade tumors showed close correlations with clinical and biological parameters that may be predictive of response to therapy (e.g., MGMT methylation). Furthermore, a set of potential prognostic biomarkers was established that may be of use for the stratification of pedGBM into clinically relevant subsets. This grouping, applicable from minimal quantities of standard FFPE material, could enable rapid pedGBM prognostication in routine diagnostic laboratories. Practical and reliable prognostication of pediatric glioma through molecular risk algorithms will be essential for rational stratification in clinical trials and for guiding optimal targeted therapeutic regimes. In this context, our findings provide a framework for such stratification as a basis for verification in additional clinical cohorts.
References
Aihara K, Mukasa A, Gotoh K et al (2014) H3F3A K27M mutations in thalamic gliomas from young adult patients. Neuro-oncology 16(1):140–146. doi:10.1093/neuonc/not144
Bady P, Sciuscio D, Diserens AC et al (2012) MGMT methylation analysis of glioblastoma on the Infinium methylation BeadChip identifies two distinct CpG regions associated with gene silencing and outcome, yielding a prediction model for comparisons across datasets, tumor grades, and CIMP-status. Acta Neuropathol 124(4):547–560. doi:10.1007/s00401-012-1016-2
Bandopadhayay P, Bergthold G, London WB et al (2014) Long-term outcome of 4040 children diagnosed with pediatric low-grade gliomas: an analysis of the Surveillance Epidemiology and End Results (SEER) database. Pediatr Blood Cancer 61(7):1173–1179. doi:10.1002/pbc.24958
Bax DA, Mackay A, Little SE et al (2010) A distinct spectrum of copy number aberrations in pediatric high-grade gliomas. Clin Cancer Res 16(13):3368–3377. doi:10.1158/1078-0432.CCR-10-0438
Brennan CW, Verhaak RG, McKenna A et al (2013) The somatic genomic landscape of glioblastoma. Cell 155(2):462–477. doi:10.1016/j.cell.2013.09.034
Broniscer A, Tatevossian RG, Sabin ND et al (2014) Clinical, radiological, histological and molecular characteristics of paediatric epithelioid glioblastoma. Neuropathol Appl Neurobiol 40(3):327–336. doi:10.1111/nan.12093
Buczkowicz P, Hoeman C, Rakopoulos P et al (2014) Genomic analysis of diffuse intrinsic pontine gliomas identifies three molecular subgroups and recurrent activating ACVR1 mutations. Nat Genet 46(5):451–456. doi:10.1038/ng.2936
Buttarelli FR, Massimino M, Antonelli M et al (2010) Evaluation status and prognostic significance of O6-methylguanine-DNA methyltransferase (MGMT) promoter methylation in pediatric high grade gliomas. Childs Nerv Syst 26(8):1051–1056. doi:10.1007/s00381-010-1191-1
Ceppa EP, Bouffet E, Griebel R, Robinson C, Tihan T (2007) The pilomyxoid astrocytoma and its relationship to pilocytic astrocytoma: report of a case and a critical review of the entity. J Neurooncol 81(2):191–196. doi:10.1007/s11060-006-9216-z
Cohen KJ, Pollack IF, Zhou T et al (2011) Temozolomide in the treatment of high-grade gliomas in children: a report from the Children’s Oncology Group. Neuro-oncology 13(3):317–323. doi:10.1093/neuonc/noq191
Donson AM, Addo-Yobo SO, Handler MH, Gore L, Foreman NK (2007) MGMT promoter methylation correlates with survival benefit and sensitivity to temozolomide in pediatric glioblastoma. Pediatr Blood Cancer 48(4):403–407. doi:10.1002/pbc.20803
Duffner PK, Horowitz ME, Krischer JP et al (1999) The treatment of malignant brain tumors in infants and very young children: an update of the Pediatric Oncology Group experience. Neuro-oncology 1(2):152–161
Faury D, Nantel A, Dunn SE et al (2007) Molecular profiling identifies prognostic subgroups of pediatric glioblastoma and shows increased YB-1 expression in tumors. J Clin Oncol: Off J Am Soc Clin Oncol 25(10):1196–1208. doi:10.1200/JCO.2006.07.8626
Fontebasso AM, Papillon-Cavanagh S, Schwartzentruber J et al (2014) Recurrent somatic mutations in ACVR1 in pediatric midline high-grade astrocytoma. Nat Genet 46(5):462–466. doi:10.1038/ng.2950
Frattini V, Trifonov V, Chan JM et al (2013) The integrated landscape of driver genomic alterations in glioblastoma. Nat Genet 45(10):1141–1149. doi:10.1038/ng.2734
Haque T, Faury D, Albrecht S et al (2007) Gene expression profiling from formalin-fixed paraffin-embedded tumors of pediatric glioblastoma. Clin Cancer Res 13(21):6284–6292. doi:10.1158/1078-0432.CCR-07-0525
Hovestadt V, Remke M, Kool M et al (2013) Robust molecular subgrouping and copy-number profiling of medulloblastoma from small amounts of archival tumour material using high-density DNA methylation arrays. Acta Neuropathol 125(6):913–916. doi:10.1007/s00401-013-1126-5
Ida CM, Rodriguez FJ, Burger PC et al (2014) Pleomorphic xanthoastrocytoma: natural history and long-term follow-up. Brain Pathol. doi:10.1111/bpa.12217
Jeibmann A, Hasselblatt M, Pfister S et al (2009) From glioblastoma to gangliocytoma: an unforeseen but welcome shift in biological behavior. J Neurosurg Pediatr 4(5):475–478. doi:10.3171/2009.6.PEDS097
Jones C, Baker SJ (2014) Unique genetic and epigenetic mechanisms driving paediatric diffuse high-grade glioma. Nat Rev Cancer 14(10):651–661. doi:10.1038/nrc3811
Jones C, Perryman L, Hargrave D (2012) Paediatric and adult malignant glioma: close relatives or distant cousins? Nat Rev Clin Oncol 9(7):400–413. doi:10.1038/nrclinonc.2012.87
Khuong-Quang DA, Buczkowicz P, Rakopoulos P et al (2012) K27M mutation in histone H3.3 defines clinically and biologically distinct subgroups of pediatric diffuse intrinsic pontine gliomas. Acta Neuropathol 124(3):439–447. doi:10.1007/s00401-012-0998-0
Kleinschmidt-DeMasters BK, Aisner DL, Birks DK, Foreman NK (2013) Epithelioid GBMs show a high percentage of BRAF V600E mutation. Am J Surg Pathol 37(5):685–698. doi:10.1097/PAS.0b013e31827f9c5e
Koelsche C, Sahm F, Wohrer A et al (2014) BRAF-mutated pleomorphic xanthoastrocytoma is associated with temporal location, reticulin fiber deposition and CD34 expression. Brain Pathol 24(3):221–229. doi:10.1111/bpa.12111
Korshunov A, Sycheva R, Gorelyshev S, Golanov A (2005) Clinical utility of fluorescence in situ hybridization (FISH) in nonbrainstem glioblastomas of childhood. Mod Pathol 18(9):1258–1263. doi:10.1038/modpathol.3800415
Lee JY, Park CK, Park SH, Wang KC, Cho BK, Kim SK (2011) MGMT promoter gene methylation in pediatric glioblastoma: analysis using MS-MLPA. Childs Nerv Syst 27(11):1877–1883. doi:10.1007/s00381-011-1525-7
Lewis PW, Muller MM, Koletsky MS et al (2013) Inhibition of PRC2 activity by a gain-of-function H3 mutation found in pediatric glioblastoma. Science 340(6134):857–861. doi:10.1126/science.1232245
Louis DN, Ohgaki H, Wiestler OD et al (2007) The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 114(2):97–109. doi:10.1007/s00401-007-0243-4
Mistry M, Zhukova N, Merico D et al (2015) BRAF mutation and CDKN2A deletion define a clinically distinct subgroup of childhood secondary high-grade glioma. J Clin Oncol: Off J Am Soc Clin Oncol. doi:10.1200/JCO.2014.58.3922
Ostrom QT, Gittleman H, Liao P et al (2014) CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2007–2011. Neuro-oncology 16(Suppl 4):iv1–63. doi:10.1093/neuonc/nou223
Parsons DW, Jones S, Zhang X et al (2008) An integrated genomic analysis of human glioblastoma multiforme. Science 321(5897):1807–1812. doi:10.1126/science.1164382
Paugh BS, Broniscer A, Qu C et al (2011) Genome-wide analyses identify recurrent amplifications of receptor tyrosine kinases and cell-cycle regulatory genes in diffuse intrinsic pontine glioma. J Clin Oncol: Off J Am Soc Clin Oncol 29(30):3999–4006. doi:10.1200/JCO.2011.35.5677
Paugh BS, Qu C, Jones C et al (2010) Integrated molecular genetic profiling of pediatric high-grade gliomas reveals key differences with the adult disease. J Clin Oncol: Off J Am Soc Clin Oncol 28(18):3061–3068. doi:10.1200/JCO.2009.26.7252
Phillips JJ, Aranda D, Ellison DW et al (2013) PDGFRA amplification is common in pediatric and adult high-grade astrocytomas and identifies a poor prognostic group in IDH1 mutant glioblastoma. Brain Pathol 23(5):565–573. doi:10.1111/bpa.12043
Pollack IF, Finkelstein SD, Burnham J et al (2001) Age and TP53 mutation frequency in childhood malignant gliomas: results in a multi-institutional cohort. Cancer Res 61(20):7404–7407
Puget S, Philippe C, Bax DA et al (2012) Mesenchymal transition and PDGFRA amplification/mutation are key distinct oncogenic events in pediatric diffuse intrinsic pontine gliomas. PLoS One 7(2):e30313. doi:10.1371/journal.pone.0030313
Qu HQ, Jacob K, Fatet S et al (2010) Genome-wide profiling using single-nucleotide polymorphism arrays identifies novel chromosomal imbalances in pediatric glioblastomas. Neuro-oncology 12(2):153–163. doi:10.1093/neuonc/nop001
Robinson GW, Orr BA, Gajjar A (2014) Complete clinical regression of a BRAF V600E-mutant pediatric glioblastoma multiforme after BRAF inhibitor therapy. BMC Cancer 14:258. doi:10.1186/1471-2407-14-258
Schiffman JD, Hodgson JG, VandenBerg SR et al (2010) Oncogenic BRAF mutation with CDKN2A inactivation is characteristic of a subset of pediatric malignant astrocytomas. Cancer Res 70(2):512–519. doi:10.1158/0008-5472.CAN-09-1851
Schindler G, Capper D, Meyer J et al (2011) Analysis of BRAF V600E mutation in 1320 nervous system tumors reveals high mutation frequencies in pleomorphic xanthoastrocytoma, ganglioglioma and extra-cerebellar pilocytic astrocytoma. Acta Neuropathol 121(3):397–405. doi:10.1007/s00401-011-0802-6
Schwartzentruber J, Korshunov A, Liu XY et al (2012) Driver mutations in histone H3.3 and chromatin remodelling genes in paediatric glioblastoma. Nature 482(7384):226–231. doi:10.1038/nature10833
Srivastava A, Jain A, Jha P et al (2010) MGMT gene promoter methylation in pediatric glioblastomas. Childs Nerv Syst 26(11):1613–1618. doi:10.1007/s00381-010-1214-y
Stokland T, Liu JF, Ironside JW et al (2010) A multivariate analysis of factors determining tumor progression in childhood low-grade glioma: a population-based cohort study (CCLG CNS9702). Neuro-oncology 12(12):1257–1268. doi:10.1093/neuonc/noq092
Stupp R, Mason WP, van den Bent MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352(10):987–996. doi:10.1056/NEJMoa043330
Sturm D, Bender S, Jones DT et al (2014) Paediatric and adult glioblastoma: multiform (epi)genomic culprits emerge. Nat Rev Cancer 14(2):92–107. doi:10.1038/nrc3655
Sturm D, Witt H, Hovestadt V et al (2012) Hotspot mutations in H3F3A and IDH1 define distinct epigenetic and biological subgroups of glioblastoma. Cancer Cell 22(4):425–437. doi:10.1016/j.ccr.2012.08.024
Suri V, Das P, Pathak P et al (2009) Pediatric glioblastomas: a histopathological and molecular genetic study. Neuro-oncology 11(3):274–280. doi:10.1215/15228517-2008-092
Taylor KR, Mackay A, Truffaux N et al (2014) Recurrent activating ACVR1 mutations in diffuse intrinsic pontine glioma. Nat Genet 46(5):457–461. doi:10.1038/ng.2925
Weber RG, Hoischen A, Ehrler M et al (2007) Frequent loss of chromosome 9, homozygous CDKN2A/p14(ARF)/CDKN2B deletion and low TSC1 mRNA expression in pleomorphic xanthoastrocytomas. Oncogene 26(7):1088–1097. doi:10.1038/sj.onc.1209851
Weller M, Pfister SM, Wick W, Hegi ME, Reifenberger G, Stupp R (2013) Molecular neuro-oncology in clinical practice: a new horizon. Lancet Oncol 14(9):e370–e379. doi:10.1016/S1470-2045(13)70168-2
Weller M, van den Bent M, Hopkins K et al (2014) EANO guideline for the diagnosis and treatment of anaplastic gliomas and glioblastoma. Lancet Oncol 15(9):e395–e403. doi:10.1016/S1470-2045(14)70011-7
Wu G, Broniscer A, McEachron TA et al (2012) Somatic histone H3 alterations in pediatric diffuse intrinsic pontine gliomas and non-brainstem glioblastomas. Nat Genet 44(3):251–253. doi:10.1038/ng.1102
Wu G, Diaz AK, Paugh BS et al (2014) The genomic landscape of diffuse intrinsic pontine glioma and pediatric non-brainstem high-grade glioma. Nat Genet 46(5):444–450. doi:10.1038/ng.2938
Yan H, Parsons DW, Jin G et al (2009) IDH1 and IDH2 mutations in gliomas. N Engl J Med 360(8):765–773. doi:10.1056/NEJMoa0808710
Acknowledgments
For technical support and expertise we thank Andrea Wittmann and Matthias Schick, Roger Fischer and Melanie Bewerunge-Hudler from the DKFZ Genomics and Proteomics Core Facility. This work was principally supported by the PedBrain Tumor Project contributing to the International Cancer Genome Consortium, funded by German Cancer Aid (109252) and by the German Federal Ministry of Education and Research (BMBF, grants #01KU1201A, MedSys #0315416C and NGFNplus #01GS0883). Additional support came from the German Cancer Research Center—Heidelberg Center for Personalized Oncology (DKFZ-HIPO) Personalized Oncology Program (POP).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Korshunov, A., Ryzhova, M., Hovestadt, V. et al. Integrated analysis of pediatric glioblastoma reveals a subset of biologically favorable tumors with associated molecular prognostic markers. Acta Neuropathol 129, 669–678 (2015). https://doi.org/10.1007/s00401-015-1405-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-015-1405-4