Abstract
The chromogenic and neurotoxic γ-diketone 1,2–diacetylbenzene (1,2-DAB), but not its isomer 1,3-DAB, induces blue discoloration of tissues and urine, clustering of axonal microtubules and proximal neurofilament-filled axonal swellings in rodents. The remarkable chromogenic property of 1,2-DAB, a monocyclic aromatic hydrocarbon, arises from reaction with lysine residues of proteins and formation of dimeric and polymeric derivatives. Tetralin, a dicyclic solvent structurally related to acetyl ethyl tetramethyl tetralin, a chromogenic and neurotoxic agent, reportedly induces excretion of green urine, and causes neurological disturbances in humans. Monocyclic aromatic 1,2,4-triethylbenzene (1,2,4-TEB), but not its isomer 1,3,5-TEB, is also reportedly chromogenic and induces neurophysiological deficits in rodents consistent with axonal neuropathy, but without neuropathological confirmation. We treated 12-week-old C57Bl/6 mice by gavage with 300, 600, or 900 mg/kg/day 1,2,4-TEB, or equivalent doses of 1,3,5-TEB, 3 days/week, for up to 12 weeks, or intraperitoneally with 400 mg/kg/day tetralin, or 50 or 100 mg/kg/day of its α-tetralol analogue, 5 days/week, for up to 5 weeks. Animals treated with 1,2,4-TEB, but not 1,3,5-TEB, tetralin or α-tetralol, developed hind limb weakness, excreted greenish urine, and showed 1,2-DAB-like neuropathology. These findings support the hypothesis that 1,2-spaced ethyl (or acetyl) moieties on a benzene ring of hydrocarbons are required for hydrocarbons to induce chromogenic changes and proximal giant neurofilamentous axonopathy. Key molecular targets of these compounds likely reside in the axon where they serve to maintain normal cytoskeletal organization.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The aromatic hydrocarbon 1,2-diacetylbenzene (1,2-DAB), an ortho diacetyl metabolite of the solvent 1,2-diethylbenzene (1,2-DEB), reacts as a γ-diketone with ε-amino groups of lysines in proteins to form a blue pigment, causes blue-greenish discoloration of urine and tissues, and induces proximal giant neurofilamentous axonopathy in rodents; by contrast, its isomer 1,3-DAB (which lacks an ortho diacetyl structure) fails to react with proteins, is non-chromogenic, and does not induce axonopathy [14, 15, 27]. Properties comparable to those of 1,2-DAB and 1,3-DAB have been reported for 2,5-hexanedione (2,5-HD), the neurotoxic aliphatic γ-diketone metabolite of n-hexane, and its non-neurotoxic isomer 2,4-HD, respectively. Neurotoxic 2,5-HD reacts with amino acids and ε-amino groups of lysines in proteins to form pyrrole polymers with an orange hue; with prolonged incubation in vitro, these form blue-purple isoindole compounds comparable to the blue chromogen produced by 1,2-DAB and proteins [6, 14, 22, 26]. These findings demonstrate a relationship between the protein-reactive, chromogenic, and neurotoxic properties of aromatic (1,2-DAB) and aliphatic (2,5-HD) γ-diketones, both of which are oxidation products of the corresponding solvents 1,2-DEB and n-hexane, respectively [6, 8].
1,2-DEB and 1,3-DEB appear on a 1960 list of commercially important monocyclic and dicyclic hydrocarbon solvents that induced the excretion of greenish urine by rats treated with large, single subcutaneous doses [11] (Table 1). The listed agents may have been impure in the 1950s when the studies were performed. Indeed, studies published in the 1990s demonstrated that a pure sample of 1,2-DEB, but not of 1,3-DEB, was chromogenic and neurotoxic in repeatedly treated rats, presumably because the 1,2-DEB metabolite (1,2-DAB) but not the corresponding 1,3-DEB metabolite reacts with proteins to form blue-colored pigments [9, 14, 29]. Our previous work with aromatic hydrocarbons has shown a direct association between protein reactivity, chromogenicity, and neurotoxicity of the axonopathy type [14, 15, 22, 27].
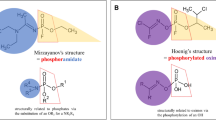
We have continued our series of studies to define the structural requirements for chromogenicity and neurotoxicity of the monocyclic and dicyclic hydrocarbon solvents described in Gerarde’s 1960 list (Table 1 and Fig. 1). The present experimental murine studies examine the neurotoxic potential of individual monocylic triethylbenzenes (TEB), namely 1,2,4-TEB and 1,3,5-TEB, and the dicyclic hydrocarbon solvent tetralin (and its metabolite α-tetralol), reportedly a compound that in native or derivatized form is chromogenic and acutely neurotoxic in both rodents and humans [5, 20, 21]. These studies demonstrate that 1,2,4-TEB alone, the only one of the four tested agents with potential to form a γ-diketone metabolite (1,2,4-TAB), has chromogenic and neurotoxic properties, and induces 1,2-DAB-like giant proximal axonopathy.
a Chemical structures of neurotoxic solvents (parent compounds, their putative active γ-diketone metabolites, and their non-neurotoxic isomers. Note structural similarities (1,4 spacing of ethyl groups) between the neurotoxic solvents 1,2-DEB and 1,2,4-TEB and between 2,5-HD and 1,2-DAB (1,4 spacing of acetyl groups), the γ-diketone neurotoxic metabolites of n-hexane and 1,2-DEB, respectively. 1,2,4-TAB, a putative γ-diketone neurotoxic metabolite of 1,2,4-TEB shares the same similarity. b Chemical structures of neurotoxic AETT (tetralin derivative), its putative γ-diketone metabolite keto-AETT, tetralin and α-tetralol
Materials and methods
Chemicals
1,2,4-TEB (99.4%), 1,3,5-TEB (99.8%), tetralin (99%), and α-tetralol (97%) were purchased from Aldrich Chemical Co. (Madison, WI). Compounds were stored at room temperature (tetralin, α-tetralol), desiccated at room temperature (1,2,4-TEB), or stored at 4°C (1,3,5-TEB). Purity of stock samples was checked by gas chromatography-mass spectrometry (GC-MS). Impurities could not be readily identified, but 1,3,5-TEB was found to be free of 1,2,4-TEB and vice-versa, and tetralin was free of α-tetralol and vice-versa.
Animals
These were 12-week-old C57 Bl/6 male mice and 9-week-old Sprague-Dawley rats (Charles River, CA) each weighing ∼25 and 300 g on arrival, respectively. Mice were singly housed in cages supplied with soft and absorbent bedding, whereas rats were individually housed in metabolic cages. Stacked cages were held in a room provided with a 12-h/12-h light–dark cycle and maintained at the temperature of 20°C. Animals were given a rodent chow (PMI® Nutrition International, NJ) and water ad libitum; they were acclimated for up to 5 days prior to the treatment with the test articles. All aspects of this study were conducted in accordance with the institutional guide for care and use of laboratory animals.
Dosing regimens
Tetralin and α-tetralol
Rat study
To reproduce Gerarde’s 1950 experiments [11], rats (n = 2) were treated subcutaneously (s.c.) with a single injection of neat tetralin at the dose of 5 ml/kg body weight and observed for physical and behavioral changes, and changes in the color of urine. Animals were individually placed in metabolic cages and 24-h urine collected and subjected to GC-MS analysis for the presence of the test article and/or its metabolites according to the method of Serve and colleagues [19]. After 24 h, the animals were severely ill; they were anesthetized with 4% isofluorane (0.5 l oxygen/min) and their internal organs examined for any tissue discoloration prior to euthanasia by decapitation.
Mice study
A preliminary study was performed to estimate the toxic potency of tetralin and α-tetralol in mice (n = 8) equally divided into two groups. Animals were treated intraperitoneally (i.p.) with either 800 mg/kg/day (n = 2) or 1,600 mg/kg/day (n = 2) of each test article for up to 7 days. Injectate was prepared daily by dissolving the test article in HPLC-grade acetone followed by the addition of saline to a concentration of 2% acetone; this produced an emulsion that was vortexed immediately prior to animal treatment. Mice with severe illness were terminated by decapitation and their internal organs examined for discoloration. All animals treated with α-tetralol showed severe illness on the first day and were subsequently terminated.
A formal experiment was conducted with mice treated with 50 mg/kg/day (n = 2) or 100 mg/kg/day (n = 4) α-tetralol, 400 mg/kg/day (n = 4) tetralin, or vehicle (8 μl/g saline containing 2% acetone, n = 4), 5 days a week, for up to 5 weeks. Test articles were administered via the intraperitoneal route with a 1-ml disposable plastic syringe equipped with a 27-gauge needle. Injection sites were rotated around the abdomen to minimize discomfort, and care was taken to minimize leakage from the injection site.
Study of TEB isomers
Mice were dosed by gastric intubation with 300 mg/kg (n = 3), 600 mg/kg (n = 3), or 900 mg/kg (n = 3) 1,2,4-TEB or its isomer 1,3,5-TEB, or vehicle (8 μl/g olive oil), 3 days a week (i.e. days 2, 4, and 6), for up to 12 weeks. The solution for gavage was prepared daily by mixing the test article with olive oil in varying proportions according to the dosage to be administered. The test article was given in a 1-ml disposable plastic syringe equipped with a 21-gauge gavage needle that was inserted into the lower esophagus.
Animal observation
Animals were daily observed in their home-cages for position, movement, and activity level. Each animal was placed in an open field (uncovered plexiglass box 45 in. square, 10 in. height) and was observed for ability to walk, locomotion pattern, and reaction to tail pinch. Locomotion was rated semi-quantitatively as follows: 1 = normal; 2 = slightly affected (walking on tip-toes or hunched-back gait, broad-based gait, abnormal outward rotation of the hind limbs), 3 = moderately affected (hind limb dragging), 4 = severely affected (“duck-walk”, inability to walk). Digital video recordings were made of selected animals for further analysis of their locomotion and/or other physical signs. Animals were weighed and treated with the test article immediately thereafter.
Tissue preparation and examination
For morphological study, animals were deeply anesthetized with 4% isofluorane (0.5 l oxygen/min) prior to systemic perfusion with tissue fixatives. The abdomen and chest were opened and the heart injected with 50 μl of heparin (1,000 USP units/ml) solution. Immediately thereafter, the left atrium and ventricular apex were excised, a cannula spurting perfusate introduced and clamped into the ascending aorta, and the animal perfused with 4% paraformaldehyde followed by 5% glutaraldehyde, each in 0.2 M sodium cacodylate buffer (pH 7.4). Tissues were sampled from the central nervous system (CNS) and peripheral nervous system (PNS). CNS tissues included frontal cortex, hippocampus, basal ganglia, cerebellum, medulla oblongata, lumbar and cervical spinal cords. PNS tissues included lumbar dorsal and ventral spinal roots, lumbar dorsal root ganglia, sciatic, tibial, peroneal, and sural nerves. Peripheral nerves were excised and cut into proximal, medium, and distal segments. All tissues were post-fixed in excess cacodylate-buffered 1% osmium tetroxide (pH 7.4), dehydrated, and embedded in epoxy resin. Cross sections (∼900 nm thick) were stained with 1% toluidine blue and screened by bright-field microscopy. Thin sections (∼90 nm) of regions of special interest were stained with 2% uranyl acetate followed by 1% lead citrate for examination by transmission electron microscopy.
Statistical methods
The weekly body weight for each animal was calculated as the median of five daily measurements for each week; this yielded weekly body-weight profiles for 13 animals; three animals had data from only the first week and were excluded from further analysis. Profiles from each animal were adjusted so that all had the same average first-week body weight. The remaining time points (weeks 2–13) were used for analysis. A linear mixed-effect model [17] was used to analyze the changes in body weight over time (slope), compare differences between vehicle and TEB-treated animals and compare differences between the two forms of TEB within a given dose. Daily locomotion scores from the same 16 animals were transformed to weekly scores in the same manner as for body weight. All computations were performed using version 2.0.1 of R [18].
Results
Animal observations
Study of tetralin and α-tetralol
Tetralin-treated rats (5 ml/kg) and mice that received α-tetralol at a dose ≥ 800 mg/kg were terminated within 24 h as they became severely ill. Animals showed treatment-related changes consisting of drowsiness, acute respiratory distress, and lethargy with greater acute toxicity for α-tetralol. Rats excreted dark brown urine. Mice showed no urine or tissue discoloration. During the formal 5-week experiment, mice showed decreased reactivity to touch and tail pinch, wasting, and generalized weakness in proportion to the total dose of the test article. There was no evidence to suggest specific drug-related neuromuscular (γ-diketone-like) weakness.
Study of TEB isomers
Mice treated with 1,2,4-TEB, but not 1,3,5-TEB or vehicle, displayed blue-green discoloration of urine and CNS/PNS tissues, including the brain, spinal cord, and peripheral nerves. Blue-green urine was first seen after 5 days of treatment with 900 mg/kg of TEB.
Animals receiving 300 mg/kg of 1,2,4-TEB or vehicle gained body weight at a similar rate through the entire experiment (∼0.4 g/week for both treatments). Animals that received 600 mg/kg failed to gain significant weight (∼0.01 g/week); those that received 900 mg/kg lost weight at a rate of ∼0.11 g/week (Table 2). In comparison to the vehicle-treated animals, the highest dose of 1,2,4-TEB (900 mg/kg/d) induced significant changes (P < 0.05) in body weight only later during the course of the experiment, i.e. after 10 weeks of treatment (Table 3). Animals developed limb weakness in proportion to the total dose of the chemical (Fig. 2). Animals treated with 1,3,5-TEB showed a constant increase in body weight (between 0.24 and 0.57 g/week) regardless of the dosage (Table 2, Fig. 3).
Mice treated with 1,2,4-TEB, but not 1,3,5-TEB or vehicle, developed muscle spasms, limb weakness, and walking difficulties in the following sequence: tip-toe walking, outward rotation of hindlimbs, dragging of hind limbs, duck-walk and, eventually, complete inability to walk. Signs of neuromuscular compromise in animals treated with 600 mg/kg or 900 mg/kg 1,2,4-TEB (but not 300 mg/kg) were observed after treatment periods of ∼7 weeks and 2 weeks, respectively. Animals treated with 300 mg/kg 1,2,4-TEB developed slight walking difficulties (tip-toe and broad-based gait) noticeable after ∼8 weeks of treatment. These signs remained unchanged until the termination of the study (12 weeks).
Morphological findings
Mice treated with 1,2,4-TEB, but not 1,3,5-TEB or vehicle, showed two major types of abnormality. First, microscopic examination of distal sciatic nerves revealed disorganization of the axonal cytoskeleton with clustering of microtubules and organelles (Fig. 4). Microtubule clustering was seen in the presence or absence of the second type of change, namely the development of time and dose-dependent giant axonal swellings in lumbar ventral roots, anterior horns, and dorsal root ganglia. Mice treated with 300 or 600 mg/kg 1,2,4-TEB showed giant axonal swellings most prominently in lumbar ventral roots and to a lesser extent in dorsal root ganglia (Fig. 5). Nerve fibers within lumbar ventral roots and dorsal root ganglia also exhibited myelin bubbles containing shrunken axons. Treatment with 900 mg/kg 1,2,4-TEB was associated with these changes in lumbar ventral roots, dorsal root ganglia, and spinal anterior horns (Fig. 6). Electron microscopy of intraspinal swollen axons revealed tightly packed and maloriented 10-nm neurofilaments (NFs) (Fig. 7). Lumbar dorsal horns and distal segments of afferent dorsal roots were usually unremarkable. Axonal swellings were also seen in the cervical anterior horns, and the lower medulla oblongata, proximal to the hypoglossal nucleus (not shown). No noticeable changes were seen in the cerebellum, hippocampus, basal ganglia, or frontal cortex. CNS and PNS tissues from animals treated with 1,3,5-TEB, tetralin, α-tetralol, or vehicle were unremarkable.
Distal sciatic nerve of a mouse treated with 900 mg/kg 1,2,4-TEB 3 days/week for 12 weeks. Electron micrograph shows the clustering of axonal microtubules and mitochondria (box and inset) in a myelinated fiber. This animal also had giant intraspinal axonal swellings filled with 10-nm neurofilaments. Epoxy-embedded tissues stained with 2% uranyl acetate followed by 1% lead citrate.
Lumbar anterior horns of animals treated with a vehicle, b 900 mg/kg 1,2,4-TEB, or c an equivalent dosage of 1,3,5-TEB 3 days/week for 12 weeks. Axonal swellings (*) are evident in anterior horns of mice treated with 1,2,4-TEB, but not with 1,3,5-TEB or vehicle. Epoxy-embedded tissues stained with 1% toluidine blue
a Electron micrograph of intraspinal swollen axons in anterior horns of animals treated with 900 mg/kg 1,2,4-TEB 3 days/week for 12 weeks. b Enlarged view of box in a, showing densely packed and maloriented 10-nm NFs associated with a mitochondrion (m). Epoxy-embedded tissues stained with 2% uranyl acetate followed by 1% lead citrate
Discussion
These findings show that 1,2,4-TEB, but not 1,3,5-TEB, is chromogenic and axonopathic. The respective neurotoxic and non-neurotoxic properties of these benzene derivatives are shared with those of 1,2-DEB and 1,3-DEB [9], 1,2-DAB and 1,3-DAB [8, 15, 27], and 2,5-HD and 2,4-HD [23]. Tetralin and α-tetralol lacked chromogenicity and neurotoxicity in contrast to acetyl ethyl tetramethyl tetralin (AETT), the diketone metabolite of which is also chromogenic but untested for neurotoxic properties [21, 24]. The prominent spinal root demyelination reported after prolonged (30 weeks) treatment of rats with AETT is consistent with the late effects (secondary demyelination) of a 1,2-DAB-like or 1,2,4-TEB-like axonopathy—not a myelinopathy as previously surmised [24, 25]. Taken in concert, therefore, the present findings support the hypothesis that monocyclic and dicyclic aromatic hydrocarbons lack chromogenicity and neurotoxicity unless they have a side chain that can pose as or be metabolized to a γ-diketone-like structure [10, 21, 22]. This would exclude several commercially important compounds listed in Table 1, and it would also exclude trimethylbenzene mixtures provided they lack an impurity such as 1,2,4-TEB.
1,2,4-TEB induces a 1,2-DAB-like neuropathology consisting of proximal giant axonal swellings filled with 10-nm NFs. Segregation of cytoskeleton elements, with clustering of microtubules and organelles, is another important early feature of this axonopathy. That axonal microtubule clustering was detected prior to and concurrent with the development of axonal swellings suggests it is an early event in the pathological process. Indeed, previous studies demonstrated that microtubule clustering takes place within minutes of direct application of a gamma-diketone (2,5-HD) to the living rat sciatic nerve (30). This observation is of paramount importance because it appears to be a common feature of both 1,2,4-TEB—which is likely to be metabolized into active γ-diketones such as 1,2-diacetyl-4-ethylbenzene (1,2-DA-4-EB), 1,3,4-triacetylbenzene (1,2,4-TAB), and/or 1,2-diacetyl-4(1′hydroxy)-ethylbenzene (1,2-DA-4(1′-OH)-EB)—1,2-DAB, and 2,5-HD neuropathies [27, 28]. It is therefore likely that both aliphatic and aromatic γ-diketones induce axonopathy by common molecular mechanisms that involve attack on proteins required for maintenance of axon cytoskeletal integrity.
Mechanisms of axonal swelling resulting from the time-dependent accumulation of 10-nm NFs are not understood. Proximal γ-diketone-like NF-filled axonal swellings have been reported in other neurological disorders including amyotrophic lateral sclerosis in humans, for which the pathogenetic mechanism remains enigmatic [1, 7, 13, 16] and experimental IDPN- (β,β‘-iminodipropionitrile) induced neuropathy, where arrest of slow but not fast axonal transport has been demonstrated [12]. Whereas NFs accumulate in distal regions of axons after repeated systemic treatment with the less protein-reactive 2,5-HD, stepwise-more potent 3-methyl-2,5-hexanedione and 3,4-dimethyl-2,5-hexanedione (DMHD) cause the development of mid-level and 1,2-DAB-like proximal NF-filled axonal swellings, respectively [2–4,15, 27]; of which the latter are also inducible with 1,2,4-TEB. The differential ability of γ-diketones to react with proteins according to their total lysine content has been proposed to explain how these compounds may induce proximal or distal accumulation of NFs depending on their ability to disrupt the transport of axonal cargo via crosslinking of motor and/or other structural proteins within the axon [6, 14, 22]. Further studies on axonal transport in γ-diketone-induced neuropathy are needed to confirm this hypothesis.
Neither tetralin nor its metabolite α-tetralol induced chromogenic changes or neuropathology. Both compounds induced lethargy, drowsiness, and respiratory distress with greater acute toxicity for α-tetralol. GC-MS analysis confirmed that α-tetralol was the most abundant metabolite of tetralin. It is possible that tetralin exerts an acute neurotoxic effect via its α-tetralol metabolite that acts ultimately as CNS depressant [20]. Long-term dosing of mice with these two compounds resulted in wasting, diminished reactivity to touch and tail pinch, lethargy, and progressive generalized weakness. These signs suggest non-specific systemic toxicity that could be explained by the indirect effect (metabolic) that tetralin and/or its α-tetralol metabolite would cause after inducing hemolysis and/or kidney damage [5, 19]. Rats excreted dark brown urine presumably reflecting hemolysis after treatment with a high dose of tetralin [5]. A clear distinction should be made between urine (and/or tissue) discoloration induced by the presence of neurotoxic chromophores and that reflecting the presence of hemoglobin by-products after hemolysis.
References
Al Chalabi A, Miller CC (2003) Neurofilaments and neurological disease. Bioessays 25:346–355
Anthony DC, Boekelheide K, Anderson CW, Graham DG (1983) The effect of 3,4-dimethyl substitution on the neurotoxicity of 2,5-hexanedione. II. Dimethyl substitution accelerates pyrrole formation and protein crosslinking. Toxicol Appl Pharmacol 71:372–382
Anthony DC, Boekelheide K, Graham DG (1983) The effect of 3,4-dimethyl substitution on the neurotoxicity of 2,5-hexanedione. I. Accelerated clinical neuropathy is accompanied by more proximal axonal swellings. Toxicol Appl Pharmacol 71:362–371
Anthony DC, Giangaspero F, Graham DG (1983) The spatio-temporal pattern of the axonopathy associated with the neurotoxicity of 3,4-dimethyl-2,5-hexanedione in the rat. J Neuropathol Exp Neurol 42:548–560
Browning E (1965) Toxicity and metabolism of industrial solvents. American Elsevier, New York
DeCaprio AP (2000) n-Hexane, metabolites, and derivatives. In: Spencer PS, Schaumburg HH (eds) Experimental and clinical neurotoxicology. Oxford University Press, New York pp 633–648
Delisle MB, Carpenter S (1984) Neurofibrillary axonal swellings and amyotrophic lateral sclerosis. J Neurol Sci 63:241–250
Gagnaire F, Ensminger A, Marignac B, De Ceaurriz J (1991) Possible involvement of 1,2-diacetylbenzene in diethylbenzene-induced neuropathy in rats. J Appl Toxicol 11:261–268
Gagnaire F, Marignac B, De Ceaurriz J (1990) Diethylbenzene-induced sensorimotor neuropathy in rats. J Appl Toxicol 10:105–112
Gagnaire F, Marignac B, De Ceaurriz J (1993) Triethylbenzene-induced sensorimotor neuropathy in rats. J Appl Toxicol 13:123–128
Gerarde H (1960) Toxicology and biochemistry of aromatic hydrocarbons. In: Browning E (ed) Elsevier monographs on toxic agents. Elsevier, Amsterdam, p 73
Griffin JW, Parhad I, Gold B, Price DL, Hoffman PN, Fahnestock K (1985) Axonal transport of neurofilament proteins in IDPN neurotoxicity. Neurotoxicology 6:43–53
Hirano A, Donnenfeld H, Sasaki S, Nakano I (1984) Fine structural observations of neurofilamentous changes in amyotrophic lateral sclerosis. J Neuropathol Exp Neurol 43:461–470
Kim MS, Hashemi SB, Spencer PS, Sabri MI (2002) Amino acid and protein targets of 1,2-Diacetylbenzene, a potent aromatic gamma-diketone that induces proximal neurofilamentous axonopathy. Toxicol Appl Pharmacol 183:55–65
Kim MS, Sabri MI, Miller VH, Kayton RJ, Dixon DA, Spencer PS (2001) 1,2-Diacetylbenzene, the neurotoxic metabolite of a chromogenic aromatic solvent, induces proximal axonopathy. Toxicol Appl Pharmacol 177:121–131
Okamoto K, Hirai S, Shoji M, Senoh Y, Yamazaki T (1990) Axonal swellings in the corticospinal tracts in amyotrophic lateral sclerosis. Acta Neuropathol (Berl) 80:222–226
Pinheiro JC, Bates DM (2000) Mixed-effect models in S and S-PLUS. Springer, Berlin Heidelberg New York
R Development Core Team (2004) R: A language and environment for statistical computing. R Foundation for Statistical Computing, Austria
Serve MP, Llewelyn BM, Yu KO, McDonald GM, Olson CT, Hobson DW (1989) Metabolism and nephrotoxicity of tetralin in male Fischer 344 rats. J Toxicol Environ Health 26:267–275
Snyder R (1987) Ethyl Browning’s toxicity and metabolism of industrial solvents. Elsevier, Amsterdam
Spencer PS (2000) Acetyl ethyl tetramethyl tetralin. In: Spencer PS, Schaumburg HH (eds) Experimental and clinical neurotoxicology. Oxford University Press, New York pp 112–115
Spencer PS, Kim MS, Sabri MI (2002) Aromatic as well as aliphatic hydrocarbon solvent axonopathy. Int J Hyg Environ Health 205:131–136
Spencer PS, Schaumburg HH, Sabri MI, Veronesi B (1980) The enlarging view of hexacarbon neurotoxicity. Crit Rev Toxicol 7:279–356
Spencer PS, Sterman AB, Horoupian DS, Foulds MM (1979) Neurotoxic fragrance produces ceroid and myelin disease. Science 204:633–635
Sterman AB, Spencer PS (1981) The pathogenesis of primary internodal demyelination produced by acetyl ethyl tetramethyl tetralin: evidence for preserved Schwann cell somal function. J Neuropathol Exp Neurol 40:112–121
Trimpin S, Mixon AE, Stapels MD, Kim MY, Spencer PS, Deinzer ML (2004) Identification of endogenous phosphorylation sites of bovine medium and low molecular weight neurofilament proteins by tandem mass spectrometry. Biochemistry 43:2091–2105
Tshala-Katumbay DD, Palmer VS, Kayton RJ, Sabri MI, Spencer PS (2005) A new murine model of giant proximal axonopathy. Acta Neuropathol (Berl) 109:405–410
Zagoren JC, Politis MJ, Spencer PS (1983) Rapid reorganization of the axonal cytoskeleton induced by a gamma diketone. Brain Res 270:162–164
Zhan CG, Dixon DA, Sabri MI, Kim MS, Spencer PS (2002) Theoretical determination of chromophores in the chromogenic effects of aromatic neurotoxicants. J Am Chem Soc 124:2744–2752
Acknowledgments
We thank Dan Austin and Juan Muniz for their technical expertise. These studies were supported by PHS grants P42ES10338, U19ES11384, K01NS052183 and the Oregon Worker Benefit Fund.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tshala-Katumbay, D.D., Palmer, V.S., Lasarev, M.R. et al. Monocyclic and dicyclic hydrocarbons: structural requirements for proximal giant axonopathy. Acta Neuropathol 112, 317–324 (2006). https://doi.org/10.1007/s00401-006-0106-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-006-0106-4