Abstract
Nerve agents are organophosphate (OP) compounds, similar to OP pesticides, and are a group of potentially lethal chemical warfare agents (CWA). They are extremely potent inhibitors of the enzyme acetylcholinesterase (AChE), a key regulator of cholinergic neurotransmission. Early attempts in the synthesis of OP were made by Von Hofman, who developed methylphosphor chloride in 1873. Michaelis in 1903 introduced a compound with P – CN bond, which led to the synthesis of many OP compounds, including the nerve agent tabun. Lang and Von Kreuger synthesized compounds with P – F linkage in 1932. Schrader developed sarin and tabun in 1937; in 1944, Germans developed soman. British scientists developed VX in 1952 [1].
Access provided by CONRICYT-eBooks. Download reference work entry PDF
Similar content being viewed by others
Keywords
- Nerve agents
- Organophosphate
- Chemical warfare agents
- Acetylcholinesterase
- VX
- Matsumoto
- GA
- GB
- GD
- Tabun
- Sarin
- Soman
- Persistent nerve agent
- Butyrylcholinesterase
- Pseudocholinesterase
- Plasma cholinesterase
- Paraoxygenase
- PON1
- Neurotoxic esterase
- Organophosphate-induced delayed neuropathy
- OPIDN
- Seizures
- Miosis
- Intermediate syndrome
- Delayed neuropathy
- Pyridostigmine
- Atropine
- Oximes
- Pralidoxime
- Hypochlorite
- Bleach
- Physostigmine
- Carbamates
- HI-6
- Obidoxime
- Diazepam
- Midazolam
- Seizures
- Propofol
- Gacyclidine
- Serum alkalization
- Sodium bicarbonate
- Magnesium
- Morphine
- Aminophylline
- Theophylline
- Succinylocholine
- Hemoperfusion
- Lipid emulsion
- Sulfur mustard
- MARK1
History of the Use of Nerve Agents
Nerve agents are organophosphate (OP) compounds, similar to OP pesticides, and are a group of potentially lethal chemical warfare agents (CWA). They are extremely potent inhibitors of the enzyme acetylcholinesterase (AChE) , a key regulator of cholinergic neurotransmission. Early attempts in the synthesis of OP were made by Von Hofman, who developed methylphosphor chloride in 1873. Michaelis in 1903 introduced a compound with P – CN bond, which led to the synthesis of many OP compounds, including the nerve agent tabun. Lang and Von Kreuger synthesized compounds with P – F linkage in 1932. Schrader developed sarin and tabun in 1937; in 1944, Germans developed soman. British scientists developed VX in 1952 [1].
Exposure of nerve agents to humans was restricted to one prospective study with VX and sarin and to case reports of treatment of accidental exposure to sarin and soman [2]. The first reported use of nerve agents in a war occurred in February 1984 in Majnoon Island, by the Iraqi army against the Iranian troops. The nerve agent tabun was found in the environmental samples and in the postmortem examination of the patients who died soon after exposure. More than 300 patients died within 30 min of exposure in the field, and several thousands were poisoned by tabun [3]. Toxicologic analyses of the blood, urine, skin, and gastric juice of the chemical war gas victims revealed tabun and sulfur mustard [4]. Later in 1987 and 1988, particularly during the Halabjah massacre, another nerve agent (sarin) also was identified [5].
A presumed terrorist attack with sarin occurred in a residential area of the city of Matsumoto , Japan, on June 27, 1994. About 600 residents and rescue staff were poisoned; 58 were admitted to hospitals, and 7 died [6]. On March 20, 1995, terrorists released sarin at several points in the Tokyo subway, killing 11 and poisoning more than 5500 people [7]. United Nation has confirmed that sarin was used on 21 August 2013 in Ghouta area of Damascus, Syria [8].
Relevant Chemistry
Nerve agents are divided into two groups of G (comes from Germany) and V (abbreviated from Victory, as the British who first synthesized after the World War I victory, named it) agents. The G agents (except for tabun, which is a cyanide derivative) are fluorinated OP compounds. The V agents are sulfur-containing OP compounds. The principal G agents, GA, GB, and GD, have the common names of tabun, sarin, and soman, respectively. The other G agents and V agents do not have common names. The oldest and most common V agent is called VX. The names and chemical structures of all nerve agents are summarized in Table 1.
Although both G and V agents are commonly called nerve gases, they exist under temperate conditions as clear, colorless, viscous liquids with high boiling points. They become aerosolized when dispersed by spraying or by an explosive blast from a shell or bomb. The G agents are only moderately volatile (vapor pressure of <2 mmHg at 20 °C), but owing to their great toxicity, the vapors pose a significant inhalational hazard . Vapor pressure of the G agents is sufficiently high for the vapor to be disseminated rapidly. GB (sarin) is mainly a vapor hazard. VX is less volatile and is normally a liquid contact hazard. Delivery systems of nerve agents include bombs, missiles, cluster spray, and spray tanks. G agents spread rapidly on surfaces such as skin and in the lungs. They are dispersed within hours and are described as nonpersistent agents, whereas VX spreads slowly and remains in the place for weeks or longer after exposure and is thus called a persistent nerve agent. Clothing releases G agents for about 30 min after contact with vapor [9]. If G agents are released into the air, they are degraded rapidly by reaction with photochemically produced hydroxyl radicals and have an estimated half-life of 10 h.
Nerve agents are four to six times more dense than air. As a result, they tend to remain close to the ground and pose a risk particularly to people in low areas and below-ground shelters. The nerve agents are soluble in water, organic solvents, and fat. After contact with water, they are hydrolyzed to products that are less toxic than the parent compounds [10].
Pathophysiology
Mechanism of Action
The well-known mechanism of action of OP compounds is the inhibition of cholinesterases. Two types of cholinesterase are involved:
-
1.
AChE is a specific enzyme useful for the diagnosis of OP poisoning; it also is called true cholinesterase. It usually is estimated in red blood cells and called RBC AChE or erythrocyte AChE.
-
2.
Butyrylcholinesterase (BChE) is less specific but more sensitive than AChE for the diagnosis of OP poisoning. It also is called pseudocholinesterase . BChE is usually estimated in plasma and is so-called plasma cholinesterase .
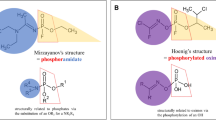
The reaction between OP compounds and AChE occurs in three steps, as shown in Fig. 1 [10]. The toxic manifestations and lethality after nerve agent exposure seem to follow the irreversible phosphorylation of the serine-containing active site of AChE. BChE also is inhibited. People with BChE genetic variation deficiencies may be at risk. The clinically most important variant is atypical (D70G) BChE because people with this variation have 2 h of apnea after receiving a dose of succinylcholine that is intended to paralyze muscle for 3–5 min [11].
Three-step reaction mechanism for the inactivation of acetylcholinesterase (AChE) by an organophosphate compound. Step 1 depicts the formation of a reversible complex between a serine residue in the AChE active site and the organophosphate. Step 2 shows the elimination of the organophosphate leaving group (X−). In step 3, the aging of the AChE is completed, forming a phosphorylated AChE
Different aging mechanisms are involved. Tabun and butyl-tabun seem to be accommodated similarly in the active center, as suggested by molecular modeling via kinetic studies of phosphorylation and aging with a series of HuAChE mutants (E202Q, F338A, F295A, F297A, and F295L/F297V) [12]. A variety of proteolytic enzymes (e.g., chymotrypsin, trypsin) also may be inhibited by OP nerve agents. Soman and sarin are detoxified in part via a two-step pathway involving bioactivation of the parent compound by the cytochrome P-450 system, then hydrolysis of the resulting oxygenating metabolite (oxon) by serum and liver paraoxygenase (PON1) . Serum PON1 has been shown to be polymorphic in humans [13].
Biochemical Changes
Acetylcholine accumulation is involved in the calcium flux into skeletal muscle fibers during OP poisoning [14]. Bright and coworkers (1990) [15] reported a histochemical demonstration of sarin-induced calcium influx in mouse diaphragm, which may be linked with OP-induced myopathy. Sarin may induce myonecrosis. Significant increase in alkaline phosphatase and creatine phosphokinase activity and minor changes in coagulation parameters (prothrombin time, activated partial thromboplastin time, fibrinogen) were observed after soman poisoning in rabbits [16]. Significant increases in creatine phosphokinase, lactate dehydrogenase, alanine aminotransferase, aspartate aminotransferase, and serum potassium, associated with damage to striated muscle and metabolic acidosis, occurred 2 days after GF poisoning in 20 male rhesus monkeys [17].
Toxicity
The vapor pressure of the three G agents (GA, GB, and GD) makes them significant inhalational hazards, especially at warmer temperatures or when droplets are created by explosion or spray. Based on information from animal studies, the lethal inhaled dose of G agents in humans may be about 1 mg. The G agents also represent a skin contact hazard, particularly when evaporation is minimized and contact is prolonged by contamination of clothing. The percutaneous absorption of G agents is much less rapid and complete, however, than the inhalational form [9].
VX does not pose a major inhalational hazard under usual circumstances, but it is well absorbed through the skin [9]. The relative lethality as determined in animal studies is VX > soman > sarin > tabun [18]. Acute toxic values of nerve agents in humans are summarized in Table 2.
The acute toxicity of nerve agents is due primarily to irreversible inactivation of AChE leading to an accumulation of toxic levels of acetylcholine. Similar to other OP compounds, these agents act by binding to a serine residue at the active site of a cholinesterase molecule, forming a phosphorylated protein that is inactive and incapable of breaking down acetylcholine. The stable phosphoryl enzyme complex can undergo one of two possible processes: a. Reactivation: The use of an appropriate nucleophile can trigger hydrolysis of the phosphoryl enzyme which can lead to reactivation of the enzyme [19].
b. Aging: Cleavage of the PO-C bond of the phosphorylated protein and the subsequent release of an alkyl carbenium ion is a process that is referred to as aging. In this case, the enzyme can no longer be reactivated even with the aid of a nucleophile.
In addition to the classical definition of aging of AChE described above, other definitions have also been proposed. One example involves the breakage of the P-N bond (as opposed to the PO-C bond) [12].
The reactivation of the aged AChE in many cases is not feasible, and the inhibition of the enzyme is considered irreversible. This is in part due to the negative charge at the active site of the enzyme, which makes any nucleophilic attack difficult [20].
The accumulation of toxic levels of acetylcholine at the synapse initially stimulates, then paralyzes cholinergic synaptic transmission (Fig. 2). Cholinergic synapses are found in the central nervous system, at the termination of somatic nerves, in the ganglionic synapses of autonomic nerves, and at the parasynaptic nerve endings, such as those in the sweat glands [10].
Cholinergic signaling in neurons and bronchial epithelial cells. (a) In neurons, choline for ACh synthesis is transported by the choline high-affinity transporter (CHT1). ACh is then synthesized by the action of choline acetyltransferase (ChAT) and packaged into synaptic vesicles by the action of the vesicular acetylcholine transporter (VAChT) and CHT1. ACh is then secreted by the complex processes that control synaptic release. Released ACh then interacts with postsynaptic nAChR and mAChR as well as presynaptic receptors. Signaling is terminated by acetylcholinesterase (AChE) and butyrylcholinesterase (BChE). Key signal transduction events lead to the generation of action potentials, opening of membrane and internal ion channels, muscle contraction, and kinase activation. (b) In bronchial epithelial cells (BEC), though CHT1 is present, CHT1 does not appear necessary for choline transport for ACh synthesis. In BEC, as for neurons, ChAT is utilized for ACh synthesis, though since there are multiple isoforms of ChAT, different splicing products may be utilized in different cell types. Since CHT1 is not required, and BEC do not have synaptic vesicles, the role of VAChT and CHT1 in ACh secretion is unknown, though both are expressed in BEC. ACh released by BEC is inactivated by the same cholinesterases as expressed in neurons. A key difference is that released ACh is not limited just to synaptic communication, but can also signal multiple neighboring cells as a paracrine factor or more distal cells as a hormone (From Muscarinic Receptors: Handbook of Experimental Pharmacology 208, 2012. Fryer AD, Christopoulos A, and Nathanson NM, eds, Springer, with permission)
The rate of aging varies greatly among the nerve agents. The half-time of aging is within minutes after soman exposure, about 5 h after sarin exposure, and more than 40 h after exposure to tabun and VX [18].
OP compounds also bind to other esterases and cholinergic receptors. Inactivation of neurotoxin esterase by some OP pesticides can lead to delayed peripheral naturopathic effects known as organophosphate-induced delayed neuropathy (OPIDN). At many times the median lethal dose (LD50), the nerve agents inhibit neurotoxin esterase to some extent, although the activity of VX is much less than that of G agents [21]. Possible involvement of neurotrophic factor (growth-related enzyme ornithine decarboxylase) during early stages of OPIDN , particularly after diisopropylfluorophosphate, has been reported [22]. Nerve agents also bind quickly to cardiac muscarinic (M2) receptors at higher than physiologic concentrations, but whether this contributes to cardiac toxicity is unknown [23]. They also interact with the nicotinic acetylcholine receptor–ion channel complexes, but only at tissue concentrations of 10–100 times greater than the concentrations fully inhibiting AChE. Sarin, soman, and tabun are partial agonists of these channel complexes, whereas VX acts as an antagonist [24]. There also is evidence that nerve agents affect noncholinergic mechanisms in the central nervous system at a dose approaching LD50 [25]. Antagonistic effects of γ-aminobutyric acid (GABA)–ergic systems may explain convulsive activity after OP poisoning. Effects of soman and tabun on the uptake and release of GABA and glutamate in the synaptosomes of guinea pig cerebral cortex did not support the previous belief that nerve agents cause convulsions by affecting the uptake or release of GABA or glutamine. Indirect evidence that soman and tabun inhibit catabolism of GABA and glutamine was obtained, however [26].
Acute exposure to tabun, sarin, or soman increases brain levels of cyclic adenosine monophosphate and decreases cyclic guanosine monophosphate as a result of stimulation of adenylyl cyclase and phosphodiesterase systems [6, 27]. VX at concentration of 10 μM produced a significant reduction in cell metabolism within 2 min as measured by changes in the acidification rate of medium culture after 4 h of exposure. Two alkali degradation products of VX produced no cytotoxicity [28].
Toxicokinetics
As the OP nerve agents are lipophilic, they are absorbed rapidly following inhalation or ingestion. Dermal absorption is slow, but severe poisoning may still ensue if exposure is prolonged. Following absorption, OP nerve agents accumulate in fat, liver, kidneys, and salivary glands. Shih and co-workers (1994) studied toxicokinetics of GB, GD, and GF in rats. They had collected urine, blood, and lung tissue from rats dosed subcutaneously at 75 μg kg−1. Urinary excretion of the metabolite was the major elimination route for these three nerve agents. The major differences between them were primarily the extent and rate of excretion. Alkylmethylphosphonic acid is the single major metabolite formed and excreted in urine by a nonsaturable mechanism. Nearly total recoveries of the given doses for GB and GF in metabolite form were obtained from the urine. The terminal elimination half-lives in urine were 3.7x ± 0.1 and 9.9 ± 0.8 h for GB and GF, respectively. GD metabolite showed a biphasic elimination curve with terminal half-lives of 18.5 ± 2.7 and 3.6 ± 2.2 h. GD was excreted at a slower rate with a recovery of only 62%. Lung was the major organ of accumulation for this nerve agent. The toxic G agents were concentrated more in red blood cells than in plasma [29].
The metabolism of nerve agents results in the formation of inactive phosphonic acids, which are excreted via kidneys [30–32]. Experimental studies reveal that the elimination half-life of G agents was less than 1 h which is shorter than VX, which persists for several hours following intravenous administration and even longer after percutaneous exposure [33].
Oxidation and hydrolysis are principal metabolic inactivation pathways, which occur mainly by reaction with glutathione and also by glucuronidation and demethylation. Tabun causes the largest number of degradation products among the G agents. Detoxification of tabun takes place slowly, by di-isopropyl-fluorophosphatase, formerly termed tabunase. There are sparse toxicity data available for the subset of tabun degradation products. Ethyl-dimethylaminophosphoric acid is the main product of tabun dimethylamine, which is also produced by hydrolysis of tabun. Dimethylamine causes human irritation in the respiratory tracts [34].
Isopropyl-methylphosphonic acid (IMPA) is a metabolite of sarin which subsequently hydrolyses to the high stable methylphosphonic acid (MPA) which mildly irritates rabbit skin and human skin and eyes [35].
In rats, 10 min after intravenous sarin, around 70% of the plasma was bound to large protein molecules similar to carboxylesterase [36]. The toxicity of sarin enhanced 6–8 times when the rats were pretreated with triorthocresyl phosphate, which is a weak anti-ChE OP with irreversible blocking carboxylesterase activity [37].
In a report of Little et al. (1986) who injected 80 μg/kg of sarin intravenously to mice, sarin concentration was at the highest in the kidney, liver, and plasma within one minute. Over the first minute, about half of the labeled sarin was associated with the major sarin metabolite; IMPA and the kidneys contained the highest concentration of sarin and its metabolites. Much lower hepatic concentrations after 24 h suggest a primary role of the kidneys in detoxification of sarin [38]. In another experiment of Little et al. (1988) with the same method, hypothalamus contained concentrations of both sarin and the metabolites 2–5 times greater than those in other brain areas. This finding suggests that the hypothalamus is more important with respect to central effects of nerve agents [39]. In 4 of 12 patients of Matsumoto with sarin exposure who underwent the study, the levels of IMPA and MPA correlated with clinical manifestations [40].
Pinacolyl methylphosphonic acid is the predominant hydrolytic product of soman [41].
A two-compartment model, with a biologic half-life of 1–1.5 min, described toxicokinetics of the four stereoisomers of soman in atropinized rats. The extremely toxic C(±) P(−) isomers could be followed in rat blood samples for more than 4 and 2 h at doses of 6 and 3 LD50 (82 μg/kg). The toxicokinetics of P(−) isomers was described with a three-compartment model, with terminal half-lives of 40–64 min and 16–22 min at doses of 6 and 3 LD50, respectively [41].
Clinical Presentation and Complications
The nerve agents cause toxic effects mainly by interfering with cholinergic synaptic function. This effect occurs at cholinergic neuroeffector functions (muscarinic effects), at the skeletal myoneural junctions and autonomic ganglia (nicotinic effects), and in the central nervous system. The signs and symptoms of nerve agent poisoning are classified according to whether they are due to overstimulation of muscarinic, nicotinic, or central nervous system receptors [42–53]. Nerve agents also cause long term and late complications [54–57].
Muscarinic effects of acetylcholine stimulation include miosis ; blurred vision; eye pain; hypersecretion by salivary, sweat, lachrymal, and bronchial glands; bronchoconstriction; cough; cyanosis; pulmonary edema; nausea; vomiting; diarrhea; crampy abdominal pains; tenesmus; urinary and fecal incontinence; hypotension; and bradycardia (see Chap. 23, “Anticholinergic Syndrome”). Nicotinic effects include easy fatigue, weakness, muscle cramping, fasciculations, skeletal muscle twitching, convulsions, and flaccid paralysis. Nicotinic stimulation also can obscure muscarinic parasympathetic effects and produce mydriasis, tachycardia, and hypertension by stimulation of the adrenal medulla. Central nervous system effects include irritability; nervousness; giddiness; ataxia; fatigue; generalized weakness; depression of respiratory and circulatory centers with dyspnea, cyanosis, hypoventilation, and hypotension; lethargy; impairment of memory; confusion; convulsions; coma; and respiratory depression [6, 7, 10, 42, 51–53]. The main toxic effects of nerve agents at various sites in the body are summarized in Table 3.
Clinical Manifestations by Routes of Exposure
The effects of nerve agent exposure occur via inhalation, contact with skin and the eyes, and, rarely, ingestion. Most often, exposure is to vapor (inhalation) or liquid (percutaneous). After small-to-moderate doses, initial effects and their time of onset are determined by the route of exposure [47, 58–63]. In contrast, large doses cause similar effects by all exposure routes, although the time of onset varies [10]. Gastrointestinal absorption rarely may occur through ingestion of contaminated food.
Inhalation
Exposure to low vapor concentrations may affect only the eyes, nose, and airways. Miosis, visual disturbances, rhinorrhea, and some degree of dyspnea develop within seconds to several minutes. The severity of dyspnea is dose dependent. Usually, these effects do not progress significantly when the patient is removed from contamination. After inhalation of high vapor concentrations, victims lose consciousness within 1 or 2 min, then have seizures, flaccid paralysis, and apnea. Other early effects of high vapor concentrations include miosis and copious secretions. Involuntary micturition and defecation also may occur. Unless medical assistance is immediate, victims may die within 30 min [43–46].
Skin Absorption
Percutaneous absorption of nerve agents varies according to the body site exposed and the ambient temperature. VX was absorbed nearly eight times more rapidly from facial skin than it was from the volar forearm, and absorption increased markedly as surrounding temperature increased from 18 °C to 46 °C [27]. Initial local effects of liquid, which seldom are noticed, include muscular fasciculations and sweating at the contamination site. A large droplet also may cause gastrointestinal effects and complaints of malaise and weakness. Droplets containing near-lethal or lethal doses cause loss of consciousness, seizures, flaccid paralysis, and apnea. The onset of these effects is sudden, usually after a symptomatic interval of 10–30 min [10, 42].
Eyes
Miosis rapidly occurs after splash exposure or eye contact with vapor and later, if at all, after systemic poisoning. Unilateral miosis can occur if only one eye has been exposed. Miosis may be accompanied by deep aching eye pain, conjunctival irritation, and visual disturbances. Dim vision may be due to constricted pupils or inhalation of cholinergic fibers of the retina or central nervous system. The miotic pupil may improve vision (the pinhole effect), although complaints of blurred vision are common [58]. Direct installation of diluted nerve agent into the eyes does not produce tissue damage [10].
Life-Threatening Complications
The most life-threatening complication is respiratory failure, which is due mainly to the effect of the nerve agents on the central nervous system [59, 60], although in one animal experiment with sarin, respiratory paralysis could be purely central, peripheral, or both, depending on the doses of sarin and atropine antidote employed [61]. Hypoxia also is a major problem in the nerve agent poisoning, as it may cause cerebral edema and convulsions and may induce histopathologic brain damage.
Cardiovascular complications sometimes are severe and life-threatening [47, 62] (See Figs. 3 and 4). The nerve agents tabun, sarin, soman, or VX at 5–10 times the LD50 administered to guinea pigs induced circulatory arrest a few minutes after apnea in nontreated animals. Antidote treatment by atropine (10 mg/kg) and HI-6 or HLo-7 (30 mg/kg) 2 min later rapidly restored heart rate and arterial pressure and respiratory function to various degrees. The nerve agent injection caused marked sinus bradycardia and a subsequent complete atrioventricular block within 1–2 min . In guinea pigs with depressed respiratory function (<50%), intermittent ST-T wave alterations and second-degree atrioventricular heart block were observed [47]. Other reported electrocardiogram abnormalities in animal experiments and in humans exposed to nerve agents include torsades de pointes, atria fibrillation, idioventricular dysrhythmias, complete heart block, and ventricular fibrillation [6, 10, 47, 62]. Histopathologic changes compatible with toxic myocarditis were observed after sarin and soman in animal experiments [47], but myocarditis has not been reported in humans.
Muscarinic signaling pathways in supraventricular (sinoatrial, atrial, and atrioventricular) myocytes. Acetylcholine (ACh) acts through M2 receptors to regulate ACh-activated K channels via a membrane-delimited mechanism involving direct activation by the bg subunits of the inhibitory G protein Gi. ACh also acts through M2 receptors to inhibit adenylyl cyclase (AC) activity via the a subunit (ai) of Gi, resulting in a decrease in cAMP production. This may occur in the absence or presence of agonists that stimulate cAMP production. Norepinephrine (NEPi) acts through b1-adrenergic receptors to stimulate cAMP synthesis by directly activating all isoforms of adenylyl cyclase (AC) via the a subunit (as) of the stimulatory G protein Gs. Changes in cAMP affect targets of protein kinase A (PKA)-dependent phosphorylation such as troponin I (TnI), phospholamban (PLN), and the L-type Ca2þ channel. Changes in cAMP also directly regulate pacemaker channels, which are permeable to both Na and K (From Muscarinic Receptors: Handbook of Experimental Pharmacology 208, 2012. Fryer AD, Christopoulos A, and Nathanson NM, eds, Springer, with permission)
Muscarinic signaling pathways in ventricular myocytes. Responses to M2 receptor activation are only observed in the presence of agonists that stimulate cAMP production. Norepinephrine (NEPi) acts through b1-adrenergic receptors to stimulate cAMP synthesis by directly activating all isoforms of adenylyl cyclase (AC) via the a subunit (as) of the stimulatory G protein Gs. Acetylcholine (ACh) acts through M2 receptors to inhibit AC5/6 activity via the a subunit (ai) of the inhibitory G protein Gi. ACh acting through M2 receptors can also stimulate AC4/7 activity via the bg subunits of Gi. Changes in cAMP affect targets of protein kinase A (PKA)-dependent phosphorylation such as troponin I (TnI), phospholamban (PLN), as well as L-type Ca2+, delayed rectifier K+, and CFTR Cl− channels (From Muscarinic Receptors: Handbook of Experimental Pharmacology 208, 2012. Fryer AD, Christopoulos A, and Nathanson NM, eds, Springer, with permission)
Intermediate Syndrome
The intermediate syndrome consists of marked weakness of the proximal skeletal musculature (including the muscles of respiration) and cranial nerve palsies that occurs 1–4 days after acute poisoning. This syndrome, which was observed after certain OP pesticides poisoning [63], has not been reported yet after OP nerve agent poisoning. Intermediate syndrome may be a consequence of cholinergic overactivity at the neuromuscular junction, and a connection has been made between the intermediate syndrome and OP-induced myopathy or undertreatment. Myopathy has been observed histologically in experimental animals with the nerve agents tabun, soman, and sarin [14, 15]. It can be anticipated that the intermediate syndrome occurs in some cases of nerve agent poisoning (Fig. 5).
Delayed Neuropathy
Organophosphorus pesticides-induced delayed neuropathy is a symmetric sensorimotor axonopathy, tending to be most severe in long axons and occurring 7–14 days after exposure. In severe cases, it is an extremely disabling condition [64]. Inhibition of neuropathy target esterase seems to be necessary for OPIDN to develop. Other mechanisms may be involved, however. The trophic factor ornithine decarboxylase, a growth-related enzyme, was decreased in the spinal cord after the naturopathic agent diisopropylfluorophosphate [22]. Although OPIDN was not observed after nerve agent poisoning in experimental studies [65, 66] and in accidental nerve agent poisoning, a case of sensory polyneuropathy 7 months after sarin poisoning has been reported [67].
Temporary psychological effects, such as depression, fatigue, insomnia, irritability, nervousness, and impairment of memory, have been described after nerve agent exposure [57]. Electroencephalography in a person who was severely intoxicated with sarin showed marked slowing with bursts of high-voltage waves at a rate of five per second [42]. Epileptic-type changes of the electroencephalography were observed after sarin poisoning 11 months after exposure [6].
Course and Prognosis
Victims with heavy exposure to nerve agents may die within a few minutes in the field. Persons with physical and chemical protection (pyridostigmine) who remain in a heavily contaminated area may become intoxicated after 30 min. A patient with moderate-to-severe intoxication who receives first aid and emergency medical treatment may survive for a few days to a few weeks, according to the severity of intoxication and type of treatment [44]. Death, however, is common.
Hypoxia, coma, convulsions, and respiratory failure are signs of a poor prognosis. Patients who remain severely hypoxic and cyanotic may develop cardiac arrhythmias and die quickly. Patients who develop apnea and do not receive assisted ventilation immediately may incur brain damage and either die or become vegetative. It is unlikely that nerve agents possess the potential to give rise to OPIDN [45].
Soldiers who are caught unaware and who are exposed to large amounts of nerve agent before donning respirators and other protective clothing and who rapidly develop severe symptoms and signs are unlikely to survive. Soldiers who rapidly develop respiratory failure and who become incapable of self-administrating their own autoinjector devices also have a poor prognosis, unless emergency medical treatment is provided rapidly [44]
Late Complications
The nerve agents are less likely to cause chronic diseases in comparison with sulfur mustard poisoning . However, hypoxic encephalopathy is reported as one of the most remarkable long-term neurologic toxic effects of the nerve agents [46]. Cardiomyopathy has been reported in soman and sarin intoxicated rats, which may be a cause of death; however, it is not reported in human cases yet [47]. Neurological assessment of 43 Iranian veterans 22–27 years post exposure revealed fatigue, paraesthesia, and headache as the most common symptoms and sensory nerve impairments as the most common observed clinical complication in the Iranian veterans with the nerve agents of tabun and sarin. Sensory nerve dysfunction is more prevalent than motor nerves, which predominantly was a distal sensory deficit [48].
Engel et al. (2004) reported fatigue, depression, and chronic pain as the common clinical presentations of “Gulf war syndrome” [49]. Electroencephalogram (EEG) studies on sarin patients showed significant slowing with bursts of high voltage waves at a rate of five per second on EEG, 11 months after the exposure [50, 51]. Asthenia, insomnia, fatigue, blurred vision, narrowing of the visual field, shoulder stiffness, slight fever, and asthenia were observed in patients who exposed to sarin 1 and 3 years after Tokyo subway explosion [52]. Fullerton and co-authors (1990) on a review of article mentioned temporary psychological effects such as depression, insomnia, fatigue, nervousness, irritability, and memory impairment as long-term complication of exposure to NAs [53]. Page (2003) on a telephone survey of 4,022 sarin exposed patients 28 years post exposure reported poor concentration abilities and sleep disturbances in comparison with the controls [54]. Grauer et al. (2008) have studied late neuronal and behavioral deficit after sarin exposure in rats. The data showed long lasting impairment of brain function after single sarin exposure that developed with time [55]. There is no real evidence on carcinogenicity, mutagenicity, and teratogenicity of NAs [56, 57].
Diagnostic Considerations
Initial diagnosis of nerve agent poisoning can be made based on the exposure history (accidental, terrorism, chemical warfare attack) and clinical manifestations. In low-level exposure, the route of absorption may affect the clinical features, but in high-level exposure, severe intoxication occurs. Absorption is faster through inhalation than by skin contact. Estimation of AChE in erythrocytes is required to confirm the anticholinesterase diagnosis and to estimate the severity of intoxication. BChE estimation also may help, although it is not specific and may be low due to genetic variations [11].
Diagnostic certainty of nerve agent exposure requires toxicologic analyses of the environment, blood sampling, or both. A biosensor, which is a potentiometer enzyme electrode for direct determination of OP nerve agent, has been developed [68].
A fiberoptic enzyme biosensor for the direct measurement of OP nerve agents has been developed. Concentrations of 2 μM can be measured in less than 2 min using the kinetic response. When stored in buffer at 4 °C, the biosensor shows long-term stability [69]. A new method for retrospective detection of exposure to OP nerve agents was applied to estimate serum sarin concentrations of the Matsumoto incident. The concentrations ranged from 0.2 to 4.1 ng/mL in serum [70]. Definitive evidence for the acute sarin poisoning of the Tokyo subway was obtained by detecting sarin-hydrolyzed products from erythrocytes of four victims in postmortem examinations [71].
Intravenous administration of atropine can be used as a diagnostic test for anticholinesterase poisoning, whereas oximes are used only for treatment [72]. Cholinesterase activity in postmortem blood as a screening test for OP nerve agent exposure was performed in 53 nonpreserved postmortem whole-blood specimens. There was a negligible loss of cholinesterase activity by the 7th day of the study. Cholinesterase activity could be applied as the screening test for anticholinesterase nerve agents [73].
Diagnosis of the delayed neurotoxin effects can be made by estimation of neuropathy target esterase, although it is unlikely to occur after nerve agent poisoning. Marked reduction of neurotrophic factor (ornithine decarboxylase) during the early stages of neurotoxicity also may be helpful when it is possible to perform it [22]. Measurement of nerve conduction velocity and electromyography may be useful for the diagnosis of the delayed neuropathy of OP nerve agents [74].
Toxicologic Analyses
Cholinesterases and Neuropathy Target Esterase Determination
Estimation of BChE in plasma is widely available and should be performed as soon as possible. Erythrocyte AChE is more specific, however, and has more quantitative value than BChE, although both enzymes usually are measured spectrophotometrically. Inhibition of greater than 50% activity of either enzyme confirms the diagnosis of an anticholinesterase poisoning. Reactivation of BChE is relatively more rapid, depending on the agent, severity of intoxication, and use of oximes, taking 1–4 weeks. In contrast, reactivation of AChE may take up to 3 months [6]. Neuropathy target esterase shall also be estimated when there are clinical features of delayed neuropathy.
Nerve Agent Detection
Detection and estimation of nerve agents are easier in environmental samples than in blood and urine samples of patients. By using new technology, such as biosensors and fiberoptic bioenzyme, and new methods for detection and determination of nerve agents (e.g., sarin) in the serum and erythrocytes, identification and estimation of common nerve agents are possible [68–72, 75].
Oxime Estimation
Estimation of pralidoxime concentration in blood may be required, although it is not necessary for the routine management of the patient. To achieve a maximal therapeutic effect, however, a blood pralidoxime concentration of 4 mg/L should be reached. An obidoxime plasma level in the range of 10–20 μM was estimated as appropriate. This was achieved in 34 severely OP-poisoned patients using regimen of 250 mg i.v. as bolus, followed by 750 mg/24 h and was maintained as long as reactivation was possible. The result confirmed using this definite regimen for adults [75].
Biochemical and Hematologic Analyses
Acid–base and electrolyte disturbances are common during severe nerve agent poisoning. Arterial blood gas analysis, estimation of serum electrolytes, liver and kidney function tests, amylase, creatine phosphokinase, and lactate dehydrogenase may be required for patient management. Hypokalemia and hyperglycemia are common and should be considered and corrected. Elevation of serum amylase may reveal acute pancreatitis. Transient elevation of liver enzymes, hematuria, leukocyturia, and proteinuria may be observed during nerve agent poisoning. Blood cell count and other hematologic tests may be performed as clinically indicated. Transient leukocytosis, particularly in polymorphonuclear neutrophils, may be observed during severe nerve agent poisoning [45].
Other Investigations
Chest x-ray, electrocardiogram, electroencephalogram, electromyogram, nerve conduction velocity, spirometry, computed tomography, magnetic resonance imaging, and other investigations may be performed in nerve agent poisoning as clinically indicated [44].
Severity Grading of Intoxication
Severity grading of nerve agent poisoning can be done based on clinical manifestations, cholinesterase activity, and initial atropine dose required for atropinization.
Clinical Symptoms and Signs
Patients with OP nerve agent poisoning can be divided into four groups – mild, moderate, severe, and fatal – according to symptoms and signs of poisoning (Table 4).
Inhibition of Cholinesterases
Patients with nerve agent poisoning may be divided into three groups according to cholinesterase activities (Table 5).
Atropine Dose
Patients with OP nerve agent poisoning can be divided into three groups according to the initial atropine dose required for atropinization:
-
1.
Mild: less than 2 mg
-
2.
Moderate: 2–10 mg
-
3.
Severe: greater than 10 mg [45]
Causes of Death
Death after nerve agent exposure is mainly due to respiratory failure resulting from depression of the respiratory center, paralysis of respiratory muscles, and obstruction caused by bronchospasm and bronchial secretions. Some animal studies suggest that lack of central drive is the major factor [59, 60]. Cardiomyopathy in soman-intoxicated and sarin-intoxicated rats has been reported [34] and may be a contributory cause of death.
Status epilepticus occurred in animals after high doses of sarin, soman, or VX despite early treatment with atropine and pralidoxime. Prolonged seizures may cause anoxia and morphologic brain damage, which induces more morbidity and mortality [65, 66].
Treatment
Priorities
The first rule for managing chemical casualties is that the emergency responders must protect themselves from contamination, resulting from contact with casualties and the environment (Fig. 2). This can be done by wearing personal protective equipment or by thoroughly decontaminating the patient. At minimum, rescuers should wear a protective mask (or mask containing a charcoal filter for a self-contained breathing apparatus device, not a surgical or similar mask) and heavy rubber gloves (surgical gloves offer negligible protection) and avoid skin contact with victims until decontamination has been carried out [9, 76].
As soon as possible, victims should be removed from the contaminated place and decontamination must be initiated. Antidotes should be given at the onset of effects as appropriate (e.g., autoinjector containing atropine, obidoxime, and diazepam). For unconscious or severely intoxicated patients, priorities must follow the ABCs (airway, breathing, and circulation) of resuscitation. Oxygen administration and assisted ventilation should be undertaken as soon as possible in patients with respiratory distress. Because atropine reverses bronchoconstriction within minutes, one could hesitate to intubate a dyspneic, conscious patient who is likely to improve quickly. In a severely poisoned, unconscious, apneic patient, however, endotracheal intubation with assisted ventilation should be undertaken as quickly as possible.
Airway resistance may be high initially, causing some mechanical ventilators to malfunction, but this should return to normal after atropine administration. Frequent airway suctioning may be required for copious bronchial secretions. Supplemental oxygen through an endotracheal tube with positive end-expiratory pressure is indicated for severely hypoxic patients. It is important to improve tissue oxygenation before atropine administration to minimize the risk of ventricular fibrillation. Advanced life support, including intravenous line placement, should be provided to all victims with evidence of respiratory compromise or other signs of severe exposure [10, 44].
Decontamination
Decontamination must be carried out at the earliest opportunity to limit skin absorption of the agent and prevent contamination of the rescuers. Thorough decontamination is essential before casualties enter an emergency department or other site of medical care to avoid contamination of staff and other patients.
Indications for ICU Admission in Nerve Agent Poisoning
-
1.
Patients with severe nerve agent intoxication (see section on “Severity Grading of Intoxication”), particularly patients with respiratory failure who need mechanical ventilation, should be admitted to the intensive care unit.
-
2.
Although intermediate syndrome has not clearly been reported in nerve agent poisoning, it may occur in some cases. Patients with moderate-to-severe intoxication even without assisted ventilation should be monitored, preferably in the intensive care unit, for treatment of possible sudden respiratory arrest due to muscle paralysis.
If the eyes have been exposed, they should be irrigated as soon as possible with running water or saline. Skin should be decontaminated by pouring on large amounts of a chlorine-liberated solution, such as 5% hypochlorite solution (household bleach), followed by copious water rinsing. If bleach is not available, the skin should be blotted gently (without rubbing) with generous amounts of alkaline soap and water followed by a water rinse. Generous amounts of water alone can be used if nothing else is available. Water dilutes and physically washes away the nerve agents, but it does not hydrolyze them. Contaminated clothing and jewelry should be removed, and the underlying skin should be decontaminated thoroughly. Care should be taken to clear under the nails, the intertriginous areas, the axillae, the groin, and the hair [10, 45].
Experimental Antidotes
Fetal bovine serum AChE protected mice from multiple LD50 doses of OP nerve agents [77]. BChE purified from human plasma also was effective in vitro and in vivo in mice and rats as a single prophylactic antidote against the lethal effects of nerve agents [78]. Addition of the oxime HI-6 to fetal bovine serum and AChE as a pretreatment drug amplified the efficacy of enzyme as a scavenger of nerve agents [79].
Recombinant DNA–derived AChEs showed a great improvement over wild-type AChEs as bioscavengers; they can be used to develop effective methods for the safe disposal and storage of OP nerve agents and are potential candidates for preexposure or postexposure treatment for OP toxicity [80]. By the use of cell immobilization technology, immobilized Escherichia coli with surface-expressed organophosphorus hydrolase was made to detoxify nerve agents [81]. By protein engineering techniques, one BChE mutant, G117H, was made to hydrolyze V and G agents, but it reacted much too slowly [82].
OP acid hydrolyses from two species of Alteromonas were cloned and sequenced to detoxify G agents, which was effective [83]. Cholinesterases that are covalently linked to a polyurethane matrix can be used effectively to remove nerve agents from and decontaminate surface biologic areas (skin or wounds) or other areas (clothing or medical equipments) or the environment. These cholinesterases could protect medical personnel from secondary contamination while attending chemical casualties and civilians exposed to highly toxic nerve agents [84].
A reactive skin decontamination lotion active against classic nerve agents and sulfur mustard was developed. The inactivation process was time and agent dependent and related to the ratio of OP to reactive skin decontamination lotion [85].
Pretreatment
In animal studies, pretreatment with reversible carbamate AChE inhibitors, such as pyridostigmine and physostigmine, enhances the efficacy of postexposure treatment of soman exposure or soman poisoning with atropine and pralidoxime chloride and permits survival at higher agent challenges [86]. His protection apparently is due to the fact that the more lethal nerve agents cannot attack AChE molecules bound by carbamates. Carbamylation of 20–40% of the erythrocyte AChE is associated with antidotal enhancement. Carbamate pretreatment does not reduce the effects of the agents and by themselves carbamates provide no benefit. Pretreatment is not effective against sarin and VX challenge and should not be considered a panacea for all nerve agents. It is of value for soman intoxication when agent challenge is followed by atropine and an oxime . Pretreatment is ineffective unless standard therapy is administered after the exposure .
Because physostigmine is toxic at the amounts required, pyridostigmine is the drug of choice for pretreatment (Grade III recommendation). The standard dosage is 30 mg orally every 8 h for impending nerve agent attack. Because pyridostigmine does not cross the blood–brain barrier, it causes no central nervous system toxicity of nerve agents. Carbamates must never be used after nerve agent exposure; in that setting, carbamate administration worsens, rather than protects from toxicity. Excessive doses cause many of the same toxic effects as do the nerve agents, and the recommended amounts caused annoying side effects in more than half of the population in a war zone. Eptastigmine treatment given intravenously protected mice better than physostigmine against soman exposure [87].
Pretreatment with a drug mixture (pyridostigmine, benactyzine, and trihexyphenidyl) and antidotal treatment (HI-6 and benactyzine) were investigated in rats. This cholinergic-anticholinergic pretreatment in restoring respiratory and circulatory changes induced by soman is important [88].
Antidotes
Available antidotes (atropine, oximes) do not prevent respiratory failure or incapacitation [89]. Early aggressive medical therapy with antidotes and intensive care management are the keys, however, to prevention of morbidity and mortality associated with nerve agent poisoning.
Atropine
Atropine should be titrated with the goal of drying secretions and resolving bronchoconstriction and bradycardia [90]. There is no actual dose for atropine. The dose (2 mg) of atropine available in an autoinjector is not adequate for moderate-to-severe exposure to nerve agents. Atropine should be given intravenously in doses to produce mild-to-moderate atropinization (dryness of tongue, oropharyngeal and bronchial tree, tachycardia, mydriasis, and flushing) as soon as possible. At least the same amount as the initial atropinization dose should be infused in 500 mL of dextrose 5% constantly to sustain the atropinization and should be repeated as needed until the patient becomes asymptomatic. Continuous infusion of atropine effectively antagonizes the muscarinic effects and some of the central nervous system effects of nerve agent poisoning, but it has no effect on skeletal muscle weakness, seizures, unconsciousness, or respiratory failure [10, 44]. Large doses of atropine require higher concentrations of atropine preparation (e.g., 100 mg/10 mL made in Germany) or at least a vast amount of atropine (10–100 mg) in dextrose 5% solution, ready-made for intravenous infusion in severely nerve agent–intoxicated patients. Much lower atropine doses are required for nerve agents than for the severe OP pesticides poisoning.
Atropine should not be given intravenously to a hypoxic patient. (Grade III recommendation) Hypoxia occurs as a result of hypersecretion in the respiratory tracts. The secretion must be suctioned and oxygen given to overcome hypoxia before inducing atropinization. If the patient is hypotensive, atropine can be given through an endotracheal tube or intratracheally for more rapid absorption through the peribronchial vessels [45]. Aerosolized atropine has also been used and can be administered quickly by inhalation. Studies suggest that in addition to the local effects in the lungs, it is absorbed systemically [91].
Oximes
Oximes are mainly pyridinium compounds, which are divided into mono-pyridium and bis-pyridium oximes. Common oximes used in the treatment of nerve agent poisoning are presented in Table 6. Although oximes have been designed to reactivate the inhibited AChE, clinical experience has indicated that they are not always effective as reactivators, and at this time, none of them can be regarded as a broad-spectrum antidote [92]. The choice of oximes based on the data presently available also may depend on factors other than protection against lethality, such as cost and availability of the oxime and its side effects. Obidoxime (Toxogonin, Merck, Germany) is likely to cause more toxic effects (hepatitis after high doses) than pralidoxime and HI-6 [93]. HI-6 is the least toxic, but it is less stable in solution and is not commercially available in many parts of the world.
Pralidoxime, HI-6, and HGG-12 were used in dogs with soman and tabun poisoning. Pralidoxime (in conjunction with atropine and diazepam ) showed the best protective effects in soman-poisoned dogs: The protective indices were 9 for pralidoxime, 6.3 for HI-6, and 3.5 for HGG-12. None of these agents was effective against tabun poisoning [94]. Efficacy of two other oximes, HLo-7 and pyrimidoxime (an analog of trimedoxime), in three times the LD50 of sarin, soman, and GF and two times the LD50 of tabun, was tested in mice. HLo-7 produced significant (P < 0.05) reactivation of phosphorylated AChE, resulting in 47%, 38%, 27%, and 10% reactivation of sarin-inhibited, GF-inhibited, soman-inhibited, and tabun-inhibited mouse diaphragm AChE, respectively [95]. In a comprehensive study, the order of effectiveness against soman was HI-6, HLo-7, and pyrimidoxime. HLo-7 was extremely effective against tabun poisoning, whereas HI-6 and pyrimidoxime were of moderate value. Against GF, HI-6 and HLo-7 were extremely effective, obidoxime was moderately effective, and pralidoxime and pyrimidoxime were least effective [96]. In soman-intoxicated guinea pigs, HI-6 was therapeutically slightly more effective than HLo-7; HLo-7 was more effective than HI-6 against tabun intoxication [97].
Pharmacokinetics and effects of HI-6 in blood and brain of soman-intoxicated rats were studied. High doses of HI-6 can reach the brain in sufficient amounts to reactivate inhibited brain AChE. Signs of soman poisoning correlated positively to AChE inhibition and negatively to the concentration of inbound HI-6 in the brain, and soman intoxication significantly decreased uptake of HI-6 into the brain [98]. Reactivating potency of obidoxime, pralidoxime, HI-6, and HLo-7 in human erythrocyte AChE inhibited by soman, sarin, cyclosarin, and VX was studied in vitro. After soman, sarin, cyclosarin, and VX inhibition, the reactivating potency decreased in the following order: HLo-7 > HI-6 > obidoxime > pralidoxime [99]. Dose–response effects of atropine and HI-6 treatment in soman and tabun poisonings were studied in guinea pigs. Atropine had a large effect on the efficacy of HI-6 against both the nerve agents. They also were more effective against soman than against tabun. Adjunctive treatment with diazepam enhanced the efficacy of HI-6 and atropine against soman [100]. The effects of common oximes in different nerve agent poisonings are summarized in Table 7.
Despite many oximes tested in animal experiments, the human experience in war or terrorism is limited to pralidoxime and obidoxime. Pralidoxime should be administered intravenously at a dose of 30 mg/kg initially over 30 min followed by a constant infusion of 8 mg/kg/h in dextrose 5%. Pralidoxime can be continued until full recovery or until atropine is required. Obidoxime was hepatotoxic at high recommended doses of 8 mg/kg initially and 3 mg/kg/h [5]. It may be given at a dose of not more than 500 mg initially and 750 mg/day. Liver function tests should be checked regularly during obidoxime therapy [45].
Diazepam
Behavioral efficacy of diazepam against nerve agents in rhesus monkeys was studied. The results showed that diazepam would be an excellent adjunct to traditional nerve agent therapy to facilitate behavioral recovery from nerve agent intoxication that might be encountered by medical military personnel on the battlefield [101]. Diazepam was the drug of choice for treatment of convulsions in nerve agents poisoning.(Grade III recommendation) The initial IV doses of 0.2–0.5 mg/kg in children and 5–10 mg in adults are recommended and may be repeated as required [102, 103].
Diazepam has not only symptomatic anticonvulsant effect but also has more specific effect on cholinergic and GABAergic systems [104]. In severe cases of nerve agents poisoning, convulsion starts within seconds after losing consciousness. It may persist for several minutes until the victim becomes flaccid and apneic. In these cases, diazepam must be administered promptly [103].
Other anticonvulsant benzodiazepines, such as lorazepam and midazolam, are effective in stopping seizures in acute nerve agents poisoning [105–108]. (Grade III evidence) Midazolam, however, is more potent and more rapid than diazepam in treatment of seizure in nerve agents poisoning. It is thus recommended that midazolam replace diazepam as an urgent anticonvulsant treatment for the nerve agents-induced seizures. (Grade III recommendation) Barbiturates, phenytoin, and other anticonvulsants are not effective against seizure in nerve agents poisoning [102]. Fast acting barbiturates may be effective, but they have more CNS depressive than the benzodiazepines. Propofol may be used in OP-induced grand mal convulsions if the response to benzodiazepines was not satisfactory.
Gacyclidine
Gacyclidine is an antiglutaminergic compound that was studied as a complement to the available emergency therapy in OP poisoning. It was used in conjunction with atropine , pralidoxime, and diazepam in nerve agent poisoning in primates.
Gacyclidine prevents the mortality observed after early administration of the aforementioned classic emergency medications. (Grade III recommendation) Electroencephalogram recordings and clinical observations revealed that gacyclidine prevented soman-induced seizures and motor convulsions. It also markedly accelerated clinical recovery of soman-challenged primates. Gacyclidine prevented the neuropathology observed 3 weeks after soman exposure in animals [72]. In a case of severe nerve agent poisoning, gacyclidine represented a promising adjuvant therapy to the currently available polymedication to ensure optimal management of OP nerve agent poisoning in humans. Administration of gacyclidine at zero to 30 min after intoxication obtains optimal neuropathological protection [109].
Serum Alkalization
Effects of sodium bicarbonate in OP pesticide poisoning were investigated in patients with moderate-to-severe intoxication. The goal of the investigation was to make an alkalization to reach and sustain the arterial blood pH between 7.45 and 7.55. Sodium bicarbonate was administered intravenously first to correct the metabolic acidosis, then as a constant infusion of 3–5 mg/kg/24 h until recovery or until atropine was required. Arterial blood gas analysis was performed at certain intervals to adjust the dosing [104, 105, 110, 111]. Esteratic portion of OP molecules are hydrolyzed in alkaline solution. Increasing one unit of pH is accompanied by a 10-fold increase in OP nerve agent hydrolysis. The arterial pH of >7.50 makes the OP hydrolysis faster particularly the nerve agents and their metabolites that are weak acids [112, 113]. However, it should be administered carefully to avoid severe metabolic alkalosis. Administration of sodium bicarbonate helps to control the cardiotoxicity as judged by electrocardiogram [114] (Grade III evidence).
Magnesium Sulfate
IV administration of magnesium sulfate (4 g) in the first day after admission would decrease the hospitalization period and improve outcomes in patients with OP pesticides poisoning [115] (Grade II-3 evidence). Magnesium sulfate may reduce ACh release by blocking calcium channels [116]. It also reduces CNS overstimulation and reversed the neuroelectrophysiological defects from OP toxicity [117]. Additionally, magnesium sulfate has a bronchodilating effect in mild to severe asthmatic patients, and it may relieve bronchoconstriction in a dose-dependent manner [118]. Magnesium sulfate has recently been administered up to 16 g per day in OP pesticides poisoning in the Mashhad Toxicology center without serious side effects. However, applying magnesium sulfate in nerve agents poisoning needs further study.
Drug Interactions
Drugs reported as contraindicated in severe OP nerve agent poisoning are morphine and its derivatives, aminophylline, theophylline, and chlorpromazine. Morphine derivatives and chlorpromazine potentiate the drowsiness and coma. Aminophylline and theophylline may potentiate nicotinic syndrome. Drugs known to be hydrolyzed by the enzyme cholinesterase, such as suxamethonium (succinylcholine ) and procaine, may have sustained effects [104].
Hemoperfusion
Effects of hemoperfusion through coated resin adsorbent synachrome E-5 were studied in five anesthetized dogs after intoxication by two to six times the LD50 of VX and another four dogs after intoxication by two to three times the LD50 of sarin. Hemoperfusion therapy prevented the development of serious signs of intoxication, provided that the dose of both nerve agents was only two times the LD50. It was concluded that hemoperfusion therapy in poisoning by the nerve agents sarin and VX is only partially successful [45].
Yokoyama et al. (1995) reported a 45-year-old woman who was severely intoxicated by sarin during Tokyo subway attack. She had been treated with atropine, 2-PAM, and respiratory support, while she received hemofiltration and hemoperfusion because of an insufficient response to treatment. When she regained consciousness, her pupils were dilated, cholinesterase activity had increased, and the patient survived [119].
Based on the first author’s clinical experience, charcoal hemoperfusion may be used in severely intoxicated OP nerve agent patients, as the OPs and some of their metabolites are lipid-soluble organic compounds and can be absorbed by charcoal.
Intravenous Lipid Emulsion
Following the introduction of intravenous lipid emulsion in the treatment of human poisoning with lipophilic drugs [120], some authors express a hypothesis that the combination of intravenous lipid emulsions can apply to treating severe OP poisoning [121]. However, in a study on mice, it showed no significant effect of intravenous lipid emulsion against OP toxicity [122]. Whether lipid emulsion is beneficial is unknown. For a severely poisoned patient in extremis, it may be potentially beneficial.
Special Populations
Pediatric Patients
Children are more susceptible to OP nerve agents, as was seen during the Sardasht and Halabjah massacres. Mortality was higher in children than in adults. Children have lesser mass and more surface/volume ratio, more immature respiratory system, and stratum corneum in the skin that facilitates dermal absorption. Besides, their neurotransmitter systems are immature that makes them more susceptible to an epileptogenic stimulus [105, 123].
Children are more sensitive to atropine and oximes [123]. Atropine administration should include the monitoring of vital signs, especially the pulse rate. Atropine must be adjusted based on heart rate between 140 and 160 beat/min [104, 123] (Grade III recommendation). Loading dose of pralidoxime in children should be at 25 mg/kg, which is infused over 15–30 min. It may continue by 10–20 mg/kg/h to achieve a plasma concentration of >4 mg/L [110, 124]. Half-life of pralidoxime in children is about twice that of adults [105].
The Program for Pediatric Preparedness of the National Center for Disaster Preparedness (NCDP) issued the first recommendations and treatment guidelines of pediatric disaster and terrorism awareness that is nationally accepted [125]. They recommended that the Mark 1 Auto-injector kits should be applied as first treatment of children with severe and critical nerve agents poisoning, especially when intravenous therapy is impossible or unavailable [123, 125]. In a recent experimental study, perinatal (postnatal day [PND] 7, 14 and 21) and adult (PND 70) rats were more susceptible than pubertal (PND 28 and 42) rats to the lethal effects associated with exposure to tabun, sarin, soman, and cyclosarin [126].
Pregnant Patients
OP nerve agents may cross the placenta and induce fetal intoxication. The fetus is more sensitive to OP nerve agents than the mother and more sensitive to atropine than the mother. Fetal intoxication may occur because OP nerve agents cross the placenta. The sensitivity of fetus to OP compounds and atropine is higher than their mothers [110]. Clinical experience on pregnant women in Sardasht and Halabjah who were exposed to sarin in the Iran-Iraq war discovered that mortality rate is higher in fetus than in the mothers [104, 110]. Fetus of survived sarin poisoned pregnant women died within a few hours to a few days [104]. However, some pregnant women in the second and third trimesters of pregnancy intoxicated with commercial OP compounds have been successfully treated with atropine and 2-PAM and have delivered healthy newborns [127].
In pregnant women, administration of atropine should be with caution and at lower doses. Pralidoxime has potential teratogenetic properties in animal studies, but has not been shown in humans and therefore should be used as clinically required [128]. Obstetric consultation may be necessary. Removing of a dead fetus should be performed immediately after improving the mother’s clinical condition [110].
OP nerve agents may be excreted in the mother’s milk. It would be advisable to stop breast feeding at least for a few days after exposure [44].
Elderly Patients
Elderly people also are more susceptible to OP nerve agents. Experience with sarin poisoning during the Iran-Iraq War in Sardasht and Halabjah revealed that morbidity and mortality were higher among the elderly. Multiple organ failure and complications were more common among the elderly than other adult age groups. Atropine , oxime , diazepam , and any other medication should be administered with caution. Depending on the age and clinical condition of the patient, critical care therapy should be initiated more rapidly. Elderly patients with OP nerve agent poisoning should be treated in the same priority group as children [104].
Rescue Staff and Hospital Personnel
Rescue staff and hospital personnel who are in contact with victims of OP nerve agent poisoning may become intoxicated due to secondary exposure. Among 59 rescuers and duty physicians, 8 had mild symptoms of sarin poisoning during the Matsumoto incident. All the rescue activities had taken place without gas masks or decontamination procedures [108].
Secondary contamination of house staff that treated victims occurred during the sarin Tokyo subway incident. More than 20% of the house staff had symptoms, including ocular pain, headache, sore throat, dyspnea, nausea, dizziness, and nasal pain, but none were seriously affected [7]. Rescue staff and medical personnel in the field, during transportation, and in the hospital should protect themselves by proper gas masks, clothing, and thick gloves (not surgical gloves) [104].
Experience in War and Terrorism
Observations during the nerve gas attack of the Iraqi army against the Iranian troops in Majnoon Island revealed that the heavily exposed people died within 30 min after onset of coma, convulsions, hypersecretion, respiratory failure, and apnea. Although the medical facilities were not adequate in Majnoon Island, first-aid treatment and decontamination were performed. The victims with moderate-to-severe intoxication were transferred from the field hospital to medical centers in big cities for further management [45].
Recorded clinical manifestations include miosis , hypersecretions, hypotension, nausea, vomiting, abdominal cramps, diarrhea, loss of consciousness, respiratory depression, cyanosis, pulmonary edema, muscle twitching, and convulsions. Bradycardia and hypotension were observed more before treatment with atropine , whereas tachycardia, normal hypertension, mydriasis, and dryness of the tongue were recorded more after atropinization. Morbidity and mortality were higher in patients with severe respiratory distress and cyanosis who received large doses of atropine. It is vital to correct the severe hypoxemia and cyanosis before atropinization (see section on “Treatment”). Suctioning of nasooropharyngeal and bronchial secretions (clear airway) and establishing adequate ventilation are the first priority. Intermediate syndrome, which was described after OP pesticide poisoning [63], has not been observed with nerve agent poisoning [44, 45].
Sulfur mustard was the most common chemical warfare agent that was used by the Iraqi army. Mixed poisoning by tabun and sulfur mustard also was common. No exact quantitative records of the nerve agent exposure are available. It has been estimated that greater than 2000 patients with nerve agent (later on diagnosed as tabun) poisoning were treated in March 1984. Another massive nerve agent poisoning occurred during the Halabjah massacre. It also was diagnosed as sarin and mixed with sulfur mustard [68, 69].
Two main terrorist attacks with sarin occurred in Japan. The first one occurred on June 27, 1994, in Matsumoto with about 600 casualties and 7 deaths [6]. The second attack occurred on March 20, 1995, in the Tokyo subway system, killing 11 and injuring more than 5500 people [7]. Diagnosis of sarin on both occasions was made based on the chemical analysis of environmental samples similar to the diagnosis of tabun in Majnoon Island and sarin in Halabjah [4]. Confirmative tests of serum sarin concentrations of the Halabjah massacre, Matsumoto incident, and Tokyo subway incident [70] and detection of sarin hydrolysis products from erythrocytes of four victims of the Tokyo subway incident [71] were performed after the incidents.
Preparation for a chemical incident resulting from an accident, war, or terrorism is important in every community. Because the rescue staff and medical personnel usually are from different departments, coordination between them is required. Guidelines and treatment protocols [129] should be available to all personnel. It should be updated at certain intervals to use the results of new research. For instance, recent clinical studies have confirmed that midazolam is effective when given at the onset of seizures caused by nerve agents. However, midazolam and the other benzodiazepines are less effective at terminating seizures when given 30 min or later after OP nerve agents seizure onset, likely because of internalization or downregulation of synapses, which can lead to diminished potency and seizure recurrence [130].
Teaching the staff and performing a simulation exercise at certain intervals is necessary. Public awareness through the mass media and even written instructions to the public are valuable and may prevent chaos during the chemical incident [45].
Key Points in the Diagnosis and Management of Nerve Agents
-
1.
Although plasma cholinesterase activity is given as percentages or U/mL, it should be valued qualitatively rather than quantitatively. Because of genetic variation in plasma cholinesterase, lower activity may be observed in 5–20% of normal individuals. However, treatment is based on clinical manifestations.
-
2.
Hypokalemia and metabolic acidosis, which occur during organophosphate nerve agent poisoning, should be corrected near to the upper limit of normal range.
-
3.
Administration of atropine in single repeated doses is mentioned in other textbooks. Mild-to-moderate atropinization must be produced and sustained until the patient’s recovery.
-
4.
Mydriatic eye drops are not needed; mydriasis will be induced by intravenous atropine.
-
5.
Aminophylline and theophylline should not be administered for bronchospasm during organophosphate nerve agent poisoning. Anticholinergic bronchodilators and β2-agonists (salbutamol, terbutaline) should be administered instead.
-
6.
Although pulmonary edema is less common in organophosphate nerve agent poisoning than in pesticide organophosphate poisoning, it should be treated only by atropine and not by morphine, aminophylline, furosemide, or digoxin. Morphine and aminophylline are contraindicated in organophosphate poisoning; furosemide might induce dehydration and electrolyte imbalance.
Conclusion
Nerve agents are the deadliest CWA that need immediate interventions. The Iraqi army used nerve agents against the Iranian troops and innocent civilians in the cities of Sardasht and Halabjah during the 1980s. Sarin was also used in terrorist actions in Matsomoto and Tokyo Metro in 1994 and 1995, respectively. It was used in Syria civil war as well in August 2013. In spite of the chemical weapons convention and the active role of the Organization for Prohibition of Chemical Weapons, nerve agents may be used again as CWAs in a war or terrorist attack. Therefore, health professionals should be familiar with the medical aspects of the nerve agents and prepare for appropriate action as required.
The nerve agents are OP compounds, similar to OP pesticides, but are more toxic than the pesticides. Applying first aid kits, for example, MARK1 is important to reduce toxicity. However, atropine and oximes are the well-known antidotes for the treatment of OP nerve agents. There are several adjuvant and additional therapies including magnesium sulfate, sodium bicarbonate, gacyclidine, benactyzine, tezampanel, hemoperfusion, and bioscavengers that have recently been used for OP nerve agents and pesticide poisoning with promising effects.
References
Holmsted B. The third symposium on prophylaxis and treatment of chemical poisons, April 22–24, 1985, Stockholm, Sweden. Fundam Appl Toxicol. 1985;5:S1–9.
Sidell FR, Groff WA. The reactivability of cholinesterase inhibited by VX and sarin in man. Toxicol Appl Pharmacol. 1974;27:241–52.
Foroutan A. Report of the specialist appointed by the Secretary- General of the United Nations to investigate allegation by the Islamic Republic of Iran concerning the use of chemical weapons. In: Proceedings of the First World Congress on Biological and Chemical Warfares, Ghent, May 21–23, 1984. p. 302–10.
Hendrickx B. Report and conclusion of the biological samples of men, intoxicated by war gases, sent to the Department of Toxicology of the State University of Ghent, for toxicological investigation. In: Proceedings of the Second World Congress on Biological and Chemical Warfares, Ghent, Aug 24–27, 1986. p. 553–582.
Balali-Mood M, Shariat M. Treatment of organophosphate poisoning: experience of nerve agents and acute pesticide poisoning on the effects of oximes. J Physiol Paris. 1998;92:375–8.
Morita H, Yanagisawa N, Nakajima T, et al. Sarin poisoning in Matsumoto, Japan. Lancet. 1995;346:290–3.
Ohbu S, Yamashina A, Takasu N, et al. Sarin poisoning on Tokyo subway. South Med J. 1997;90:587–93.
United Nations, General Assembly Security Council. Report of the United Nations Mission to Investigate Allegations of the use of chemical weapons in the Syrian Arab Republic on the alleged use of chemical weapons in the Ghouta area of Damascus on 21 Aug 2013. A/67/997 S/2013/553 (16th September 2013).
Dunn MA, Sidell FR. Progress in medical defense against nerve agents. JAMA. 1998;262:649–52.
Sidell FR, Borak J. Nerve agents. Ann Emerg Med. 1992;21:865–71.
Lockridge O, Masson P. Pesticides and susceptible populations: people with butyrylcholinesterase genetic variants may be at risk. Neurotoxicology. 2000;21:113–26.
Barak D, Ordentlich A, Kaplan D, et al. Evidence for P-N bond scission in phosphoramidate nerve agent adducts of human acetylcholinesterase. Biochemistry. 2000;39:1156–61.
Furlong CE, Li WF, Richter RJ, et al. Genetic and temporal determinants of pesticide sensitivity: role of paraoxonase (PON1). Neurotoxicology. 2000;21:91–100.
Inns RH, Tuckwell NJ, Bright JE, Marrs TC. Histochemical demonstration of calcium accumulation in muscle fibres after experimental organophosphate poisoning. Hum Exp Toxicol. 1990;9:245–50.
Bright JE, Inns RH, Marrs TC, Tuckwell NJ. Histochemical demonstration of sarin-induced calcium influx in mouse diaphragm. Hum Exp Toxicol. 1990;9:245–50.
Lee MJ, Clement JG. Effect of soman poisoning in haematology and coagulation parameters and serum biochemistry in rabbits. Mil Med. 1990;155:244–9.
Young GD, Koplovitz I. Acute toxicity of cyclohexylmethylphosphonofluoridate (CMPF) in rhesus monkeys: serum biochemical and hematologic changes. Arch Toxicol. 1995;69:379–83.
Rickell DJ, Glenn JF, Houston WE. Medical defense against nerve agents: new direction. Mil Med. 1987;152:35–41.
Worek F, Koller M, Thiermann H, et al. Diagnostic aspects of organophosphate poisoning. Toxicology. 2005;214(3):182–9.
Balali-Mood B. Chemistry and classification of OP compounds. In: Balali-Mood M, Abdollahi M, editors. Basic and clinical toxicology of organophosphorus compounds. 1st ed. London: Springer; 2014.
Gordon JJ, Inns RH, Johnson MK, et al. The delayed neuropathic effects of nerve agents and other organophosphate compounds. Arch Toxicol. 1983;52:82–6.
Pope C, Dilorenzo K, Ehrich M. Possible involvement of a neurotrophic factor during the early stages of organophosphate-induced delayed neurotoxicity. Toxicol Lett. 1995;75:111–7.
Silveria CL, Eldefrawi AT, Eldefrawi ME. Putative M2 muscarinic receptors of rat heart have high affinity for organophosphorous anticholinesterases. Toxicol Appl Pharmacol. 1990;103:474–81.
Albuquerque EX, Deshpande SS, Kawabuchi M, et al. Multiple actions of anticholinesterase agents on chemoreceptive synapses: molecular basis for prophylaxis and treatment of organophosphate poisoning. Fundam Appl Toxicol. 1985;5:S182–203.
Sivam SP, Hoskins B, Ho IK. An assessment of comparative acute toxicity of diisopropyl-fluorophosphate, Tabun, Sarin and soman in relation to cholinergic and GABAergic enzyme activities in rats. Fundam Appl Toxicol. 1984;19:23–32.
Szilagyi M, Gray PJ, Dawson RM. Effects of the nerve agents soman and tabun on the uptake and release of GABA and glutamate in synaptosomes of guinea pig cerebral cortex. Gen Pharmacol. 1993;24:663–8.
Liu DD, Watanabe HK, Ho IK, et al. Acute effects of soman, sarin and tabun on cyclic nucleotide metabolism in rat striatum. J Toxicol Environ Health. 1986;19:23–32.
Cao CJ, Mioduszewski RJ, Menking DE, et al. Cytotoxicity of organophosphate anticholinesterases. In Vitro Cell Dev Biol Anim. 1999;35:493–500.
Shih ML, McMonagle JD, Dolzine TW, et al. Metabolite pharmacokinetics of soman, sarin and GF in rats and biological monitoring of exposure to toxic organophosphorus agents. J Appl Toxicol. 1994;14(3):195–9.
Van der Schans MJ, Polhuijs M, van Dijk C, et al. Retrospective detection of exposure to nerve agents: analysis of phosphofluoridates originating from fluoride-induced reactivation of phosphylated BuChE. Arch Toxicol. 2004;78:508–24.
Minami M, Hui DM, Katsumata M, et al. Method for the analysis of the methylphosphonic acid metabolites of sarin and its ethanol-substituted analogue in urine as applied to the victims of the Tokyo sarin disaster. J Chromatogr B Biomed Sci Appl. 1997;695:237–44.
Van der Schans MJ, Lander BJ, van der Wiel H, et al. Toxicokinetics of the nerve agent (+/−)-VX in anesthetized and atropinized hairless guinea pigs and marmosets after intravenous and percutaneous administration. Toxicol Appl Pharmacol. 2003;191:48–62.
Munro NB, Talmage SS, Griffin GD, et al. The sources, fate, and toxicity of chemical warfare agent degradation products. Environ Health Perspect. 1999;107:933–74.
Reynolds ML, Little PJ, Thomas BF, et al. Relationship between the biodisposition of [3H]soman and its pharmacological effects in mice. Toxicol Appl Pharmacol. 1985;80:409–20.
Polak RL, Cohen EM. The binding of sarin in the blood plasma of the rat. Biochem Pharmacol. 1970;19:877–81.
Polak RL, Cohen EM. The influence of triorthocresylphosphate on the distribution of 32P in the body of the rat after the injection of 32P-sarin. Biochem Pharmacol. 1969;18:813–20.
Little PJ, Reynolds ML, Bowman ER, et al. Tissue disposition of [3H]sarin and its metabolites in mice. Toxicol Appl Pharmacol. 1986;83:412–9.
Little PJ, Scimeca JA, Martin BR. Distribution of [3H] diisopropyl fluorophosphate, [3H]soman, [3H]sarin, and their metabolites in mouse brain. Drug Metab Dispos. 1988;16:515–20.
Nakajima T, Sasaki K, Ozawa H, Sekjima Y, Morita H, Fukushima Y, Yanagisawa N. Urinary metabolites of sarin in a patient of the Matsumoto sarin incident. Arch Toxicol. 1998;72:601–3.
Allert M, Rizk SS, Looger LL, et al. Computational design of receptors for an organophosphate surrogate of the nerve agent soman. Proc Natl Acad Sci U S A. 2004;101:7907–12.
Benschop HP, Bijleved EC, de Jong LPA, et al. Toxicokinetics of the four stereoisomers of the nerve agent soman in atropinized rats, influence of soman simulator. Toxicol Appl Pharmacol. 1987;90:490–500.
Grob D. The manifestations and treatment of poisoning due to nerve gas and other organic phosphate anticholinesterase compounds. Arch Intern Med. 1956;98:221–39.
Sidell FR. Soman and sarin: clinical manifestations and treatment of accidental poisoning by organophosphates. Clin Toxicol. 1974;7:1–17.
Moshiri M, Alizadeh A, Balali-Mood M. Clinical management of Organophosphorus nerve agents’ poisonings. In: Balali-Mood M, Abdollahi M, editors. Basic and clinical toxicology of organophosphorus compounds. 1st ed. London: Springer; 2014.
Moshiri M, Darchini-Maragheh E, Balali-Mood M. Advances in toxicology and medical treatment of chemical warfare nerve agents. Daru. 2012;20:81–105.
Newmark J. Nerve agents. Neurol Clin. 2005;23:623–41.
Singer AW, Jaax NK, Graham JS, McLeod Jr CG. Cardiomyopathy in Soman and Sarin intoxicated rats. Toxicol Lett. 1987;36:243–9.
Balali-Mood M, Navaeian A. Clinical and paraclinical findings in 233 patients with sulfur mustard poisoning. In: Heyndrickx B, editor. Proceedings of the second world congress on new compounds in biological and chemical warfare, toxicological evaluation. Ghent: Ghent University Press; 1986. p. 464–73.
Engel CC, Jaffer A, Adkins J, Riddle JR, Gibson R. Can we prevent a second ‘Gulf War syndrome’? Population-based healthcare for chronic idiopathic pain and fatigue after war. Adv Psychosom Med. 2004;25:102–22.
Masson P. Evolution of and perspectives on therapeutic approaches to nerve agent poisoning. Toxicol Lett. 2011;206:5–13.
Tang FR, Loke WK, Ling EA. Comparison of status epilepticus models induced by pilocarpine and nerve agents – a systematic review of the underlying aetiology and adopted therapeutic approaches. Curr Med Chem. 2011;18:886–99.
Nakajima T, Sato S, Morita H, Yanagisawa N. Sarin poisoning of a rescue team in the Matsumoto sarin incident in Japan. Occup Environ Med. 1997;54:697–701.
Fullerton CS, Ursano RJ. Behavioral and psychological responses to chemical and biological warfare. Mil Med. 1990;155:54–9.
Page WF. Long-term health effects of exposure to sarin and other anticholinesterase chemical warfare agents. Mil Med. 2003;168:239–45.
Bajgar J. Organophosphates/nerve agent poisoning: mechanism of action, diagnosis, prophylaxis, and treatment. Adv Clin Chem. 2004;38:151–216.
Grauer E, Chapman S, Rabinovitz I, Raveh L, Weissman BA, Kadar T, Allon N. Single whole-body exposure to sarin vapor in rats: long-term neuronal and behavioral deficits. Toxicol Appl Pharmacol. 2008;227:265–74.
Lotti M. Organophosphorus compounds. In: Spencer PS, Schaumburg HH, Ludolph AC, editors. Experimental and clinical neurotoxicology. 2nd ed. New York: Oxford University Press; 2000.
Rengstoff RH. Accidental exposure to sarin: vision effects. Arch Toxicol. 1985;56:201–3.
Rickett DL, Glenn JF, Beers ET. Central respiratory effects versus neuromuscular actions of nerve agents. Neurotoxicology. 1953;8:466–75.
Decandole CA, Duglas WW, Evans CL, et al. The failure of respiration in death by anticholinesterase poisoning. Br J Pharmacol. 1953;8:466–75.
Stewart WC. The effects of sarin and atropine on the respiratory center and neuromuscular junctions of the rat. Can J Biochem Physiol. 1959;37:651–60.
Worek F, Kleine A, Falke K. Arrhythmias in organophosphate poisoning: effect of atropine and bispyridinium oximes. Arch Int Pharmacodyn Ther. 1995;3:418–35.
Senanayake N, Karalliede L. Neurotoxic effects of organophosphorous insecticides: an intermediate syndrome. N Engl J Med. 1987;316:761–3.
DeBleecker J, Van Den Neucker K, Willems J. The intermediate syndrome in organophosphate poisoning: presentation of a case and review of the literature. J Toxicol Clin Toxicol. 1992;30:321–9.
McLeod CG, Singer AW, Harrington DG. Acute neuropathology in soman poisoned rats. Neurotoxicology. 1984;5:53–8.
Anzueo A, Berdine GG, Moore GT, et al. Pathophysiology of soman intoxication in primates. Toxicol Appl Pharmacol. 1986;86:56–68.
Sekijima Y, Morita H, Yanagisawa N. Follow-up of sarin poisoning in Matsumoto. Ann Intern Med. 1997;127:1042–6.
Mulchandani P, Mulchandani A, Kaneva I, et al. Biosensor for direct determination of organophosphate nerve agents: 1. Potentiometric enzyme electrode. Biosens Bioelectron. 1999;14:77–85.
Mulchandani A, Pan S, Chen W. Fiber-optic enzyme biosensor for direct determination of organophosphate nerve agents. Biotechnol Prog. 1999;15:130–4.
Polhuijs M, Langenberg JP, Benschop HP. New method for retrospective detection of exposure to organophosphorous anticholinesterases: application to alleged sarin victims of Japanese terrorists. Toxicol Appl Pharmacol. 1997;146:156–61.
Nagao M, Takatori T, Matsuda Y, et al. Definitive evidence for the acute sarin poisoning diagnosis in the Tokyo subway. Toxicol Appl Pharmacol. 1997;144:198–203.
Nozaki H, Aikawa N, Fujishima S, et al. A case of VX poisoning and the difference from sarin. Lancet. 1995;346:698–9.
Klette KL, Levine B, Dreka C, et al. Cholinesterase activity in postmortem blood as a screening test for organophosphate/chemical weapon exposure. J Forensic Sci. 1993;38:950–5.
Jalali N, Balali-Mood M, Jalali I, et al. Electrophysiological changes in patients with acute organophosphorous pesticide poisoning. Basic Clin Pharmacol Toxicol. 2011;108(4):251–5.
John H, Breyer F, Thumfart JO, et al. Matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS) for detection and identification of albumin phosphylation by organophosphorus pesticides and G- and V-type nerve agents. Anal Bioanal Chem. 2010;398:2677–91.
Munro N. Toxicity of the organophosphate chemical warfare agents GA, GB, and VX: implications for public protection. Environ Health Perspect. 1994;102:18–37.
Wolfe AD, Rush RS, Doctor BP, et al. Acetylcholinesterase prophylaxis against organophosphate toxicity. Fundam Appl Toxicol. 1987;9:266–70.
Ravesh L, Grunwald J, Marcus D, et al. Human butyrylcholinesterase as a general prophylactic antidote for nerve agent toxicity: in vitro and in vivo quantitative characterization. Biochem Pharmacol. 1993;45:2465–74.
Caranto GR, Waibel KH, Asher JM, et al. Amplification of the effectiveness of acetylcholinesterase for detoxification of organophosphorus compounds by bis-quatenary oximes. Biochem Pharmacol. 1994;47:347–57.
Saxena A, Maxwell DM, Quinn DM, et al. Mutant acetylcholinesterase as potential detoxification agents for organophosphate poisoning. Biochem Pharmacol. 1997;54:269–74.
Mulchandani A, Kaneva I, Chen V. Detoxification of organophosphate nerve agents by immobilized Escherichia coli with surface expressed organophosphate hydrolase. Biotechnol Bioeng. 1999;63:216–23.
Broomfield CA, Lockridge O, Millard CB. Protein engineering of a human enzyme that hydolyzes V and G nerve agents: design, construction and characterization. Chem Biol Interact. 1999;119–120:413–8.
Cheng TC, DeFrank JJ, Rastogi VK. Alteromonas prolidase for organophosphorous G-agent decontamination. Chem Biol Interact. 1999;119–120:455–62.
Gordon RK, Feaster SR, Russell AJ, et al. Organophosphate skin decontamination using immobilized enzymes. Chem Biol Interact. 1999;119–120:463–70.
Sawyer TW, Parker D, Thomas N, et al. Efficacy of an oximate-based skin decontaminant against organophosphate nerve agents determined in vivo and in vitro. Toxicology. 1991;67:267–77.
Bajgar J. Prophylactic possibilities in case of high risk of exposure to nerve agents. In: Aroa R, Aroa P, editors. Disaster management, medical preparedness, response and homeland security. Boston: CAB International; 2013. p. 425–45.
Tuovinen K, Hannien O. Protection of mice against soman by pre-treatment with eptastigmine and physostigmine. Toxicology. 1999;139:233–41.
Kassa J, Fusek J. The positive influence of a cholinergic-anticholinergic pretreatment and antidotal treatment on rats poisoned with supralethal doses of soman. Toxicology. 1998;128:1–7.
Munro NB, Watson AP, Ambrose KR, et al. Treating exposure to chemical warfare agents: implications for health care providers and community emergency planning. Environ Health Perspect. 1990;89:205–15.
Holstege CP, Kirk M, Sidell FR. Chemical warfare: nerve agent poisoning. Crit Care Clin. 1997;13:923–42.
Orma PS, Middleton RK. Aerosolized atropine as an antidote to nerve gas. Ann Pharmacother. 1992;26:937–8.
van Helden HPM, Busker RW, Melchers BPC, et al. Pharmacological effects of oximes: how relevant are they? Arch Toxicol. 1996;70:779–86.
Dawson RM. Review of oximes available for treatment of nerve agent poisoning. J Appl Toxicol. 1994;14:317–31.
Boskovic B, Kovacevic V, Jovanovic D. PAM-2, HI-6 and HGG-12 in soman and tabun poisoning. Fundam Appl Toxicol. 1984;4:S106–15.
Clement JG, Hansen AS, Boulet CA. Efficacy of HLo-7 and pyrimidoxime as antidotes of nerve agent poisoning in mice. Toxicology. 1992;66:216–9.
Lundy PM, Hansen AS, Hand BT, et al. Comparison of several oximes against poisoning by soman, tabun and GF. Toxicology. 1992;72:99–105.
Melchers BP, Philippens IH, Wolthuis OL. Efficacy of HI-6 and HLo-7 in preventing incapacitation following nerve agent poisoning. Pharmacol Biochem Behav. 1994;49:781–8.
Cassel G, Karlsson L, Waara L, et al. Pharmacokinetics and effects of HI-6 in blood and brain of soman-intoxicated rats: a microdialysis study. Eur J Pharmacol. 1997;332:43–52.
Worek F, Widmann R, Knopff O, et al. Reactivating potency of obidoxime, pralidoxime, HI 6 and Hlo7 in human erythrocyte acetylcholinesterase inhibited by highly toxic organophosphorous compounds. Arch Toxicol. 1998;72:237–43.
Kopolovitz I, Menton R, Matthews C. Dose–response effects of atropine and HI-6 treatment of organophosphorous poisoning in guinea pigs. Drug Chem Toxicol. 1995;18:119–36.
Castro CA, Larsen T, Finger AV, et al. Behavioral efficacy of diazepam against nerve agent exposure in rhesus monkeys. Pharmacol Biochem Behav. 1992;41:159–64.
ATSDR. Medical management guidelines for Nerve Agents: Tabun (GA); Sarin (GB); Soman (GD); and VX. Agency for Toxic Substances and Disease Registry. 2012. http://www.atsdr.cdc.gov/MHMI/mmg166.pdf
ATSDR. Nerve agents (GA, GB, GD, VX). Agency for Toxic Substances and Disease Registry, Division of Toxicology. 2012. http://www.atsdr.cdc.gov/toxfaqs/tfacts166.pdf.
Balali-Mood M, Balali-Mood K. Neurotoxic disorders of organophosphorus compounds and their managements. Arch Iran Med. 2008;11:65–89.
Sidell FR, Newmark J, McDonough JH. Nerve agents. In: Lenhart MK, Tuorinsky SD, editors. Textbooks of military medicine, medical aspects of chemical warfare. 1st ed. Wshington, DC: Department of the army, United States of America; 2008.
McDonough Jr JH, Zoeffel LD, McMonagle J, et al. Anticonvulsant treatment of nerve agent seizures: anticholinergics versus diazepam in soman-intoxicated guinea pigs. Epilepsy Res. 2000;38:1–14.
Shih TM, Koviak TA, Capacio BR. Anticonvulsants for poisoning by the organophosphorus compound soman: pharmacological mechanisms. Neurosci Biobehav Rev. 1991;15:349–62.
McDonough JH. Midazolam: an improved anticonvulsant treatment for nerve agent-induced seizures. A technical report, 2002.
Hirbec H, Gaviria M, Vignon J. Gacyclidine: a new neuroprotective agent acting at the N-methyl-D-aspartate receptor. CNS Drug Rev. 2001;7:172–98.
Balali-Mood M, Saber H. Recent advances in the treatment of organophosphorous poisonings. IJMS. 2012;37:74–91.
Balali-Mood M, Ayati MH, Ali-Akbarian H. Effect of high doses of sodium bicarbonate in acute organophosphorous pesticide poisoning. Clin Toxicol (Phila). 2005;43:571–4.
Antonijvic B, Stefanovic D, Milovanovic ZA, et al. Standard antidotes along with sodium bicarbonate in organophosphate poisoning. In: Proceedings of chemical and biological medical treatment symposium (CBMTS); Spiez. April 28–May 3; 2002.
Koller M, Becker C, Thiermann H, et al. GC-MS and LC-MS analysis of nerve agents in body fluids: intra-laboratory verification test using spiked plasma and urine samples. J Chromatogr B Analyt Technol Biomed Life Sci. 2010;878:1226–33.
Cole JB, Stellpflug SJ, Gross EA, et al. Wide complex tachycardia in a pediatric diphenhydramine overdose treated with sodium bicarbonate. Pediatr Emerg Care. 2011;27:1175–7.
Pajoumand A, Shadnia S, Rezaie A, Abdi M, Abdollahi M. Benefits of magnesium sulfate in the management of acute human poisoning by organophosphorus insecticides. Hum Exp Toxicol. 2004;23:565–9.
Fuchs-Buder T, Tassonyi E. Magnesium sulphate enhances residual neuromuscular block induced by vecuronium. Br J Anaesth. 1996;76:565–6.
Eddleston M, Buckley NA, Eyer P, Dawson AH. Management of acute organophosphorus pesticide poisoning. Lancet. 2008;371:597–607.
Okayama H, Aikawa T, Okayama M, Sasaki H, Mue S, Takishima T. Bronchodilating effect of intravenous magnesium sulfate in bronchial asthma. JAMA. 1987;257:1076–8.
Yokoyama K, Ogura Y, Kishimoto M, et al. Blood purification for severe sarin poisoning after the Tokyo subway attack. JAMA. 1995;274:379.
Rothschild L, Bern S, Oswald S, et al. Intravenous lipid emulsion in clinical toxicology. Scand J Trauma Resusc Emerg Med. 2010;18:51.
Zhou Y, Zhan C, Li Y, et al. Intravenous lipid emulsions combine extracorporeal blood purification: a novel therapeutic strategy for severe organophosphate poisoning. Med Hypotheses. 2010;74:309–11.
Bania TC, Chu J, Stolbach A. The effect of intralipid on organophosphate toxicity in mice ACAD Emerg Med, 2005 Saem Annual Meeting Abstracts. 2005; 12 (Suppl 1) 7:12.
Baker MD. Antidotes for nerve agent poisoning: should we differentiate children from adults? Curr Opin Pediatr. 2007;19:211–5.
Barthold CL, Schier JG. Organic phosphorus compounds – nerve agents. Crit Care Clin. 2005;21:673–89.
Pediatric Expert Advisory Panel Participants. Atropine use in children after nerve gas exposure In Pediatric Expert Advisory Panel(PEAP) Addressing terrorism, Disaiter and public health emergency New York: Columbia university Maliman school of public health, National center for disaster preparedness; 1–8, 2004.
Wright LK, Lee RB, Vincelli NM, Whalley CE, Lumley LA. Comparison of the lethal effects of chemical warfare nerve agents across multiple ages. Toxicol Lett. 2016;241:167–74.
Terra-MacIver M, Larson K. Implication of chemical biological terrorist event for children and pregnant women. MCN. 2008;33(4):224–32.
Howland MA. Pyridoxine. In: Nelson L, Lewin N, Howland MA, Hoffman R, Goldfrank L, Flomenbaum NE, editors. Goldfrank’s toxicologic emergencies. 9th ed. NewYork: McGroHill; 2015.
Volans AP. Sarin: guidelines on the management of victims of a nerve gas attack. J Accid Emerg Med. 1996;13:202–6.
Reddy SD, Reddy DS. Midazolam as an anticonvulsant antidote for organophosphate intoxication – a pharmacotherapeutic appraisal. Epilepsia. 2015;56(6):813–21.
Author information
Authors and Affiliations
Corresponding authors
Editor information
Editors and Affiliations
Grading System for Levels of Evidence Supporting Recommendations in Critical Care Toxicology, 2nd Edition
-
I
Evidence obtained from at least one properly randomized controlled trial.
-
II-1
Evidence obtained from well-designed controlled trials without randomization.
-
II-2
Evidence obtained from well-designed cohort or case–control analytic studies, preferably from more than one center or research group.
-
II-3
Evidence obtained from multiple time series with or without the intervention. Dramatic results in uncontrolled experiments (such as the results of the introduction of penicillin treatment in the 1940s) could also be regarded as this type of evidence.
-
III
Opinions of respected authorities, based on clinical experience, descriptive studies and case reports, or reports of expert committees.
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this entry
Cite this entry
Balali-Mood, M., Balali-Mood, B., Balali-Mood, K. (2017). Nerve Agents. In: Brent, J., et al. Critical Care Toxicology. Springer, Cham. https://doi.org/10.1007/978-3-319-17900-1_73
Download citation
DOI: https://doi.org/10.1007/978-3-319-17900-1_73
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-17899-8
Online ISBN: 978-3-319-17900-1
eBook Packages: Biomedical and Life SciencesReference Module Biomedical and Life Sciences