Abstract
Rifampicin is an antibacterial drug which is highly effective in the treatment of tuberculosis and leprosy. It has been shown to exert antioxidative as well as anti-apoptotic effects. In this study, the neuroprotective effect of rifampicin was examined after 1-methyl-4-phenylpyridinium (MPP+)-induced dopaminergic cell death in vitro, and on the survival of retinal ganglion cells after optic nerve transection in vivo. Rifampicin administration significantly increased the number of surviving dopaminergic neurons after MPP+ intoxication as compared to control cultures. No cytotoxic effects were noted even at final rifampicin concentrations of 100 μM. In the rifampicin-treated group, retinal ganglion cell survival was significantly increased after axotomy as compared with vehicle-treated and phosphate-buffered saline-treated control animals. These results suggest that rifampicin is able to prevent neuronal degeneration in cell death paradigms involving oxidative stress and activation of apoptotic pathways. It may thus play a role in the future treatments of neurodegenerative disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
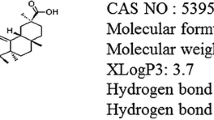
The most effective treatment for leprosy is the multi-drug therapy recommended by the World Health Organization consisting of dapsone, clofozamine and rifampicin [20]. It was recently reported that non-demented elderly leprosy patients showed an unusual absence of senile plaques in their brains compared with age-matched controls [15]. This report surmised that some drug being used for leprosy treatment might be neuroprotective. Rifampicin is a semi-synthetic derivative of the rifampycins, a class of broad-spectrum antibiotics that are fermentation products of Nocardia meditterranei. It reaches maximal serum concentrations 1–4 h after application and its plasma half time is 2–5 h [1]. The common structure of rifampycins is a naphthohydroquinone or naphthoquinone chromophore spanned by an aliphatic ansa chain [18]. This lipophilic ansa chain is mainly responsible for the transport of the drug across the blood-brain/retina barriers [14]. The structural feature of its naphthohydroquinone ring suggested that rifampicin may function as a hydroxyl radical scavenger, and it was shown to inhibit β-amyloid (Aβ) aggregation and Aβ-induced neurotoxicity [15]. Neuroprotective actions of free radical scavengers in neurodegenerative disorders have been well established [7].
In this study we evaluated putative neuroprotective effects of rifampicin on the survival of cultured dopaminergic (DAergic) neurons in the 1-methyl-4-phenylpyridinium (MPP+)-lesion paradigm in vitro and retinal ganglion cells (RGCs) after transection of the optic nerve (ON) in vivo.
Material and methods
Primary ventral midbrain floor culture
The mesencephalon floor was dissected from embryonic day 14 Wistar rats and further processed for establishing dissociated cell cultures as previously described [13]. In brief, tissue pieces were collected in ice-cold calcium-magnesium-free balanced salt solution and centrifuged at 1,000 rpm for 4 min. The tissue pellet was incubated in 750 µl trypsin (0.25%, 15 min, 37°C; Sigma). Trypsin was inactivated by addition of 750 µl cold fetal calf serum. The pellet was dissociated by gentle trituration using a fire-polished Pasteur pipette. After centrifugation at 1,000 rpm for 4 min, the pellet was resuspended in warm culture medium. Cells were seeded in poly-l-ornithine/laminin (Sigma)-coated 96-well culture plates (Nunc) at a density of 175,000 cells/cm2. Cultures were maintained at 37°C in a humidified atmosphere and 5% CO2 in DMEM/F12 plus the N1 supplements and antibiotics for 4 or 7 days. Medium was changed on days in vitro (DIV) 1 and 3. Cultures were virtually free of glial fibrillary acidic protein-positive astroglial cells throughout the culture period [12, 13]. Rifampicin (Sigma) was added on DIV 4 at concentrations of 0.1, 1, 10 or 100 mM. 3 h after rifampicin application MPP+ (Sigma) was added to the culture at a final concentration of 4 µM. Cells were fixed 24 h after MPP+ application with 4% formaldehyde and immunocytochemically stained for tyrosine hydroxylase (TH) as previously described [13]. Numbers of TH-positive cells were counted in approximately 10% of the culture area in each well (n=4) using a fluorescence microscope (Axioplan; Zeiss, Germany).
Animal groups and RGC labeling technique
All experimental procedures were carried out according to the National Institutes of Health guidelines for the care and use of laboratory animals with permission of local government authorities. Adult male C57BL/6J mice (Charles River Laboratory, Sulzfeld, Germany), weighing 22–25 g, were assigned to the following experiments and groups: (a) phosphate-buffered saline (PBS)-treated group (n=3); (b) vehicle-treated group (n=6); (c) rifampicin-treated group (n=7). All retinas were prepared 14 days following ON axotomy. RGCs were retrogradely labeled prior to ON transection. Animals were anesthetized by i.p. injection of 7% chloral hydrate. The superior colliculi were exposed by drilling a bur hole into the pericranium 0.7 mm lateral to the sagittal suture and 3.0 mm posterior to bregma. A Hamilton syringe was inserted 2.0 mm beneath the surface of the brain, and 0.750 µl Fluorogold (FG, Fluorochrom, LLC, Denver, CO; infusion rate 0.7 µl/min) were injected stereotactically into both superior colliculi. After infusion, the needle remained inside the tissue for 2 min to prevent FG diffusion along the needle track, before the syringe was withdrawn, and the wound closed with a suture [10].
ON axotomy and administration of rifampicin
Four days after labeling, mice were anesthetized by i.p. injection of 7% chloral hydrate. After skin incision close to the superior orbital rim, the right orbita was opened, leaving the supraorbital vein intact, and the lacrimal gland was resected subtotally. After spreading the superior extraocular muscles, the right ON was transected under microscopical control approximately 0.5 mm distant to the posterior pole of the eye, taking care not to damage the retinal blood vessels. The wounds were sutured and the retinal blood supply was verified by fundoscopy [10].
Rifampicin (Sigma Chemicals, St Louis, MO) was dissolved in ethanol and further diluted in normal saline to a final concentration of 13%. A rifampicin bolus of 5 mg/kg body weight was injected i.p. just after axotomy. Two micro-osmotic pumps (Alzet, Palo Alto, CA; model 1002) were placed into the abdominal cavity after ON transection. During the subsequent 14 days, rifampicin (5 mg/kg body weight per day) was continuously applied i.p. with the micro-osmotic pump at a flow rate of 0.5 µl/h.
Tissue processing
At 14 days after ON transection, the mice were killed by an overdose of chloral hydrate and both eyes were removed. The retinas were dissected, fixed in 4% paraformaldehyde (PFA) in 0.1 M PBS for 30 min and flat-mounted on glass slides. Survival of RGCs was evaluated by fluorescence microscopy using a rhodamine filter (546/590 nm). RGC densities were determined by counting tracer-labeled RGCs in 12 distinct areas of 62,500 μm2 each (three areas per retinal quadrant at three different retinal eccentricities of 1/6, 3/6 and 5/6 of the retinal radius, respectively) [5]. Only those cells were counted that were clearly detectable as RGCs because of their size and morphology. The RGCs were round, and cell bodies were bigger than those of microglial cells, which were FG-positive to some extent because of phagocytosis.
Statistics
For statistical data comparisons, a standard software package (SPSS for Windows) was used. Differences between groups in the in vivo experiments were measured by repeated measures ANOVA. Differences between groups in the in vitro experiments were calculated by unpaired t-tests. All values are given as mean ± SD. P values less than 0.05 are considered significant.
Results
Effects of rifampicin on survival of DAergic neurons in vitro
Treatment of midbrain cultures with rifampicin did not affect survival of DAergic neurons in a statistically significant manner as compared to the non-rifampicin-treated group. Most importantly, no toxic effect of rifampicin was noted up to a final concentration of 100 µM (Fig. 1; control group).
MPP+ administration to midbrain cultures resulted in a reduction of surviving DAergic neurons to approximately 62–70% of control values, in the 0.1 µM and 0 µM rifampicin-treated groups, respectively. Rifampicin at concentrations of 1, 10 and 100 µM significantly increased the number of surviving DAergic neurons as compared to the non-rifampicin-treated controls. DAergic cell numbers could be restored to up to 88–99% of the control values (Fig. 1; MPP+ group).
Effects of rifampicin on survival of RGCs in vivo
Cell counts of FG-labeled RGCs from axotomized animals are summarized in Fig. 2 and Table 1. Rifampicin treatment significantly increased the number of surviving RGCs as compared to vehicle-treated or PBS-treated animals. The effect of rifampicin, vehicle-treated control and PBS-treated control on the density of RGCs are shown in Fig. 3. The number of viable cells in the rifampicin-treated animals was significantly increased as compared with PBS-treated control and vehicle treated animals (Fig. 3). The number of viable cells in the vehicle-treated animals was also increased as compared with PBS-treated control animals. However, this neuroprotection was not at a significant level. Rifampicin rescued 1.5–2 times more RGCs at 1/6, 3/6 and 5/6 of the retinal radius than control injections (Table 1; Fig. 2).
RGCs surviving 14 days after ON transection, given as fractions of cell numbers in non-axotomized eyes. Areas were counted separately at one-sixth, one-half, and five-sixths of the retinal radius as indicated. *Significant difference (P<0.05) compared with PBS-treated control animals. $Significant difference (P<0.05) compared with vehicle-treated control animals. Data are given as mean ± SD (RGC retinal ganglion cell, ON optic nerve)
Effects of rifampicin on the RGCs surviving 14 days after ON transection. Note that the number of viable RGCs was significantly increased in rifampicin-treated mice as compared with control animals. *Significant difference (P<0.05) compared with PBS-treated control animals. $Significant difference (P<0.05) compared with vehicle-treated control animals. Data are given as mean ± SD
Discussion
In the present study, we evaluated the neuroprotective effects of rifampicin on DAergic neuron and RGC survival in a combined in vitro and in vivo approach using the MPP+ intoxication and ON axotomy models. After rifampicin administration, cell numbers of TH-labeled DAergic neurons and of FG-labeled RGCs were significantly increased.
Oxidative stress has been shown to play a major role in the pathophysiology of neurodegeneration in both experimental models employed in our study. MPP+ is the active metabolite of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP); in vivo MPTP is metabolized to MPP+ by astroglial cells and then taken up into DAergic neurons by the dopamine transporter [16]. MPP+ exerts its neurotoxic actions by inhibition of the complex I activity of the respiratory chain as well as induction of lipid peroxidation. MPP+-induced cell death is also associated with activation of apoptotic cascade elements, e.g., the JNK pathway, p53-, Bax-signaling and caspase activation [4]. Antioxidative agents, e.g., U-78517F and deprenyl, and radical scavengers, e.g., DMSO, have previously been shown to be protective against MPP+-induced neuron damage [21].
Transection of the ON triggers a highly coordinated response of injury-associated genes, which finally leads to apoptosis of RGCs [8, 11]. There is evidence to suggest that free oxygen radicals enhance injury programs. Free oxygen radicals are highly reactive molecules that contain one or more unpaired electrons. Under normal physiological conditions, antioxidant defense mechanisms are present to combat reactive oxygen radicals. In neurodegenerative disease, production of reactive oxygen species overwhelms endogenous scavenging mechanisms and is able to damage lipids, proteins, nucleic acids and carbohydrates. Antioxidant agents suppress apoptosis induced by various insults, including axotomy [3].
The free radical-scavenger activity of rifampicin has already been shown by electron spin resonance spectrometric analysis and stable free radical, alpha, alpha-diphenyl-beta-picrylhydrazyl (DPPH) reduction [9, 15]. Next to the antioxidative properties of rifampicin, several other mechanisms have been discussed as being neuroprotective: recent studies showed that rifampicin binds to and activates glucocorticoid receptors (GRs), resulting in the induction of transcription of genes controlled by glucocorticoid receptor-binding elements [2]. GRs were shown in isolated Müller and photoreceptor cells in intact salamander retina and in all cell types in the human eye [17]. Activated GRs can inhibit AP-1, which in turn is essential for the induction of photoreceptor apoptosis by light. GR-mediated inhibition may occur in the nucleus of retinal cells by a protein-protein interaction of both transcription factors. Thus, induction of GR activity prevents light–induced retinal degeneration by interference with AP-1-dependent steps of apoptosis induction in mice [19]. Gollapudi et al. [6] reported that rifampicin-mediated inhibition of apoptosis and activation of caspase-3 and capase-8 occurred at least in part via GR activation. Furthermore, rifampicin down-regulated the expression of pro-apoptotic Bax and up-regulated the expression of anti-apoptotic Bcl-2, Bcl-XL and of anti-apoptotic gene products such as XIAP, cIAP2, FLIPs, which play essential roles to block programmed cell death.
Rifampicin is a well-established and generally well-tolerated drug for the treatment of tuberculosis and leprosy. Our present data underline the pathophysiological significance of the neuroprotective mechanisms of this compound. Rifampicin may, therefore, play a beneficial neuroprotective role in the future treatment of neurodegenerative diseases, such as Parkinson’s disease.
References
Acocella G (1978) Clinical pharmacokinetics of rifampicin. Clin Pharmacokinet 3:108–127
Calleja C, Pascussi JM, Mani JC, Maurel P, Vilarem MJ (1998) The antibiotic rifampicin is a nonsteroidal ligand and activator of the human glucocorticoid receptor. Nat Med 4:92–96
Castagne V, Clarke PG (1996). Axotomy-induced retinal ganglion cell death in development: its time course and its dimunition by antioxidants. Proc R Soc Lond B Biol Sci 263:1193–1197
Eberhardt O, Schulz JB (2003) Apoptotic mechanisms and antiapoptotic therapy in the MPTP model of Parkinson’s disease. Toxicol Lett 4:135–151
Eschweiler GW, Bahr M (1993) Flunarizine enhances rat retinal ganglion cell survival after axotomy. J Neurol Sci 116:34–40
Gollapudi S, Jaidka S, Gupta S (2003) Molecular basis of rifampicin-induced inhibition of anti-CD95-induced apoptosis of peripheral blood T lymphocytes: the role of CD95 ligand and FLIPs. J Clin Immunol 23:11–22
Hal ED (1997) Antioxidant pharmacotherapy. In: Ginsberg M, Bogousslavsky J (eds) Cerebrovascular disease: pathophysiology, diagnosis and management. Blackwell Science, Malden
Isenmann S, Wahl C, Krajewski S, Reed JC, Bahr M (1997) Up-regulation of Bax protein in degenerating retinal ganglion cells precedes apoptotic cell death after optic nerve lesion in the rat. Eur J Neurosci 9:1763–1772
Karunakar N, Prabhakar MC, Krishna DR (2003) Determination of antioxidant activity of some drugs using high-pressure liquid chromatography. Arzneimittelforschung 53:254–259
Kilic E, Hermann DM, Isenmann S, Bahr M (2002) Effects of pinealectomy and melatonin on the retrograde degeneration of retinal ganglion cells in a novel model of intraorbital optic nerve transection in mice. J Pineal Res 32:106–111
Klocker N, Cellerino A, Bahr M (1998) Free radical scavenging and inhibition of nitric oxide synthase potentiates the neurotrophic effects of brain-derived neurotrophic factor on axotomized retinal ganglion cells in vivo. J Neurosci 18:1038–1046
Krieglstein K, Suter-Crazzolara C, Hotten G, Unsicker K (1995) Trophic and protective effects of growth/differentiation factor 5, a member of the transforming growth factor-beta superfamily, on midbrain dopaminergic neurons. J Neurosci Res 42:724–732
Lingor P, Unsicker K, Krieglstein K (2000) GDNF and NT-4 protect midbrain dopaminergic neurons from toxic damage by iron and nitric oxide. Exp Neurol 163:55–62
Mindermann T, Landolt H, Zimmerli W, Rajacic Z, Gratzl O (1993) Penetration of rifampicin into the brain tissue and cerebral extracellular space of rats. J Antimicrob Chemother 31:731–737
Namba Y, Kawatsu K, Izumi S, Ueki A, Ikeda K (1992) Neurofibrillary tangles and senile plaques in brain of elderly leprosy patients. Lancet 340:978
Przedborski S, Chen Q, Vila M, Giasson BI, Djaldatti R, Vukosavic S, Souza JM, Jackson-Lewis V, Lee VM, Ischiropoulos H (2001) Oxidative post-translational modifications of alpha-synuclein in the 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) mouse model of Parkinson’s disease. J Neurochem 76:637–640
Psarra AM, Bochaton-Piallat ML, Gabbiani G, Sekeris CE, Tsacopoulos M (2003) Mitochondrial localization of glucocortocoid receptor in glial (Muller) cells in the salamander retina. Glia 41:38–49
Tomiyama T, Shoji A, Kataoka K, Suwa Y, Asano S, Kaneko H, Endo N (1996) Inhibition of amyloid β protein aggregation and neurotoxicity by rifampicin. J Biol Chem 271:6839–6845
Wenzel A, Grimm C, Seeling MW, Jaissle G, Hafezi F, et al (2001) Prevention of photoreceptor apoptosis by activation of the glucocorticoid receptor. Invest Ophthalmol Vis Sci 42:1653–1659
World Health Organization (1988) WHO Expert Committee on leprosy, sixth report. Tech. Rep. Ser. 768, WHO, Geneva
Wu RM, Murphy DL, Chiueh CC (1996). Suppression of hydroxyl radical formation and protection of nigral neurons byl-deprenyl (selegiline). Ann N Y Acad Sci 15:379–390
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kilic, Ü., Kilic, E., Lingor, P. et al. Rifampicin inhibits neurodegeneration in the optic nerve transection model in vivo and after 1-methyl-4-phenylpyridinium intoxication in vitro. Acta Neuropathol 108, 65–68 (2004). https://doi.org/10.1007/s00401-004-0867-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-004-0867-6