Abstract
Purpose
This study aimed to explore the differences in iodine metabolism and expression of NIS and Pendrin in pregnant rats under different iodine nutritional status.
Methods
Female Wistar rats were divided into four groups: low iodine (LI), normal iodine (NI), ten fold high iodine (10HI), and fifty fold high iodine (50HI). The intervention began after one week of adaptive feeding. Iodine metabolism experiments were performed beginning on the 15th day of pregnancy. 24-h iodine intake and excretion were calculated. The concentrations of iodine in urine, fecal, thyroid, and placenta were measured by ICP-MS. PCR and Western Blot were used to detect the mRNA levels and cell membrane protein of sodium/iodide symporter (NIS) and Pendrin in the small intestine, thyroid, kidney, and placenta.
Results
Fecal iodine excretion (FIE) and urinary iodine excretion (UIE) in the 50HI group were significantly higher than those in the NI group (P < 0.05). The NIS protein and mRNA in the kidney and small intestine have an upward trend in iodine deficiency and a downward trend in iodine excess. Thyroid and placental iodine storage in the 50HI group were significantly higher than those in the NI group (P < 0.05). NIS, Pendrin protein, and mRNA in the thyroid and placenta tend to increase when iodine is deficient and decrease when there is excess.
Conclusion
Iodine excretion and iodine stores in the placenta and thyroid gland are positively correlated with iodine intake. NIS and Pendrin are also regulated by iodine intake.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Iodine is crucial for the synthesis of thyroid hormones (THs) in the thyroid and the subsequent action of these hormones in the organism [1]. Pregnant women are sensitive to iodine malnutrition, which can also cause damage to the development of infants [2]. Severe iodine deficiency during pregnancy will affect the thyroid function of pregnant women and cause new-born cretinism [3, 4]. Even mild iodine deficiency may be associated with offspring’s intellectual impairment [5, 6]. Iodine excess during pregnancy may lead to hypothyroidism in the pregnant women and fetus. Rapid normalization of fetus/newborn thyroid function is necessary to prevent neurological damage [7]. At present, there are few studies on how the body regulates the absorption, storage, and excretion of iodine to maintain iodine homeostasis under different iodine exposures.
Iodine metabolism mainly includes the absorption, storage, excretion, and reabsorption of iodine. The metabolism experiment is a direct evaluation method to assess the physiological requirements of iodine. In classical iodine metabolism experiments, the iodine intake was used as the estimated average requirement (EAR) in the population when the subject reached a “zero balance” (iodine intake was equal to iodine excretion) [8]. Current research shows that when the iodine intake is different, the iodine intake when reaching “zero balance” is different, so the EAR obtained is different [9]. This has confused the formulation of recommended iodine intakes.
Iodine is principally transported by the sodium/iodide symporter (NIS) and anion exchanger of Pendrin [10]. The expression of NIS and Pendrin is currently found in the thyroid, mammary gland, kidney, small intestine, and placenta [10, 11]. Dietary iodine enters the blood through small intestinal epithelial cells [12]. Studies have shown that an enriched diet decreases NIS protein expression in small intestinal enterocytes [13]. The thyroid is the most important site for iodine metabolism and storage [14]. Furthermore, previous studies indicate that the placenta stores iodine in a concentration-dependent manner and serves as a long-term storage supply [15,16,17]. When iodine intake is excessive, NIS and Pendrin expression is compensatorily decreased in the thyroid [18, 19]. It has also been shown that when iodine intake is insufficient, Pendrin and glycosylated NIS in the placenta were significantly upregulated in a dose-dependent manner[17, 20]. The kidney is responsible for the excretion and reabsorption of iodine [21]. NIS is, at least partially, involved in driving renal iodine transport [21]. There is a lack of studies on the regulatory mechanisms of NIS in the kidney.
In this study, the levels of iodine excretion and storage, as well as the expression of NIS and Pendrin in the small intestine, thyroid, placenta, and kidney were determined via pregnant rats fed under different iodine nutritional status. We aimed to explore how the body maintains iodine homeostasis through multi-organ coordination under different iodine nutritional statuses and the role and regulation of NIS and Pendrin gene expression in related events.
Materials and methods
Animals and dietary treatment
32 female and 20 male Wistar rats aged 4 weeks were provided by the SPF (Beijing) Biotechnology Co., Ltd (Grade SPF, Certificate Number SYXK (Beijing) 2019–0010). The Tianjin Hospital of ITCWM Nankai Hospital Animal Ethics Committee approved all the experimental procedures (NKYY-DWLL-2021–048). All rats were housed in a specific pathogen-free facility under a controlled temperature (23 ± 1) °C and humidity (50 ± 5)% environment with a 12-h light/dark cycle, allowing free access to food and water. The intervention began after one week of adaptive feeding.
Female Wistar rats were randomly divided into four groups according to the concentration of KI in drinking water: low iodine group (LI, 1 μg/day), normal iodine group (NI, 6 μg/day), ten fold high iodine group (10HI, 60 μg/day), and fifty fold high iodine group (50HI, 300 μg/day). According to the iodine content of normal chow, 6 μg/day was considered as normal iodine intake [22]. Considering the average dosage of normal chow to be 20 g/day and the average dosage of water to be 30 ml/day, we calculated the iodine intake dosage per day of rats in the high-iodine groups. All rats were given a low iodine diet which has plenty of other nutrients and the average dietary iodine content was 50 μg/kg (Trophic Animal Free High-tech Co. Ltd, China, TP016ID103). Rats in the LI group were provided with deionized water daily and the other groups were given deionized water supplemented with potassium iodide (KI): the NI control group obtained 0.218 μg/ml, the 10HI group obtained 2.575 μg/ml, and the 50HI group obtained 13.028 μg/ml. The iodine concentration of drinking water was adjusted weekly according to the actual food intake and drinking volume of rats. Male rats were fed the same as female rats in the NI group.
After 10 weeks of conditional intervention, female rats were cohabited and mated. After confirming the pregnancy through the presence of spermatozoa in the vaginal smear [23], the pregnant rats were housed in individual cages. Iodine metabolism experiments were performed for 3 days beginning on the 15th day of pregnancy, and the rats continued to be fed water with different iodine concentrations as before. After the iodine metabolism experiment, all the rats were anesthetized with pentobarbital (40 mg/kg, intraperitoneally), bled, and perfused with buffered saline. Blood, small intestine, thyroid, kidney, and placenta were removed and weighed.
Iodine metabolism experiment
On the 15th day of pregnancy, pregnant female rats were placed in metabolic cages at 10 a.m. to accomplish an iodine metabolism experiment, which was repeated for 3 days. Adequate low iodine diet and corresponding water of different KI concentrations were given and recorded. 24-h (24-h) urine and 24-h feces of the rats were collected. On the next morning at 10 a.m., residual feed, residual water, 24-h urine, and 24-h feces were recorded. Iodine concentrations in urine and feces were measured. Dietary iodine intake (DII), water iodine intake (WII), urinary iodine excretion (UIE), and fecal iodine excretion (FIE) were measured and calculated. Iodine balance value (IBV) = iodine intake (DII + WII)-iodine output (UIE + FIE).
Thyroid function test
Serum thyroid-stimulating hormone (TSH), free triiodothyronine (FT3), and free tetraiodothyronine (FT4) were measured using an automatic IMMULITE analyzer with a chemiluminescent kit (Sophonix, China).
HE staining
HE staining of the thyroid was performed with a HE Staining kit (Beyotime, China) according to the manufacturer’s instructions. The images (at 20× magnification) were captured by an Olympus IX81 microscope (Olympus, Japan) in bright-field mode.
Measurement of iodine in tissue and metabolite
The iodine concentration of urine, feces, thyroid, and placenta was detected by Inductively Coupled Plasma Mass Spectrometry (ICP-MS, iCAP Q, Thermo Fisher Scientific, Germany) using Te for mass bias correction. Iodine content measurements were carried out at least three times. Standard materials were used as standards for the determination of each batch of samples.
The tissue was digested with 25% tetra-methyl-ammonium hydroxide (TMAH) at 90 °C for 5 h. The within-samples CV was 1.8% and the between-samples CV was 4.5% for tissue iodine concentration (IC). Urine samples were diluted (21-fold) with 0.25% TMAH, 0.02% Triton X-100, and 100 mg/l Te before analysis using ICP-MS. The total inter-assay and intra-assay CV for UIC measurements were 1.4–3.2% and 0.6–1.8%, respectively.
Immunohistochemistry
After the small intestine, thyroid, placenta, and kidney were removed, they were immediately fixed with 4% paraformaldehyde and then embedded in paraffin. Sections were dewaxed and rehydrated and the next steps were performed with rabbit-specific HRP/DAB (ABC) IHC Detection Kit ab64261(Abcam, UK). The tissue section of maternal rats was incubated with the primary antibody of rabbit anti-sodium iodine symporter (1:100; Proteintech, China) or rabbit anti-SLC26A4 (1:100; Santa Cruz) overnight at 4 °C. Then the biotinylated secondary antibody was bound to the primary antibody, and the HRP-labeled streptavidin was bound to the secondary antibody. The HRP produced a brown-colored substance at the site of primary antibody binding by reacting with DAB. The images were obtained with an inverted microscope (IX81; Olympus, Tokyo, Japan).
Western blot
Membrane proteins from the small intestine, thyroid, placenta, and kidney of maternal rats were obtained with the Membrane and Cytosol Protein Extraction Kit (Beyotime, China). Protein samples were fractionated through SDS-PAGE and transferred onto PVDF membranes (PVDF; Millipore, Billerica, MA). The PVDF membranes were blocked with 5% BSA (Sigma) in 1× Tris-buffered saline Tween for 1 h at room temperature. Then the membranes were incubated with primary antibody of mouse anti-NIS (1:500; Santa Cruz, USA), rabbit anti-SLC26A4 (1:500; Santa Cruz), and rabbit anti-GAPDH (Loading Control) (1:5000; Bioss) overnight at 4 °C. After incubation, the membrane was washed with TBST, relational horseradish peroxidase [HRP]-conjugated secondary antibodies were added, and incubated at room temperature for 1 h. Then, the proteins were detected by chemiluminescence reagents (Shandong Sparkjade) and observed using a ChemiDocTM XRS+ Imaging System (Bio‐Rad, Hercules, CA). The protein levels were quantified by densitometry using NIH ImageJ 1.61 Software (National Institutes of Health, Bethesda, MD, USA).
RNA extraction and real-time PCR analysis
The total RNA of the small intestine, thyroid, placenta, and kidney was extracted using a TRIzol reagent. RNA was reverted to cDNA using the SPARK script II RT Kit (Shandong Sparkjade, China), and cDNA was quantified using SYBR Green (Life Technologies). PCRs were conducted in a Real-Time PCR Machine Roche Light Cycler 480 under the conditions of 95 °C for 1 min for PCR initial heat activation, followed by 40 cycles of 95 °C for 20 s for denaturation, 60 °C for 20 s, and 72 °C for 30 s for combined annealing/extension. All experiments were conducted in three separate replicates. The gene expression data were analyzed using the comparative 2-DDCt method with act-1 as the normalizer. Primer sequences are described in Supplementary Table S1.
Statistical analysis
Results were expressed as mean ± standard deviation (SD). Comparisons among different groups were performed by one-way ANOVA and followed by an LSD test for multiple comparisons. The statistical software package SPSS 20.0 (IBM Corp., USA) was used to evaluate differences among groups, which were considered statistically significant at P < 0.05.
Results
Concentrations of serum thyroid hormone and thyroid morphologic changes in pregnant rats
TSH tended to decrease with the increase in iodine intake, while the differences were not statistically significant. (Fig. 1a). The levels of FT4 were stable in the NI group, while the values of LI, 10HI, and 50HI groups fluctuated greatly (Fig. 1c). FT4 values in the 10HI and 50HI groups were significantly higher than that in the NI group (P < 0.05).
Concentrations of plasma thyroid hormone and thyroid morphologic changes in pregnant rats. a–c Serum thyroid hormone concentration with different iodine concentrations. TSH thyroid stimulating hormone, FT3 free triiodothyronine, FT4 free thyroxine (values were shown as mean ± SD, n = 8 per group, comparisons among different groups were performed by one-way ANOVA and followed by LSD test for multiple comparisons. #P < 0.05 compared with the NI group). d–g Representative micrographs of HE staining in the thyroid. Scale bars: 20 μm
To further verify the effect of modeling, the pregnant rats were killed after the iodine metabolism experiment, and thyroid morphologic changes were observed by HE staining. As shown in Fig. 1d–g, most of the thyroid follicles were round or oval and were medium-sized in the NI group. The follicular epithelial cells were cuboidal. Follicular cavities were filled with glia, and new small follicles were occasionally observed between follicles. Compared with the NI group, the thyroid follicles in the LI group were significantly smaller and were increased in number. Epithelial cells proliferated and became hypertrophy. Mostly columnar intrafollicular glia were significantly reduced. In the 10HI and 50HI groups, the thyroid follicles were significantly enlarged. The epithelial cells were flat, and the follicular cavities were filled with abundant densely stained glia.
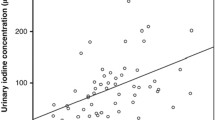
Iodine absorption and excretion vary in pregnant rats with different iodine intakes
To explore the absorption and excretion of iodine under different iodine nutrition conditions, we further carried out an iodine metabolism experiment (Table 1). FIE represents iodine that was not absorbed by the small intestine. With the increase in iodine intake, FIE also tended to increase, and the 50HI group significantly increased compared with the NI group. The ingested iodine was actively excreted in the urine. The total 24-h UIE was 0.49 ± 0.38, 14.00 ± 14.32, 25.11 ± 12.56 and 166.68 ± 49.46 μg/day in the LI, NI, 10HI, and 50HI groups. There was a significant change between the NI and 50HI groups (P < 0.05). IBV represents all iodine intake minus all iodine output. When iodine was excessive, IBV values increased significantly, that is, the output of iodine was significantly lower than the intake, indicating that some iodine was stored in the body.
Compensatory effects of the small intestine and kidney on iodine deficiency and iodine excess
We tested the localization of NIS and Pendrin in the small intestine (Fig. 2a, b) and kidney (Fig. 3a, b). The protein expression and mRNA levels of NIS in the small intestine (Fig. 2d and f) and kidney (Fig. 3d and f) in the LI group were significantly higher than those in the NI group (P < 0.05). On the contrary, compared with the NI group, NIS mRNA levels and protein expression in both 10HI and 50HI groups tended to decrease, but only the 50HI group decreased significantly (P < 0.05). However, Pendrin didn’t appear to be affected by iodine status in the small intestine (Fig. 2e and g) and kidney (Fig. 3e and g).
The cell membrane protein localization/expression and mRNA level of NIS and Pendrin in the intestine. Localization of NIS (a) and Pendrin (b) in the intestine. Scale bars: 50 μm. c Representative western blot of NIS and Pendrin in the intestine. Bar graphs show the semi-quantitative levels of NIS (d) and Pendrin (e) as determined by band density analysis. Values were shown as mean ± SD, n = 6 per group, comparisons among different groups were performed by one-way ANOVA and followed by an LSD test for multiple comparisons. #P < 0.05 compared with the NI group
The cell membrane protein localization/expression and mRNA level of NIS and Pendrin in the kidney. Localization of NIS (a) and Pendrin (b) in the kidney. Scale bars: 50 μm. c Representative western blot of NIS and Pendrin in the kidney. Bar graphs show the semi-quantitative levels of NIS (d) and Pendrin (e) as determined by band density analysis. Values were shown as mean ± SD, n = 6 per group, comparisons among different groups were performed by one-way ANOVA and followed by an LSD test for multiple comparisons. #P < 0.05 compared with the NI group
Iodine storage in thyroid and placenta in pregnant rats with different iodine intakes
To verify if the body stores more iodine when iodine intake increases, we further examined iodine concentration and storage in the thyroid and placenta. As shown in Table 2, the iodine concentration and storage in the thyroid and placenta were both positively correlated with iodine intake. Though it was lower in the placenta when compared to the thyroid, the 50HI group was significantly higher than the NI group (P < 0.05).
Compensatory effects of thyroid and placenta on iodine deficiency and iodine excess
We also tested the localization of NIS and Pendrin in the thyroid (Fig. 4a, b) and placenta (Fig. 5a, b). NIS, Pendrin gene, and protein expression levels in the thyroid and placenta were tested. The protein expression and mRNA levels of NIS and Pendrin in the thyroid (Fig. 4d and f) and placenta (Fig. 5d and f) in the LI group were significantly higher than those in the NI group (P < 0.05). However, that both 10HI and 50HI groups tended to decrease, but only the 50HI group decreased significantly (P < 0.05).
The cell membrane protein localization/expression and mRNA level of NIS and Pendrin in the thyroid. Localization of NIS (a) and Pendrin (b) in the thyroid. Scale bars: 50 μm. c Representative western blot of NIS and Pendrin in the thyroid. Bar graphs show the semiquantitative levels of NIS (d) and Pendrin (e) as determined by band density analysis. Values were shown as mean ± SD, n = 6 per group, comparisons among different groups were performed by one-way ANOVA and followed by an LSD test for multiple comparisons. #P < 0.05 compared with the NI group
The cell membrane protein localization/expression and mRNA level of NIS and Pendrin in the placenta. Localization of NIS (a) and Pendrin (b) in the placenta. Scale bars: 50 μm. c Representative western blot of NIS and Pendrin in the placenta. Bar graphs show the semiquantitative levels of NIS (d) and Pendrin (e) as determined by band density analysis. Values were shown as mean ± SD, n = 6 per group, comparisons among different groups were performed by one-way ANOVA and followed by an LSD test for multiple comparisons. #P < 0.05 compared with the NI group
Discussion
The metabolism experiments are a classic design used to define nutrient requirements. By assessing total nutrient intake and excretion, nutrient retention can be calculated and the minimum daily intake required to achieve the balance status can be determined [24]. This intake level is an important reference for EAR. The human body is a multi-organ system that maintains iodine homeostasis by regulating the absorption, storage, and excretion of iodine. To overcome the deficiency of only observing iodine intake and excretion in population studies, iodine metabolism experiments in pregnant rats were carried out to observe iodine storage and transport mechanisms in the body. The novelty of this study is that the small intestine, thyroid, placenta, and kidneys, which are responsible for iodine absorption, storage, and excretion, were studied simultaneously. This study provides a theoretical basis for the formulation of EAR. The iodide atom (I−), an electron donor (I−), functions as a reducing agent and is oxidized by specialized peroxidase enzymes to generate thyroid hormones [25]. Thyroid hormones are critical for life in all vertebrates and have essential roles in development, growth, metamorphosis, and metabolism [1]. The mechanism of iodine homeostasis during pregnancy was discussed for the first time, which also provided a new idea for the homeostasis study of other elements.
The flow chart describes the mechanism of iodine homeostasis during pregnancy in the case of iodine deficiency and excess. When iodine is excessive, NIS levels in the small intestine decrease, which reduces the absorption capacity of iodine in the intestine. Excessive iodine in the blood reduces NIS and Pendrin levels in the placenta and thyroid and impairs NIS and Pendrin’s ability to transport iodine. Meanwhile, the level of NIS in the kidney also decreased, reducing the reabsorption of renal iodine. When iodine is deficient, the situation is reversed
The body regulates the absorption of iodine through the small intestine
Dietary iodine is absorbed into the blood through the small intestine and is excreted through the kidneys [21]. NIS and Pendrin are major iodine transporters, which control the entry of iodine into various organs. In this study, unabsorbed iodine by the small intestine was reflected by detecting iodine content in feces. FIE in the 50HI group was significantly increased compared with the NI group, indicating that iodine was not fully absorbed by the small intestine when the intake was severely excessive.
NIS was expressed in small intestinal epithelial cells, and iodine uptake in these cells was also kinetically similar to that in thyrocytes [26]. Excessive iodine concentration reduced iodine uptake potentially by increasing NIS protein degradation and decreasing NIS mRNA levels [13]. Our results found that both NIS and Pendrin were expressed in the intestine epithelial cell, but Pendrin expression didn’t seem to be regulated by iodine. The current study found that Pendrin is highly expressed in the kidney, thyroid, and inner ear epithelia. Systemic pH, aldosterone, angiotensin II, and Cl− levels regulate the activity of pendrin [27]. However, no studies have focused on the expression of pendrin in the small intestine and its regulatory mechanism. This study detected the expression of pendrin protein in the small intestine for the first time.
The body regulates iodine storage through the thyroid and placenta
The thyroid is an important storage organ of iodine in the body. Iodine is transported by NIS at the basolateral membrane of the thyrocytes and diffuses by the exchanger of pendrin to the lumen at the apical membrane [18]. When iodine concentration is too high, excessive iodine inhibits the expression of NIS and Pendrin. Then iodine is blocked from entering cells, and the thyroid regulates the amount of iodine of entry through this mechanism [18]. When iodine is deficient, a positive correlation was observed between thyroid NIS expression and the degree of iodine deficiency [20]. However, the expression of Pendrin in the thyroid under iodine deficiency has not been reported much. For pregnant women, iodine is stored not only in the thyroid but also in the placenta to transport to fetus[28]. Previous research and this study have shown that dietary iodine levels could influence iodine storage in the placenta [29]. In previous reports, both NIS and Pendrin could be expressed in the placenta as iodine transporters, although at low levels compared within the thyroid tissue [30,31,32]. In iodine-deficient rats, the expression of glycosylated NIS and Pendrin proteins increased in the placental labyrinth, and the mRNA levels of NIS and Pendrin were not significantly different from those with appropriate iodine status in the placental labyrinth [20]. In another report, the upregulation of NIS mRNA in the fetal side of the placenta was also demonstrated in rats on a low-iodine diet [20, 33]. Huika Li et al. used the human choriocarcinoma Noma BeWo cell line as a human trophoblast cell model, and the research showed that iodide inhibited NIS mRNA and membrane protein expression but had no effects on Pendrin expression. Iodide also reduced hCG-stimulated NIS expression [34].
Slightly different from previous studies, we found that protein expression and mRNA levels in both NIS and Pendrin decreased with increased iodine intake in the thyroid and placenta. Surprisingly, the amount of iodine stored in the thyroid and placenta was positively correlated with iodine intake (Table 2). In other words, when iodine is deficient, the iodine in the mother's body would be more enriched in the placenta by increasing NIS and Pendrin expression, thus alleviating the harm of iodine deficiency to the fetus. When iodine is excessive, the placenta acts as a barrier, reducing the accumulation of iodine in the placenta by decreasing NIS and Pendrin expression. Similarly, the thyroid can also regulate NIS and Pendrin expression according to different iodine concentrations, thereby regulating thyroid iodine storage to maintain normal thyroid function.
The body regulates iodine reabsorption through the kidney
Past research has shown that functional full-length human-NIS RNA and protein expression have been demonstrated in the tubular system of the kidney, and the NIS may be involved in iodine transport in the kidney [21]. There are few studies on the regulation mechanism of NIS expression in the kidney. However, Pendrin plays an important role in acid–base metabolism as an exchange of chloride and bicarbonate in β-intercalated cells in the kidney [21]. Whether Pendrin is associated with iodine transport in the kidney is unclear. We found that both NIS and Pendrin were expressed in the kidney, but Pendrin expression didn’t seem to be regulated by iodine (Fig. 2). Therefore, we hypothesized that iodine regulation in the kidney mainly depends on NIS rather than Pendrin.
UIE is generally thought of as iodine excreted by the body through kidney filtration or the iodine that has not been reabsorbed by renal tubules. According to our results, there was no significant change in UIE in the LI group and the 10HI group, but UIE in the 50HI group increased significantly compared with the NI group. Therefore, we hypothesized that the kidney can regulate iodine metabolism by regulating NIS expression levels in renal tubules. When iodine is excessive, NIS expression is decreased, the level of iodine reabsorption is decreased, and excreted iodine is increased; when iodine is deficient, the opposite is true. When iodine intake is severely excessive, the pregnant woman does not completely excrete the excess iodine, which is stored in the thyroid and placenta.
Conclusion
In this study, the absorption, storage, and excretion of iodine and the expression levels of the iodine transporters NIS and Pendrin in the small intestine, thyroid, placenta, and kidney were measured in pregnant rats under different iodine nutritional states. Iodine excretion and iodine stores in the placenta and thyroid gland are positively correlated with iodine intake. NIS and Pendrin are also regulated by iodine intake.
We hypothesize that when iodine is deficient or excessive, the body regulates the absorption, storage, and excretion of iodine through the coordination of iodine transporters in the small intestine, thyroid, placenta, and kidney, thus maintaining iodine homeostasis (Fig. 6).
Availability of data and materials
All data are available by reasonable request from the corresponding author.
References
Andersson M, Braegger CP (2022) The role of iodine for thyroid function in lactating women and infants. Endocr Rev 43(3):469–506. https://doi.org/10.1210/endrev/bnab029
Pearce EN, Lazarus JH, Moreno-Reyes R, Zimmermann MB (2016) Consequences of iodine deficiency and excess in pregnant women: an overview of current knowns and unknowns. Am J Clin Nutr 104(3):918S-923S. https://doi.org/10.3945/ajcn.115.110429
Zimmermann MB (2009) Iodine deficiency. Endocr Rev 30(4):376–408. https://doi.org/10.1210/er.2009-0011
Zimmermann MB, Boelaert K (2015) Iodine deficiency and thyroid disorders. Lancet Diabetes Endocrinol 3(4):286–295. https://doi.org/10.1016/s2213-8587(14)70225-6
Abel MH, Caspersen IH, Meltzer HM, Haugen M, Brandlistuen RE, Aase H, Alexander J, Torheim LE, Brantsæter AL (2017) Suboptimal maternal iodine intake is associated with impaired child neurodevelopment at 3 years of age in the Norwegian mother and child cohort study. J Nutr 147(7):1314–1324. https://doi.org/10.3945/jn.117.250456
Abel MH, Ystrom E, Caspersen IH, Meltzer HM, Aase H, Torheim LE, Askeland RB, Reichborn-Kjennerud T, Brantsæter AL (2017) Maternal iodine intake and offspring attention-deficit/hyperactivity disorder: results from a large prospective cohort study. Nutrients. https://doi.org/10.3390/nu9111239
Thomas Jde V, Collett-Solberg PF (2009) Perinatal goiter with increased iodine uptake and hypothyroidism due to excess maternal iodine ingestion. Horm Res 72(6):344–347. https://doi.org/10.1159/000249162
Dworkin HJ, Jacquez JA, Beierwaltes WH (1966) Relationship of iodine ingestion to iodine excretion in pregnancy. J Clin Endocrinol Metab 26(12):1329–1342. https://doi.org/10.1210/jcem-26-12-1329
Chen W, Wang W, Gao M, Chen Y, Guo W, Dong S, Sun H, Pan Z, Pearce EN, Tan L, Shen J, Zhang W (2023) Iodine intakes of <150 μg/day or >550 μg/day are not recommended during pregnancy: a balance study. J Nutr 153(7):2041–2050. https://doi.org/10.1016/j.tjnut.2022.10.017
Lacroix L, Mian C, Caillou B, Talbot M, Filetti S, Schlumberger M, Bidart JM (2001) Na+/I− symporter and Pendred syndrome gene and protein expressions in human extra-thyroidal tissues. Eur J Endocrinol 144(3):297–302. https://doi.org/10.1530/eje.0.1440297
De la Vieja A, Santisteban P (2018) Role of iodide metabolism in physiology and cancer. Endocr Relat Cancer 25(4):R225-r245. https://doi.org/10.1530/erc-17-0515
Portulano C, Paroder-Belenitsky M, Carrasco N (2014) The Na+/I− symporter (NIS): mechanism and medical impact. Endocr Rev 35(1):106–149. https://doi.org/10.1210/er.2012-1036
Nicola JP, Reyna-Neyra A, Carrasco N, Masini-Repiso AM (2012) Dietary iodide controls its own absorption through post-transcriptional regulation of the intestinal Na+/I− symporter. J Physiol 590(23):6013–6026. https://doi.org/10.1113/jphysiol.2012.241307
Bizhanova A, Kopp P (2009) Minireview: the sodium-iodide symporter NIS and Pendrin in iodide homeostasis of the thyroid. Endocrinology 150(3):1084–1090. https://doi.org/10.1210/en.2008-1437
Karaoglan M, İşbilen E (2021) The role of placental iodine storage in the neonatal thyroid stimulating hormone surge: iodine as a driving force to adapt the terrestrial life. J Endocrinol Invest 44(5):1041–1052. https://doi.org/10.1007/s40618-020-01399-y
Neven KY, Marien CBD, Janssen BG, Roels HA, Waegeneers N, Nawrot TS, Ruttens A (2020) Variability of iodine concentrations in the human placenta. Sci Rep 10(1):161. https://doi.org/10.1038/s41598-019-56775-3
Neven KY, Cox B, Vrijens K, Plusquin M, Roels HA, Ruttens A, Nawrot TS (2020) Determinants of placental iodine concentrations in a mild-to-moderate iodine-deficient population: an ENVIRONAGE cohort study. J Transl Med 18(1):426. https://doi.org/10.1186/s12967-020-02601-8
Chen XY, Lin CH, Yang LH, Li WG, Zhang JW, Zheng WW, Wang X, Qian J, Huang JL, Lei YX (2016) The effect on sodium/iodide symporter and Pendrin in thyroid colloid retention developed by excess iodide intake. Biol Trace Elem Res 172(1):193–200. https://doi.org/10.1007/s12011-015-0580-4
Suzuki K, Kimura H, Wu H, Kudo N, Kim WB, Suzuki S, Yoshida A, Caturegli P, Kohn LD (2010) Excess iodide decreases transcription of NIS and VEGF genes in rat FRTL-5 thyroid cells. Biochem Biophys Res Commun 393(2):286–290. https://doi.org/10.1016/j.bbrc.2010.01.123
Sun Y, Han Y, Qian M, Li Y, Ye Y, Lin L, Liu Y (2021) Defending effects of iodide transfer in placental barrier against maternal iodine deficiency. Thyroid 31(3):509–518. https://doi.org/10.1089/thy.2020.0510
Spitzweg C, Dutton CM, Castro MR, Bergert ER, Goellner JR, Heufelder AE, Morris JC (2001) Expression of the sodium iodide symporter in human kidney. Kidney Int 59(3):1013–1023. https://doi.org/10.1046/j.1523-1755.2001.0590031013.x
Li N, Jiang Y, Shan Z, Teng W (2012) Prolonged high iodine intake is associated with inhibition of type 2 deiodinase activity in pituitary and elevation of serum thyrotropin levels. Br J Nutr 107(5):674–682. https://doi.org/10.1017/s0007114511003552
Serrano-Nascimento C, Salgueiro RB, Pantaleão T, Corrêa da Costa VM, Nunes MT (2017) Maternal exposure to iodine excess throughout pregnancy and lactation induces hypothyroidism in adult male rat offspring. Sci Rep 7(1):15591. https://doi.org/10.1038/s41598-017-15529-9
Guo W, Yang Y, Jiang W, Cheng Y, Wu W, Pan Z, Zhang D, Li S, Ren Z, Zhang N, Zhang K, Pearce EN, Chen W, Zhang W (2023) An iodine balance study in Chinese school-age children. J Clin Endocrinol Metab 108(10):e949–e955. https://doi.org/10.1210/clinem/dgad244
Kessler J, Hooge D (2007) Aqueous iodine equilibria in Mammalian iodination reactions. Thyroid 17(1):19–24. https://doi.org/10.1089/thy.2006.0243
Altorjay A, Dohán O, Szilágyi A, Paroder M, Wapnir IL, Carrasco N (2007) Expression of the Na+/I− symporter (NIS) is markedly decreased or absent in gastric cancer and intestinal metaplastic mucosa of Barrett esophagus. BMC Cancer 7:5–5. https://doi.org/10.1186/1471-2407-7-5
Rozenfeld J, Efrati E, Adler L, Tal O, Carrithers SL, Alper SL, Zelikovic I (2011) Transcriptional regulation of the Pendrin gene. Cell Physiol Biochem 28(3):385–396. https://doi.org/10.1159/000335100
Burns R, O’Herlihy C, Smyth PP (2011) The placenta as a compensatory iodine storage organ. Thyroid 21(5):541–546. https://doi.org/10.1089/thy.2010.0203
Burns R, Azizi F, Hedayati M, Mirmiran P, O’Herlihy C, Smyth PP (2011) Is placental iodine content related to dietary iodine intake? Clin Endocrinol (Oxf) 75(2):261–264. https://doi.org/10.1111/j.1365-2265.2011.04039.x
Mitchell AM, Manley SW, Morris JC, Powell KA, Bergert ER, Mortimer RH (2001) Sodium iodide symporter (NIS) gene expression in human placenta. Placenta 22(2–3):256–258. https://doi.org/10.1053/plac.2000.0609
Bidart JM, Lacroix L, Evain-Brion D, Caillou B, Lazar V, Frydman R, Bellet D, Filetti S, Schlumberger M (2000) Expression of Na+/I− symporter and Pendred syndrome genes in trophoblast cells. J Clin Endocrinol Metab 85(11):4367–4372. https://doi.org/10.1210/jcem.85.11.6969
Andersen SL, Nøhr SB, Wu CS, Olsen J, Pedersen KM, Laurberg P (2013) Thyroglobulin in smoking mothers and their newborns at delivery suggests autoregulation of placental iodide transport overcoming thiocyanate inhibition. Eur J Endocrinol 168(5):723–731. https://doi.org/10.1530/eje-12-0759
Schröder-van der Elst JP, van der Heide D, Kastelijn J, Rousset B, Obregón MJ (2001) The expression of the sodium/iodide symporter is up-regulated in the thyroid of fetuses of iodine-deficient rats. Endocrinology 142(9):3736–3741. https://doi.org/10.1210/endo.142.9.8377
Li H, Richard K, McKinnon B, Mortimer RH (2007) Effect of iodide on human choriogonadotropin, sodium-iodide symporter expression, and iodide uptake in BeWo choriocarcinoma cells. J Clin Endocrinol Metab 92(10):4046–4051. https://doi.org/10.1210/jc.2006-2358
Funding
This work study was funded by the National Natural Science Foundation of China (NSFC Grant nos. 81920108031).
Author information
Authors and Affiliations
Contributions
WZ and MF contributed to the study conception and design. MF, HZ, YG, RY, QJ, QM, YQ, and NS performed the experiments. Data analysis was performed by MF, YG, and QM. The first draft of the manuscript was written by MF and YG. RY checks the manuscript. All authors commented on previous versions of the manuscript; All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
The Tianjin Hospital of ITCWM Nankai Hospital Animal Ethics Committee approved all the experimental procedures (NKYY-DWLL-2021-048).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fu, M., Zhang, H., Gao, Y. et al. Mechanism of multi-organ compensation under different iodine intake in pregnant rats: results from a repeated-measures study of iodine metabolism. Eur J Nutr 63, 589–598 (2024). https://doi.org/10.1007/s00394-023-03288-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-023-03288-5