Abstract
Objective
In distinguishing urate arthritis (UA) from non-crystal-related arthritides, joint sonography including the detection of the double contour sign (DCS) and hypervascularization using power Doppler ultrasound (PDUS) is an important step in the diagnostic process. But are these sonographic features equally reliable in every accessible joint under real-life conditions?
Methods
We retrospectively analyzed 362 patients with acute arthritis and evaluated the DCS and the degree of PDUS hypervascularization in patients with gout and in those with arthritis other than urate arthritis (non-UA). We classified all joints into the groups small, medium, and large. Sensitivities, specificities, positive and negative predictive values (PPV/NPV), and a binary regression model were calculated. We also evaluated the influence of serum uric acid levels (SUA) on the presence of a DCS in each joint category.
Results
Sensitivity of the DCS in gout was 72.5% in the entire cohort, 66.0% in large, 78.8% in medium, and 72.3% in small joints. In wrist joints the DCS sensitivity maxed at 83.3%, with a specificity of 81.8%. The lowest rates of DCS sensitivity were found in gout patients with elbow joint involvement (42.9%). In all joints except metatarsophalangeal joint 1 (MTP-1), the incidence of a DCS increased by the increment of SUA levels above 7.5 mg/dl (p < 0.001). PDUS signals were most commonly found in medium and small joints and were only scarce in large joints, independent of the underlying diagnosis.
Conclusions
In our study we detected different rates of accuracy regarding DCS and PDUS in patients with acute arthritis. The best results were seen in medium-size joints, especially wrists.
Zusammenfassung
Ziel
Bei der Unterscheidung zwischen Gichtarthritis und nichtkristallassoziierten Arthritiden ist die Arthrosonographie zur Detektion des Doppelkonturzeichens (DCS) und der Hypervaskularisation im Power-Doppler-Ultraschall (PDUS) ein wichtiger Schritt im diagnostischen Prozess. Aber sind diese sonographischen Zeichen unter Alltagsbedingungen gleichsam zuverlässig in allen untersuchbaren Gelenken?
Methoden
Retrospektiv wurden die Daten von 362 Patienten mit akuter Arthritis und das DCS analysiert sowie die Hypervaskularisation im PDUS bei Fällen mit Uratarthritis (UA) vs. Nichturatarthritis (non-UA) ausgewertet. Alle Gelenke wurden der Größe nach in klein, mittel und groß eingeordnet. Es wurden Sensitivitäten, Spezifitäten, positive und negative prädiktive Werte und eine binäre Regression kalkuliert. Außerdem werteten die Autoren den Einfluss der Serumharnsäure auf die Detektierbarkeit eines DCS in jeder Gelenkkategorie aus.
Ergebnisse
Die Sensitivität des DCS bei Gicht in der gesamten Kohorte lag bei 72,5 %, bei großen Gelenken bei 66,0 %, bei mittleren betrug sie 78,8 % und bei kleinen 72,3 %. Die beste Sensitivität war bei Handgelenken mit 83,3 % bei einer Spezifität von 81,8 % zu verzeichnen. Die niedrigste Sensitivität fanden die Autoren bei Ellbogenmanifestation (42,9 %). Bei allen Gelenken außer dem Metatarsophalangealgelenk 1 (MTP-1) war die Inzidenz eines DCS bei Serumharnsäurewerten >7,5 mg/dl signifikant erhöht (p < 0,001). PDUS-Signale wurden unabhängig von der Diagnose am häufigsten bei mittleren und kleinen, dagegen kaum bei großen Gelenken gefunden.
Schlussfolgerungen
In der vorliegenden Studie war die Genauigkeit der Vorhersage einer Gichtarthritis durch das DCS sowie das Auftreten von PDUS-Hypervaskularität je nach Gelenk unterschiedlich. Die besten Ergebnisse wurden in mittelgroßen Gelenken, insbesondere Handgelenken, erzielt.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In acute arthritis the sonographic joint examination is an important diagnostic element. Urate arthritis (UA) can be identified sonographically by the detection of the double contour sign (DCS), which, according to the OMERACT definition, is an abnormal hyperechoic band over the superficial margin of cartilage, independent of the angle of insonation, and which may be either irregular or regular, continuous or intermittent, and can be distinguished from the cartilage interface sign [1,2,3,4].
The DCS in gout has been proven to be of good sensitivity and high specificity [1, 5, 6], which can be further increased by adding information from the degree of hypervascularization in power Doppler ultrasound (PDUS) and serum uric acid (SUA) levels [7]. In gout, the DCS is a visual depiction of monosodium urate (MSU) crystal deposition on the cartilage surface and is therefore mainly present in patients with elevated SUA levels [2, 7]. It is independent from the joint’s inflammatory state and can be present in inter-critical stages of the disease [8]. Furthermore, it has been shown that the DCS can dissolve under a urate-lowering therapy [9, 10].
Due to the preference of lower limb joints in gouty arthritis, the metatarsophalangeal (MTP)-1 and the knee joints have been the main focus of many studies investigating the DCS [11,12,13]. We pursued the question of whether the DCS is equally reliable in every joint or whether there are preferences of appearance.
Little is known about the value of ultrasonographic findings when patients present with acute arthritis in any joint of the body under natural real-life conditions. We therefore evaluated patients with acute mono- or oligoarthritis regarding the presence of DCS and degree of PDUS hypervascularization, and analyzed whether these findings differ between different joints and joint sizes. We furthermore investigated the influence of SUA levels on the detectability of the DCS in every joint category.
Methods
Patients and study design
In this bicentric study we retrospectively evaluated 475 patients who presented to our departments with their first episode of acute mono- or oligoarthritis within the daily hospital routine between 2012 and 2015. We performed joint sonography including PDUS in all patients. In cases with more than one joint involved, the investigation of the clinically most severely affected joint was included in this study. At the time of presentation the patients’ blood specimens were analyzed for SUA (normal range <7.0 mg/dl or <416 µmol/l), C‑reactive protein (CRP; normal range <5 mg/l), and erythrocyte sedimentation rate (ESR; normal range <15 mm after one hour). Whenever possible, patients underwent joint needle aspiration for synovial fluid analysis. None of the patients were under immunosuppressive or urate-lowering treatment at the time of the investigation.
We divided our study cohort into two groups: (1) urate arthritis (UA) and (2) arthritides other than gout (non-UA). The second group was comprised of non-crystal-related inflammatory arthritides such as rheumatoid arthritis (RA), psoriatic arthritis (PsA), spondyloarthritis, connective tissue diseases, and others. Patients with calcium pyrophosphate deposition disease (CPPD) proven by synovial fluid analysis were excluded from the study. This was necessary because joints in CPPD can present with a quasi or pseudo DCS in joint ultrasound that—despite characteristic sonographic distinctiveness—in some cases can be mistaken for a gout DCS [1, 5, 7]. In order to assess the reliability of the gout DCS, CPPD cases had to be excluded.
The affected joints were classified into three groups according to their size: small joints (metacarpophalangeal, MCP; proximal and distal interphalangeal, PIP/DIP; metatarsophalangeal joints, MTP), medium joints (wrist, elbow, ankle joints), and large joints (shoulder, hip, knee joints).
The study was undertaken according to the Helsinki Declaration on clinical studies. We additionally obtained approval of the local ethics committee (Medizinische Ethikkommission II, Universitätsmedizin Mannheim, approval no. 2016-868R-MA).
Joint sonography
A total of three rheumatologists performed the ultrasound examinations. All investigators were experienced, well trained, and joint sonographers certified by the German Society of Ultrasound in Medicine (DEGUM), two of whom were DEGUM levels 2 and 3 (3 being the highest level of expertise, i. e., ultrasound trainer). There was no blinded second-look investigation. Uncertain cases were debated on site and a team consensus was reached before the sonographic examination was finalized. In all cases, the ultrasound took place before the analyses of blood specimens, joint needle aspiration, and prior to treatment initiation. Thus, the sonographers were unaware of laboratory results.
We used an Aplio 400 (Toshiba, Minato, Japan) and a EUB-7500 (Hitachi, Tokio, Japan) ultrasound device, each equipped with a high-frequency (7–14 MHz) linear transducer head. Both devices are state-of-the-art and are explicitly recommended by the DEGUM for high-standard sonography for level 3 standards (www.degum.de).
An irregular hyperechoic band over the superficial margin of the hyaline cartilage which was independent of the angle of insonation was classified as double contour sign (DCS). Tophi, extraarticular hyperechoic deposits, and tendon pathologies were not included in the evaluation.
Wrists and MCP joints were scanned in ventral and dorsal planes, MTP-1 joints in dorsal planes only to avoid detection of false DC signs as described in [14]. We investigated the lateral and transversal axes of knee joints in extension and maximum flexion, focusing on the suprapatellar recess and the tibial condyles. Ankle joints were examined in longitudinal and transversal planes ranging from the lateral to the medial malleolus, elbows in the anterior and posterior aspect including the medial and lateral epicondyle. Shoulders were scanned from posterior, lateral, and ventral planes in longitudinal and transversal axes, each including axillary access and the analysis of the long biceps tendon. All joints were examined in a resting state as well as dynamically, i. e., under passive movement applied by the sonographer.
Synovial fluid analysis
When technically feasible and where written consent had been obtained, patients underwent synovial fluid analysis by needle aspiration of the investigated joint for standard workup. Synovial fluid specimens were analyzed by a pathologist using polarizing microscopy. The presence of MSU crystals was diagnostic for gout, that of calcium pyrophosphate (CPP) crystals for CPPD. In order to prove synovial inflammation, the synovial white blood count (sWBC, numbers of leukocytes/nl) was determined using the automated blood hematology analyzer XE-2100 (Sysmex, Japan). Synovial fluids with sWBC of 2.0/nl or greater were considered to be inflammatory. When sufficient material was obtainable, all synovial fluid specimens additionally underwent Gram staining and microbiologic assessment.
Diagnoses
All patients were newly diagnosed at the time of the investigation. The diagnosis of gout was established according to the 2015 ACR/EULAR gout classification criteria [15], which also include non-invasive diagnostic elements for cases in which synovial fluid analysis is not available or not feasible. The diseases in the non-UA group were classified according to their respective ACR/EULAR classification criteria.
Statistical analyses
Statistical analyses were performed with SPSS v11.5 (IBM, Armonk, NY, USA). We used t-tests for comparison of parametric variables with normal distribution and Mann–Whitney U test for non-parametric variables without normal distribution. We furthermore calculated sensitivities, specificities, and positive and negative predictive values (PPV, NPV) of the DCS in each joint and joint size by chi-square confusion matrixes. The influence of joint type and size on the appearance of the DCS was evaluated by correlation analyses (Pearson and Spearman coefficient). We applied a binary logistic regression model to exclude confounding variables. Statistical significance was defined as a two-tailed p < 0.05.
Results
General
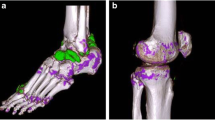
From the 475 patients screened, 24 were excluded from the study due to incomplete data. Another 89 cases were dismissed because synovial fluid analysis showed CPP crystals, leading to the diagnosis of CPPD as presented in Fig. 1. The remaining 362 cases showed a male to female ratio of 1:0.77. The mean age of our cohort was 62 ± 17 years (range 18–93 years). 39.5% of the patients suffered from UA. Patient baseline characteristics are shown in Table 1.
177 of the 362 investigated joints were knees (48.9%), followed by ankle (18.5%) and wrist joints (9.4%). Henceforth, in our cohort, the three joint size categories large/medium/small were distributed as follows: 52.8/32.6/14.6%. We performed joint paracentesis with synovial fluid analysis in about two thirds of all cases (245/362, 67.7%). A complete depiction of the joint categories involved in our cohort can be found in Fig. 2.
Joint size and underlying diagnosis
From 143 gout cases in our study, 48 (33.6%) were small, 50 (35.0%) were medium, and 45 (31.5%) were large joints. In contrast to this relatively balanced distribution, small joints were by far the fewest among non-UA patients. Here the partition (small/medium/large) was 5 (2.2%)/68 (31.5%)/146 (66.7%). The data are visualized in Fig. 3.
Prediction of gout by DCS and impact of joint size
The overall sensitivity of the DCS in gout was 72.5% in our study, showing a specificity of 80.8%.
We observed a moderate sensitivity of the DCS in large joints (66.0%), most prominently represented by knee joints. The specificity was 85.1%, with a PPV and NPV of 64.7 and 87.6%, respectively.
Medium-size joints showed a DCS sensitivity of 78.8%, which was markedly higher than in small or large joints. Among medium-size joints the best sensitivity was observed in wrist (83.3%) and ankle joints (84.8%), whereas specificity was equally satisfying in the former (81.8%) but remarkably low in the latter (58.8%). The PPV of the DCS in a wrist joint was about 71% in our cohort, and for medium-size joints in general 69.5%. The DCS correctly detected gouty arthritis in elbow joints in only 42.9% of all cases.
In small joints such as MTP-1 and MCP joints, the DCS presented with a moderate sensitivity of 72.3% (MTP-1 72.0% and MCP 72.7%), but was accentuated by a high PPV of 94% paired with a low NPV of 23.5%. In a binary logistic regression model the predictability of a CRA by a double contour was strongest for small joints (p < 0.001, 95% CI 3.093-32.345, Exp(B) 10.0).
A complete overview of all results regarding DCS in the various joint types and sizes is displayed in Table 2.
Degree of hypervascularization and joint size
Large joints tended to present with lesser degrees of vascularization (°0 and °1), whereas hypervascularization degrees 2 and 3 were more often associated with medium and small joints (p < 0.001). These findings established by non-parametric tests were confirmed by a logistic regression analysis (p < 0.05, 95% CI 1.079–2.316, Exp(B) 1.6) and are shown in Fig. 3.
DCS and SUA levels
We investigated the influence of SUA levels on the appearance of the DCS for each joint. Mean SUA levels in DCS+ patients were 8.7 ± 3.7 mg/dl vs. 5.8 ± 2.4 mg/dl in DCS− patients (p < 0.001, 95% CI 2.216–3.636).
In cases with SUA levels <7.5 mg/dl, DCS+ and DCS− patients were almost equally common in small and medium-size joints (small: 43.5% DCS+, medium: 49.4% DCS+). In large joints, however, DCS− patients outweighed DCS+ patients (30.4% DCS+). In cases with SUA levels ≥7.5 mg/dl, joints of all sizes showed a strong and statistically significant increment of DCS incidence (small: 74.4% DCS+, p < 0.05; medium: 71.7% DCS+, p < 0.05; large: 58.9%, p < 0.001).
This observation was especially noteworthy in MCP joints, in which the DCS incidence increased from 11 to 77.3% (p < 0.001) when comparing patients with SUA levels < and ≥7.5 mg/dl.
As displayed in Fig. 4, the incidence of the DCS in MTP-1 joints did not show significant differences between the two SUA level groups (69.2% DCS+ in SUA <7.5 mg/dl vs. 75.0% DCS+ in SUA ≥7.5 mg/dl; p = 0.730).
Discussion
In our retrospective study we analyzed 362 joints from patients who presented themselves to our rheumatology departments with acute arthritis. It was our goal to determine the accuracy of the DCS and of PDUS based vascularization in different joints and joint sizes comparing UA to non-UA patients in the state of acute inflammation.
Most existing studies based their work on a predefined set of joints, mostly MTP-1 and knee joints; others performed their examination in an inter-critical state of gouty arthritis in patients with a known history of hyperuricemia and gout [3, 8, 16,17,18,19,20]. A major strength of our study is that the investigation that took place under natural real-life conditions involving patients with acutely flaring diseases without pre-known established rheumatological diagnoses.
The DCS has been associated with a good sensitivity and high specificity for UA in multiple preceding publications. In our cohort its overall sensitivity was about 73%, which is rather low compared to the results of other authors [3, 21].
After having evaluated each joint and joint size separately, our data suggest that the DCS achieves the best sensitivity in medium-size joints (79%), and among medium-size joints the wrist and ankle joints are particularly good (83 and 85%).
Even in the MTP-1 joint—the most prominent joint in UA [11, 13]—we could not find a higher sensitivity (72%). The reason for the rather moderate overall DCS sensitivity in our cohort is therefore due to the investigated elbow and shoulder joints, despite their low numbers.
Other authors have investigated multiple joint sites and in part confirm our results: In the work of Roddy, only a small minority of gout patients had a DCS in elbow joints (10%) and—in contrast to our findings—in wrists (2%). In this study, a high rate of inter-critical gout patients were included. Also, non-affected joints were involved in the investigation [12]. Naredo et al. found the MTP-1 and MCP-2 joints to be the anatomical sites with the most frequent appearance of a DCS. They propose a multifocal assessment involving tendons and cartilages to optimize sensitivity and specificity. Again, patients with acute disease flares were excluded in this study [20].
In our investigation wrist and ankle joints presented with equally good sensitivities; however, specificity was markedly low in ankles compared to wrists (59 vs. 82%). Joint effusion can create an echogenic reflection on the cartilage surface mimicking a DCS due to a high impedance differential between joint effusion and the tissue below, as well as due to increased sound propagation in fluids increasing the normal echogenicity of the synovia. The result is an image that can be easily mistaken for a true DCS, as demonstrated in Fig. 5. Despite the fact that this phenomenon can occur in all joints, it is our experience that is extraordinarily frequent in the talus of the ankle joint.
Panels a and b show a B-mode sonography of ankle joints in longitudinal axis with joint effusion (asterisk) and double contour signs (DCS; arrows). Both patients underwent synovial fluid analysis. The patient in a was diagnosed with calcium pyrophosphate deposition disease (CPPD) arthritis, the patient in b had arthralgia but no arthritis. The sonographic morphology of the DCS in both cases is indistinguishable
In all joints and joint sizes (except MTP-1), the DCS prevalence was significantly higher in patients with SUA ≥7.5 mg/dl than in those with normal SUA levels as expected. This observation is coherent with what is known on the pathophysiology of urate crystal deposition and the creation of sonographic double contours [2, 22, 23]. Again, this effect was especially strong in medium-size joints.
Interestingly, in MTP-1 joints the DCS prevalence was equally high irrespective of SUA levels. These observations are in line with Roddy and colleagues, who found that the DCS in MTP-1 joints was independent of SUA levels and urate-lowering treatment [12]. Furthermore, it has been shown that the DCS in MTP-1 is likewise present in asymptomatic hyperuricemia or inter-critical gout [11, 12, 24].
We previously demonstrated that crystal-related arthritides present with particularly high degrees of PDUS hypervascularization [7]. In the present study we found PDUS hypervascularization to be more common in medium and small joints and less frequent in knee joints—a finding that is in line with our own investigation in inflammatory hip joints [25]. This observation can in part be explained by technical limitations regarding Doppler signal detection in large joints where the distance between synovial vessels and the transducer head is particularly long [26]. For the clinician this can be important since few or absent PDUS signals might lead to underestimating disease activity in large joints.
The main conclusion that we derive from our data is that the accuracy of sonographic features can vary depending on the joint investigated. A DCS in the wrist is more likely to indicate gouty arthritis than in the ankle joint, and an absent DCS in a shoulder joint argues against gout more strongly than an absent DCS in MTP-1. Likewise, missing PDUS signals in knee joints should not easily be used to rule out a flaring disease, whereas little or no hypervascularization in a wrist joint is suggestive of lesser inflammation. In the workup of patients with acute arthritis, this knowledge can be relevant for the sonographic evaluation, especially when SUA levels are normal, autoimmunological laboratory markers are negative, and a diagnostic joint needle aspiration is not feasible.
There are some mentionable limitations of our work:
Most notably, our analysis is retrospective in design and does not offer prospective, controlled data.
Baseline characteristics of both patient groups differed heavily due to the epidemiologic features of the underlying diseases. Gout patients are usually more likely to be elderly males, whereas other arthritic diseases such as RA, PsA, or systemic lupus erythematosus occur more frequently in younger women [27]. Also, gouty arthritis is characterized by an intensive inflammatory cascade induced by interleukin-1, which explains extraordinarily high levels of CRP, ESR, and sWBC in the UA group [28].
The investigated joint sizes are not equally distributed over the diagnostic groups: The majority of small joints in our cohort were seen in gout patients, whereas in non-UA cases their fraction was only about 2%. This can be explained by the clinical setting. In this study we included the most severely affected joint. In UA patients the most affected joint is more likely to be MTP-1 or a MCP joint, since gout usually presents as mono- or oligoarthritis. In contrast, in a polyarticular disease such as RA, multiple MCP joints might be involved; however, the most prominent joint might be a wrist or a knee.
Not all patients underwent synovial fluid analysis, although this is the gold standard of gout diagnosis. Therefore, a potential risk of misdiagnosis is given.
Furthermore, a total of three sonographers performed the ultrasounds. There was no programmed second-look investigation; hence, our study does not provide for an evaluation of the interobserver reliability.
The data acquisition took place within the standard clinical routine. Thus, the physicians performing the ultrasounds might have been biased regarding the probable diagnosis by the history and the clinical presentation of the patient.
References
Grassi W, Meenagh G, Pascual E, Filippucci E (2006) “Crystal clear”-sonographic assessment of gout and calcium pyrophosphate deposition disease. Semin Arthritis Rheum 36:197–202. https://doi.org/10.1016/j.semarthrit.2006.08.001
Thiele RG, Schlesinger N (2007) Diagnosis of gout by ultrasound. Rheumatology (Oxford) 46:1116–1121. https://doi.org/10.1093/rheumatology/kem058
Ottaviani S, Richette P, Allard A et al (2012) Ultrasonography in gout: a case-control study. Clin Exp Rheumatol 30:499–504
Terslev L, Gutierrez M, Schmidt WA et al (2015) Ultrasound as an outcome measure in gout. A validation process by the OMERACT Ultrasound Working Group. J Rheumatol 42:2177–2181. https://doi.org/10.3899/jrheum.141294
Filippou G, Frediani B, Gallo A et al (2007) A “new” technique for the diagnosis of chondrocalcinosis of the knee: sensitivity and specificity of high-frequency ultrasonography. Ann Rheum Dis 66:1126–1128. https://doi.org/10.1136/ard.2007.069344
Ogdie A, Taylor WJ, Weatherall M et al (2015) Imaging modalities for the classification of gout: systematic literature review and meta-analysis. Ann Rheum Dis 74:1868–1874. https://doi.org/10.1136/annrheumdis-2014-205431
Löffler C, Sattler H, Peters L et al (2015) Distinguishing gouty arthritis from calcium pyrophosphate disease and other arthritides. J Rheumatol 42:513–520. https://doi.org/10.3899/jrheum.140634
Das S, Ghosh A, Ghosh P et al (2017) Sensitivity and specificity of ultrasonographic features of gout in intercritical and chronic phase. Int J Rheum Dis 20:887–893. https://doi.org/10.1111/1756-185X.12928
Ottaviani S, Gill G, Aubrun A et al (2015) Ultrasound in gout: a useful tool for following urate-lowering therapy. Joint Bone Spine 82:42–44. https://doi.org/10.1016/j.jbspin.2014.03.011
Thiele RG, Schlesinger N (2010) Ultrasonography shows disappearance of monosodium urate crystal deposition on hyaline cartilage after sustained normouricemia is achieved. Rheumatol Int 30:495–503. https://doi.org/10.1007/s00296-009-1002-8
Pineda C, Amezcua-Guerra LM, Solano C et al (2011) Joint and tendon subclinical involvement suggestive of gouty arthritis in asymptomatic hyperuricemia: an ultrasound controlled study. Arthritis Res Ther 13:R4. https://doi.org/10.1186/ar3223
Roddy E, Menon A, Hall A et al (2013) Polyarticular sonographic assessment of gout: a hospital-based cross-sectional study. Joint Bone Spine 80:295–300. https://doi.org/10.1016/j.jbspin.2012.09.017
Peiteado D, De Miguel E, Villalba A et al (2012) Value of a short four-joint ultrasound test for gout diagnosis: a pilot study. Clin Exp Rheumatol 30:830–837
Ottaviani S, Bardin T, Richette P (2012) Usefulness of ultrasonography for gout. Joint Bone Spine 79:441–445. https://doi.org/10.1016/j.jbspin.2012.01.012
Neogi T, Jansen TLTA, Dalbeth N et al (2015) 2015 gout classification criteria: an American College of Rheumatology/European League Against Rheumatism Collaborative Initiative. Arthritis Rheumatol 67:2557–2568. https://doi.org/10.1002/art.39254
Wright SA, Filippucci E, McVeigh C et al (2007) High-resolution ultrasonography of the first metatarsal phalangeal joint in gout: a controlled study. Ann Rheum Dis 66:859–864. https://doi.org/10.1136/ard.2006.062802
Filippucci E, Riveros MG, Georgescu D et al (2009) Hyaline cartilage involvement in patients with gout and calcium pyrophosphate deposition disease. An ultrasound study. Osteoarthr Cartil 17(003):178–181. https://doi.org/10.1016/j.joca.2008.06.003
Filippucci E, Scirè CA, Delle Sedie A et al (2010) Ultrasound imaging for the rheumatologist. XXV. Sonographic assessment of the knee in patients with gout and calcium pyrophosphate deposition disease. Clin Exp Rheumatol 28:2–5
Terslev L, Gutierrez M, Christensen R et al (2015) Assessing elementary lesions in gout by ultrasound: results of an OMERACT patient-based agreement and reliability exercise. J Rheumatol 42:2149–2154. https://doi.org/10.3899/jrheum.150366
Naredo E, Uson J, Jiménez-Palop M et al (2014) Ultrasound-detected musculoskeletal urate crystal deposition: which joints and what findings should be assessed for diagnosing gout? Ann Rheum Dis 73:1522–1528. https://doi.org/10.1136/annrheumdis-2013-203487
Lamers-Karnebeek FBG, Van Riel PLCM, Jansen TL (2014) Additive value for ultrasonographic signal in a screening algorithm for patients presenting with acute mono-/oligoarthritis in whom gout is suspected. Clin Rheumatol 33:555–559. https://doi.org/10.1007/s10067-014-2505-6
Sokoloff L (1957) The pathology of gout. Metabolism 6:230–243
Burt HM, Dutt YC (1986) Growth of monosodium urate monohydrate crystals: effect of cartilage and synovial fluid components on in vitro growth rates. Ann Rheum Dis 45:858–864
Stewart S, Dalbeth N, Vandal AC et al (2017) Ultrasound features of the first metatarsophalangeal joint in gout and asymptomatic hyperuricaemia: comparison with normouricaemic individuals. Arthritis Care Res (Hoboken) 69:875–883. https://doi.org/10.1002/acr.23082
Löffler C, Sattler H, Uppenkamp M, Bergner R (2016) Contrast-enhanced ultrasound in coxitis. Joint Bone Spine 83:669–674. https://doi.org/10.1016/j.jbspin.2015.10.012
Song IH, Althoff CE, Hermann KG et al (2008) Knee osteoarthritis. Efficacy of a new method of contrast-enhanced musculoskeletal ultrasonography in detection of synovitis in patients with knee osteoarthritis in comparison with magnetic resonance imaging. Ann Rheum Dis 67:19–25
Mandell BF (2008) Clinical manifestations of hyperuricemia and gout. Cleve Clin J Med 75(Suppl 5):S5–S8
Cronstein BN, Sunkureddi P (2014) Mechanistic aspects of inflammation and clinical management of inflammation in acute gouty arthritis. J Clin Rheumatol 19:19–29. https://doi.org/10.1097/RHU.0b013e31827d8790.Mechanistic
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
C. Löffler, H. Sattler, U. Löffler, B.K. Krämer, and R. Bergner declare that they have no competing interests.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Redaktion
U. Müller-Ladner, Bad Nauheim
U. Lange, Bad Nauheim
Rights and permissions
About this article
Cite this article
Löffler, C., Sattler, H., Löffler, U. et al. Size matters: observations regarding the sonographic double contour sign in different joint sizes in acute gouty arthritis. Z Rheumatol 77, 815–823 (2018). https://doi.org/10.1007/s00393-018-0425-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00393-018-0425-6