Abstract
Background
This study investigated p aclitaxel-induced luminal changes following drug-coated balloon (DCB) angioplasty to treat coronary de novo lesions without additional stenting. DCB-mediated local drug delivery reduces late lumen loss in de novo coronary artery lesions. We performed a retrospective clinical assessment based on a pre-specified quantitative coronary angiography (QCA) protocol.
Methods
QCA was performed for each centre to assess the primary endpoint late lumen changes, i.e. the difference between in-lesion minimal lumen diameter (MLD) at the routine angiographic follow-up as compared to post-procedural in-lesion MLDs. These MLD changes were compared to corresponding reference vessel diameter changes as an intra-patient control.
Results
We evaluated 58 consecutive native coronary artery lesions directly after DCB angioplasty and at a routine target follow-up angiography of 4 months by QCA. Target lesion MLD increased significantly within the 4.1 ± 2.1 month observation period (1.75 ± 0.55 vs. 1.91 ± 0.55 mm, p < 0.001, diameter stenosis 33.8 ± 12.3 vs. 26.9 ± 13.8 %, p < 0.001), while there were no changes in non-target reference vessel diameters (2.33 ± 0.60 vs. 2.34 ± 0.61 mm, p = ns). A total of 69 % of patients showed luminal enlargement whereas 29 % had minor luminal loss.
Conclusion
Local application of paclitaxel by DCB angioplasty to native coronary arteries after pre-dilatation without major dissection and recoil leads to late lumen increase.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Plain old balloon angioplasty (POBA) is currently used in a minority of patients having either contraindications to long-term dual antiplatelet therapy (DAPT) or lesion morphologies unsuitable for stenting. Besides acute vessel occlusion, restenosis is the most serious limitation of POBA. Moreover, POBA is associated with elastic recoil, negative vessel remodelling and intimal hyperplasia.
Because of these adverse outcomes, bare-metal stents (BMS) have been developed which almost completely abandon elastic recoil but provoke neointimal hyperplasia. This in turn motivated the development of drug-eluting stents (DES) to reduce neointimal proliferation [1–4].
Positive vessel remodelling with further increases in post-procedural vessel lumen diameters until angiographic follow-up may also be observed after percutaneous transluminal coronary angioplasty (PTCA) but is seen in the minority of patients [5].
While DCBs were developed to overcome intimal hyperplasia [6, 7] and were first studied in bare-metal stent in-stent restenosis (BMS-ISR) [8–11] with excellent long-term clinical results, application of this technology as a stand alone procedure in de novo lesions was associated with low target lesions revascularization (TLR) rates in large registries [12]. Furthermore, an unanticipated increase in angiographically documented vessel lumen diameters [13] in our institutions during routine follow-ups led to standardized quantitative coronary angiography (QCA) methodology to assess these potential late lumen gains. The aim of this study was to systematically evaluate and quantify potential lumen gains after DCB angioplasty.
Methods
To investigate medium-term angiographic results following DCB interventions, the data bases of two experienced centres with more than 1,000 DCB procedures per annum were retrospectively reviewed. Eligible were patients treated with DCB angioplasty for native coronary artery lesions without additional stenting (‘DCB-only’ strategy) and proper analyzable angiograms at target follow-up of 4 months. According to patho-anatomic evaluations and pharmacologic considerations after ‘DCB-only’ PCI, vessels show healing after 2–3 months (Renu Virmani, personal communication). A sample size calculation was performed prior to our QCA analyses to assess the number of consecutive patients needed to show a pre-specified late lumen gain.
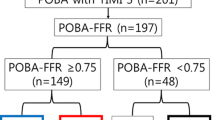
All PCIs with this ‘DCB-only’ approach were performed according to the recommendations of the German Consensus Group [14, 15]. As outlined in these recommendations all lesions were carefully pre-dilated using an uncoated semi-compliant balloon with a balloon to vessel ratio of 0.8–1.0. Only if (1) the coronary flow after this pre-dilation was normal (TIMI III), (2) dissections were absent or minor (class A or B according to the classification of the North American National Heart Lung and Blood Institute (NHLBI) [16] and (3) residual stenosis was ≤30 %, the DCB as a stand alone strategy was chosen. The DCB was used as a drug delivery and as a post-dilatation device with the same diameter as the predilatation balloon with maximum balloon pressures of only 8–10 atm. Attention was paid to avoid geographic mismatch and the DCB was chosen to be at least 5 mm longer than the pre-dilation balloon (2–3 mm on each end). If there was a dissection greater than class B after the DCB dilatation occurred or after it was noticed, a BMS was implanted. These patients (DCB+BMS) as well as patients treated for ISR were excluded. Also, left main coronary artery lesions were not included. Patients received DAPT orally for 1 month, followed by aspirin alone.
Endpoints
The primary endpoint was in-lesion MLD gain defined by the difference of MLD post-procedure and at follow-up angiography (see Fig. 1). Secondary endpoints included the mean lumen diameter gains in all segments (see Fig. 2) and the in segment MLD between the post-procedure state and the follow-up angiography.
Follow-up investigations
Consecutive patients with a target coronary angiography follow-up at 4 months were included in our dual centrer QCA analyses. To exclude that changes in the vascular tone were responsible for the vessel size changes, we undertook an internal validation of the angiographic results by performing QCA also in a non-target vessel (see Fig. 1). Non target-reference vessels for validation had to be undiseased vessels or branches and unaffected by the flow in the treated segment. A schematic explanation of the analysed vessel segments is provided in Fig. 2.
Statistical analysis
Sample sizes were estimated with nQuery Advisor version 7.0 (Statistical Solutions Ltd. Cork, Ireland) using the MOT1 algorithm for paired t tests. A sample size of 42 analyzable data sets was estimated that will have 80 % power to detect a difference of 0.20 mm in MLD post-PCI and at follow-up assuming a standard deviation per time point of 0.45 mm based with a 0.05 two-sided significance level.
In parameters with Gaussian distributions, samples were described using the mean and the standard deviation. SPSS version 20.0 (IBM, Munich, Germany) was used for all analyses at a significance level of 0.05.
Quantitative coronary angiography
Angiography of the target vessel was performed in at least two near-orthogonal views showing the target lesion free of foreshortening and vessel overlap. Quantitative analysis of the coronary angiographic images was performed by an investigator at an independent core laboratory. The CAAS II research system (Pie Medical Imaging, Maastricht, the Netherlands) was used for automated contour detection and quantification. The system, data validation and measurement procedures have been adequately published [17, 18]. Analyses were performed from angiograms in identical projections before, after interventions and at the angiographic follow-up. Frames were selected as recommended by Herrington and Walford [19]. Analysis followed the guidelines proposed by Reiber et al. [20]. Lesion length, mean diameter within the lesion (mean stenosis diameter) and MLDs were calculated for the target vessel segment. Also, diameter stenosis and MLD were measured 5 mm from the proximal and distal edge of the treated segment. Restenosis was defined as percentage diameter stenosis >50 % within the treated segment from the control angiography.
To quantify the impact of the DCB treatment on the culprit lesion and the adjacent vessel segment being not severely obstructed, the portion of the treated lesion having a diameter stenosis >50 % was analysed separately from the analysis of the entire vessel segment treated with a DCB.
Thus three segments were evaluated: Segment A represents the lesion, defined as diameter narrowing beyond 50 %; segment B represents the ‘DCB-treated’ segment and segment C included the adjacent 5 mm on both sides of segment B (see Fig. 2).
Reference diameters were defined as average diameters of adjacent undiseased proximal and distal vessel segments. QCA of non-target reference vessel was in the same angiographic scene. All follow-up angiograms were checked for identical projections and segments were identified with the help of anatomical landmarks.
Results
We evaluated 58 native coronary artery lesions (12 RCA, 25 LAD and 21 CX) mainly of small vessels (mean vessel reference diameter 2.58 ± 0.47 mm) in 56 consecutive patients (10 females, 46 males) directly after the DCB intervention and at an angiographic follow-up at 4.1 ± 2.1 months. Epidemiological data and lesion characteristics are given in Table 1. 44 lesions were treated with the SeQuent© Please (B. Braun, Melsungen, Germany) and 14 lesions with the In.Pact Falcon© (Invatec-Medtronic, Italy) DCB catheter. The initial stenosis grade was 69.1 ± 14.0 %.
MLDs increased significantly in all segments (in-lesion and balloon-treated area) except for segment C (in-segment) where the MLD increased only numerically without reaching statistical significance.
The rightward shift of the minimal lesion diameter frequency distribution is shown in Fig. 3. At follow-up the majority of patients showed a mean luminal gain (Figs. 4, 5) and 41 of 58 lesions (69 %) showed a luminal increase while 29 % showed a luminal decrease. In general, luminal increases were much larger than luminal decreases. 5 % of patients had a late lumen loss of more than 0.2 mm. A total of 33 % of patients had a late lumen gain over 0.2 mm. Binary restenosis was found in one of the 58 lesions. There was no statistically significant relationship between stenosis eccentricity and severity, calcification or the time point of the angiographic follow-up (before or after median observation period) and the extent of luminal change. A difference between the two DCB technologies could not be detected due to the small sample sizes.
The mean diameters of the non-target vessels as measured by QCA were the same directly after the PCI and at the angiographic follow-up (see Table 2). Non-target reference vessel diameters were available in 43 out of 58 lesions due angiographic limitations outside of the treated segments. In 15 patients an undiseased non-target reference vessel which would have allowed QCA with enough precision was not apparently available in the angiographic sequences.
Relative to major adverse cardiac events (MACE) there were no patients who presented themselves for angina during the follow-up. In one patient an in-segment binary restenosis (lesion percent diameter narrowing 61 %) was found. However, there was no repeat angioplasty of target vessels in any patient. There was one death after post-procedural day 221 due to multi organ failure. This patient experienced a non ST-segment myocardial infarction at post-interventional day 44 in a non-target vessel and had documented severe chronic heart failure prior to DCB treatment.
Discussion
The most important limitations of POBA so far have been acute vessel recoil with a cross sectional luminal area loss of up to 48 % [21] and restenosis mostly occurring after 2–3 months. Major dissection plays only a limited role in the failure of POBA [4]. In the days when only POBA was available, over 50 % of the patients had luminal re-narrowing between the initial PCI to the follow-up at 180 days. One-fourth of the patients had over 30 % luminal loss [5]. Stents have been developed mainly for this very reason and could demonstrate reduced binary restenosis rates mainly by abandoning vessel recoil. This, however, allowed an even higher grade of renarrowing by exaggerated neointimal proliferation [4, 22, 23] which only the further development of DES could cope with [24–26].
In the early stages of atherosclerosis vessel lumen diameters remain unchanged increasing intimal area being taken up by considerable amounts of plaque material. The luminal narrowing begins only when 40 % of the intimal area consists of plaque [27]. This is produced by vessel growth which might be understood as a compensatory mechanism aiming to maintain flow. This compensation apparently breaks down as soon as the intima becomes more diseased. Indeed, in the hypercholesterolemic rabbit model restenosis was linked not to intimal area but to the external and internal elastic membrane area, i.e. to the vessel size [28]. Moreover, luminal gain was more pronounced than neointimal reduction in a porcine coronary overstretch model with various paclitaxel concentrations. The luminal gain by neointimal reduction was 39 % but the overall lumen increase was 90 % [29].
DCB technology reduces restenosis rate in ISR [8, 9, 30–34], in de novo lesions [32] and in peripheral vessels [35–37]. Our data show a lumen increase during the follow-up period in the majority of the patients (40 of 58). Most likely these lumen increases are due to the effects of paclitaxel on the vascular wall. While an ultimate proof of vessel remodelling as the reason for this luminal increase is not possible on the basis of our data, vascular remodelling is one explanation. Paclitaxel leads to inhibition of smooth muscle cell (SMC) proliferation by modulation of the microtubule formation and upregulation of pro-apoptotic factors [38]. Initially it is found in a much higher concentration in the vascular wall after DCB use than after DES implantation [39, 40] leading not only to cytostasis but also to mitotic and post-mitotic arrest [41]. Thus it is conceivable that more profound effects not only on neointimal growth but also on medial thinning and enlargement are caused by paclitaxel. Pires et al [38] found higher reductions of SMC content in the intima and media after DES implantations while using similar doses of paclitaxel and sirolimus.
Also the secondary malapposition of DES occurring in a considerable number of DES patients as compared to their BMS counterparts [42] could be interpreted as a phenomenon on the same pathophysiological basis. Furthermore, the reported experimental paclitaxel application into the pericardial sac led to marked positive vascular remodelling in a porcine coronary balloon overstretch model [43].
On the basis of this literature our findings may be explained by positive vessel remodelling. Plaque regression or vascular healing could be alternative explanations. In our series, the most pronounced lumen enlargement was seen in segment A representing the area with the highest plaque burden. This finding reveals the possibility that plaque regression can be another mechanism leading to late lumen enlargement. During preparation of this manuscript a late positive vessel remodelling has also been shown after initial late lumen loss in bioabsorbable vascular scaffolds (BVS). BVS lead to the expected late lumen loss in the first 6 months; however, with advancing stent structure absorption a late lumen increase develops from month 6 to 24 [44]. This also helps to explain why despite several randomized trials with the DCB technology a finding like ours has not been described. The stent as a foreign body is a continuous stimulus towards intimal hyperplasia and negative vascular remodelling. Most angiographic follow-up studies with the DCB technology were conducted in ISR patients. In patients with a suboptimal initial angioplasty result, a randomized trial with paclitaxel-urea coated balloons in the superficial femoral artery demonstrated lumen gain at follow-up [35] questioning the paradigm of an optimal (‘stent-like’) primary result after angioplasty.
After first casuistic findings we designed the QCA methodology, finalized the study protocol and entered patients into this study to determine whether our initial observations were rare exceptions. We found that 40 of 58 patients showed luminal improvement which represents a percentage much higher than expected from the relevant POBA literature and our clinical experience. The study was done in two independent centres which came both to the same conclusions. The study populations have been joined since no inter-centre differences in the results were detected. The independence of luminal increase from the time point of the follow-up angiography makes a late-catch up phenomenon with later re-narrowing unlikely.
Moreover, the mechanisms of luminal improvement remain unproven. While the literature and paclitaxel’s mechanism of action points to positive vessel remodelling, plaque regression or other healing mechanisms cannot be excluded without studies with optical coherence tomography (OCT) or intravascular ultrasound (IVUS). We did not find any predictive lesion characteristics promoting luminal increase like in earlier POBA populations [45]. However, this might be due to our relatively small patient population. We strongly feel that our findings warrant further clinical investigations. Furthermore, the effect on vascular healing after the vessel injury due to balloon angioplasty is most likely but not certainly to be attributed to paclitaxel. The introduction of DAPT, albeit only for 4 weeks, could influence platelet apposition and thus restenosis via lower production of platelet derived growth factors (PDGF) [46, 47]. This relationship has been challenged and restenosis after POBA occurs primarily after 2–3 months, a time when platelet deposition should not play a major role [48]. Also, the improved efficacy of DCB vs. POBA in ISR and in de novo lesions [9, 12, 33, 49] does not make it likely that the observed effect is due to DAPT which was equally applied to POBA and DCB patient groups.
Finally, one might argue that subtle changes in luminal diameters would not be clinically relevant. However, even with unchanged plaque load, an increase in vessel diameter of only 10 % leads to a luminal gain of up to 100 %. This, however, depends on the degree of stenosis and the vessel diameter change which have been proposed as the major mechanism of restenosis after PTCA [28, 50].
Study limitations
This was not a randomized study. However, a randomization against stenting would have been inappropriate since the mechanisms leading to luminal changes after stenting are different (intimal hyperplasia). On the other hand, randomization against POBA was felt to be unethical because of the expected high restenosis rates. Thus, for this mechanistic study we believed a non-randomized study was a first appropriate approach.
Furthermore, the inclusion of patients without major dissections and recoil might influence the results. This is probably true to a certain extent. However, the small vessel size, the lesion length and the lesion characteristics (eccentricity in 34 lesions) in the studied population do not favour a low restenosis rate. Measurement of translesion pressure drop has been proposed by Andreas Gruentzig [51]. These trans-lesion pressure measurement may serve as a predictor of restenosis. The use of the fractional flow reserve (FFR) methodology at the end of the procedure might be worthwhile to study in this context.
Finally, additional studies using more precise imaging modalities like OCT might help to verify and better understand our findings [52].
Conclusion
In conclusion, our findings of luminal vessel diameter increase suggest a new era of stent-free vascular therapy especially for small vessels. By local drug release to the vascular wall, positive effects to reduce neointimal hyperplasia and even to increase vascular lumen are possible. DCB angioplasty might be able to mimic compensatory mechanisms in early atherosclerosis, thereby overcoming one of the major limitations of percuteaneous transluminal angioplasty (coronary, peripheral).
References
Smith SC Jr, Feldman TE, Hirshfeld JW Jr et al (2006) American College of Cardiology/American Heart Association Task Force on Practice Guidelines; ACC/AHA/SCAI Writing Committee to Update the 2001 Guidelines for Percutaneous Coronary Intervention. ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update the 2001 Guidelines for Percutaneous Coronary Intervention). J Am Coll Cardiol 47:e1–e121
Wijns W, Kolh P, Danchin N et al (2010) Guidelines on myocardial revascularization. Eur Heart J 31:2501–2555
Brophy JM, Belisle P, Joseph L (2003) Evidence for use of coronary stents. A hierarchical bayesian meta-analysis. Ann Intern Med 138:777–786
Al Suwaidi J, Holmes DR Jr, Salam AM et al (2004) Impact of coronary artery stents on mortality and nonfatal myocardial infarction: meta-analysis of randomized trials comparing a strategy of routine stenting with that of balloon angioplasty. Am Heart J 147:815–822
Holmes DR Jr, Vlietstra RE, Smith HC et al (1984) Restenosis after percutaneous transluminal coronary angioplasty (PTCA): a report from the PTCA Registry of the National Heart, Lung, and Blood Institute. Am J Cardiol 53:77C–81C
Cremers B, Toner JL, Schwartz LB et al (2012) Inhibition of neointimal hyperplasia with a novel zotarolimus coated balloon catheter. Clin Res Cardiol 101(6):469–476
Cremers B, Kelsch B, Clever YP et al (2012) Inhibition of neointimal proliferation after bare metal stent implantation with low-pressure drug delivery using a paclitaxel-coated balloon in porcine coronary arteries. Clin Res Cardiol 101(5):385–391
Scheller B, Hehrlein C, Bocksch W et al (2006) Treatment of coronary in-stent restenosis with a paclitaxel-coated balloon catheter. N Engl J Med 355:2113–2124
Unverdorben M, Vallbracht C, Cremers B et al (2009) Paclitaxel-coated balloon catheter versus paclitaxel-coated stent for the treatment of coronary in-stent restenosis. Circulation 119:2986–2994
Navarese EP, Austin D, Gurbel PA et al (2013) Drug-coated balloons in treatment of in-stent restenosis: a meta-analysis of randomised controlled trials. Clin Res Cardiol 102(4):279–287
Bonaventura K, Leber AW, Sohns C et al (2012) Cost-effectiveness of paclitaxel-coated balloon angioplasty and paclitaxel-eluting stent implantation for treatment of coronary in-stent restenosis in patients with stable coronary artery disease. Clin Res Cardiol 101(7):573–584
Wöhrle J, Zadura M, Möbius-Winkler S et al (2012) SeQuentPlease World Wide Registry: clinical results of SeQuent please paclitaxel-coated balloon angioplasty in a large-scale, prospective registry study. J Am Coll Cardiol 60:1733–1738
Scheller B, Fischer D, Clever YP et al (2013) Treatment of a coronary bifurcation lesion with drug-coated balloons: lumen enlargement and plaque modification after 6 months. Clin Res Cardiol 102(6):469–472
Kleber FX, Mathey DG, Rittger H et al (2011) How to use the drug-eluting balloon: recommendations by the German consensus group. EuroIntervention 7(Suppl K):K125–K128
Kleber FX, Rittger H, Bonaventura K et al (2013) Drug-coated balloons for treatment of coronary artery disease: updated recommendations from a consensus group. Clin Res Cardiol 102(11):785–797
Huber MS, Mooney JF, Madison J et al (1991) Use of a morphologic classification to predict clinical outcome after dissection from coronary angioplasty. Am J Cardiol 68:467–471
Hausleiter J, Jost S, Nolte CW et al (1997) Comparative in vitro validation of eight first- and second-generation quantitative coronary angiography systems. Coron Artery Dis 8:83–90
Dietz U, Rupprecht HJ, Brennecke R et al (1997) Comparison of QCA systems. Int J Card Imaging 13:271–280
Herrington D, Walford G (1993) Optimal frame selection for QCA. In: Reiber JHC, Serruys PW (eds) Advances in quantitative coronary arteriography. Kluwer Academic Publishers, Dordrecht, pp 125–135
Reiber JH, van Eldik-Helleman P, Visser-Akkerman N et al (1988) Variabilities in measurement of coronary arterial dimensions resulting from variations in cineframe selection. Cathet Cardiovasc Diagn 14:221–228
Haude M, Erbel R, Issa H et al (1993) Quantitative analysis of elastic recoil after balloon angioplasty and after intracoronary implantation of balloon-expandable Palmaz-Schatz stents. J Am Coll Cardiol 21:26–34
Sigwart U, Puel J, Mirkovitch V et al (1987) Intravascular stents to prevent occlusion and restenosis after transluminal angioplasty. N Engl J Med 316:701–706
Serruys PW, de Jaegere P, Kiemeneij F et al (1994) A comparison of balloon-expandable-stent implantation with balloon angioplasty in patients with coronary artery disease. Benestent Study Group. N Engl J Med 331:489–495
Brener SJ, Prasad AJ, Khan Z et al (2011) The relationship between late lumen loss and restenosis among various drug-eluting stents: a systematic review and meta-regression analysis of randomized clinical trials. Atherosclerosis 214:158–162
Chevalier B, Silber S, Park SJ, NOBORI 1 Clinical Investigators et al (2009) Randomized comparison of the Nobori Biolimus A9-eluting coronary stent with the Taxus Liberte paclitaxel-eluting coronary stent in patients with stenosis in native coronary arteries: the NOBORI 1 trial–Phase 2. Circ Cardiovasc Interv 2:188–195
Bondesson P, Lagerqvist B, James SK et al (2012) Comparison of two drug-eluting balloons: a report from the SCAAR registry. EuroIntervention 8:444–449
Glagov S, Weisenberg E, Zarins CK et al (1987) Compensatory enlargement of human atherosclerotic coronary arteries. N Engl J Med 316:1371–1375
Kakuta T, Currier JW, Haudenschild CC et al (1994) Differences in compensatory vessel enlargement, not intimal formation, account for restenosis after angioplasty in the hypercholesterolemic rabbit model. Circulation 89:2809–2815
Heldman AW, Cheng L, Jenkins GM et al (2001) Paclitaxel stent coating inhibits neointimal hyperplasia at 4 weeks in a porcine model of coronary restenosis. Circulation 103:2289–2295
Habara S, Mitsudo K, Kadota K et al (2011) Effectiveness of paclitaxel-eluting balloon catheter in patients with sirolimus-eluting stent restenosis. JACC Cardiovasc Interv 4:149–154
Byrne RA, Neumann FJ, Mehilli J, ISAR-DESIRE 3 investigators et al (2013) Paclitaxel-eluting balloons, paclitaxel-eluting stents, and balloon angioplasty in patients with restenosis after implantation of a drug-eluting stent (ISAR-DESIRE 3): a randomised, open-label trial. Lancet 381:461–467
Latib A, Colombo A, Castriota F et al (2012) A randomized multicenter study comparing a paclitaxel drug-eluting balloon with a paclitaxel-eluting stent in small coronary vessels: the BELLO (Balloon Elution and Late Loss Optimization) study. J Am Coll Cardiol 60:2473–2480
Rittger H, Brachmann J, Sinha AM et al (2012) A randomized, multicenter, single-blinded trial comparing paclitaxel-coated balloon angioplasty with plain balloon angioplasty in drug-eluting stent restenosis: the PEPCAD-DES study. J Am Coll Cardiol 59:1377–1382
Clever YP, Cremers B, von Scheidt W et al (2014) Compassionate use of a paclitaxel coated balloon in patients with refractory recurrent coronary in-stent restenosis. Clin Res Cardiol 103(1):21–27
Werk M, Albrecht T, Meyer DR et al (2012) Paclitaxel-coated balloons reduce Restenosis after femoro-popliteal angioplasty: evidence from the randomized PACIFIER trial. Circ Cardiovasc Interv 5:831–840
Tepe G, Zeller T, Albrecht T et al (2008) Local delivery of paclitaxel to inhibit restenosis during angioplasty of the leg. N Engl J Med 358:689–699
Werk M, Langner S, Reinkensmeier B et al (2008) Inhibition of restenosis in femoropopliteal arteries: paclitaxel-coated versus uncoated balloon: femoral paclitaxel randomized pilot trial. Circulation 118:1358–1365
Pires NM, Eefting D, de Vries MR et al (2007) Sirolimus and paclitaxel provoke different vascular pathological responses after local delivery in a murine model for restenosis on underlying atherosclerotic arteries. Heart 93:922–927
Vogt F, Stein A, Rettemeier G et al (2004) Long-term assessment of a novel biodegradable paclitaxel-eluting coronary polylactide stent. Eur Heart J 25:1330–1340
Speck U, Cremers B, Kelsch B et al (2012) Do pharmacokinetics explain persistent restenosis inhibition by a single dose of paclitaxel? Circ Cardiovasc Interv 5:392–400
Axel DI, Kunert W, Göggelmann C et al (1997) Paclitaxel inhibits arterial smooth muscle cell proliferation and migration in vitro and in vivo using local drug delivery. Circulation 96:636–645
Ako J, Morino Y, Honda Y et al (2005) Late incomplete stent apposition after sirolimus-eluting stent implantation: a serial intravascular ultrasound analysis. J Am Coll Cardiol 46:1002–1005
Hou D, Rogers PI, Toleikis PM et al (2000) Intrapericardial paclitaxel delivery inhibits neointimal proliferation and promotes arterial enlargement after porcine coronary overstretch. Circulation 102:1575–1581
Diletti R, Serruys PW, Farooq V et al (2012) ABSORB II randomized controlled trial: a clinical evaluation to compare the safety, efficacy, and performance of the Absorb everolimus-eluting bioresorbable vascular scaffold system against the XIENCE everolimus-eluting coronary stent system in the treatment of subjects with ischemic heart disease caused by de novo native coronary artery lesions: rationale and study design. Am Heart J 164:654–663
Hirshfeld JW Jr, Schwartz JS, Jugo R et al (1991) Clinical and angiographic determinants of primary coronary angioplasty success. M-HEART Investigators. J Am Coll Cardiol 17:22–28
Lam JY, Chesebro JH, Steele PM et al (1986) Deep arterial injury during experimental angioplasty: relation to a positive indium-111-labeled platelet scintigram, quantitative platelet deposition and mural thrombosis. J Am Coll Cardiol 8:1380–1386
Chesebro JH, Lam JY, Badimon L et al (1987) Restenosis after arterial angioplasty: a hemorrheologic response to injury. Am J Cardiol 60:10B–16B
Serruys PW, Luijten HE, Beatt KJ et al (1988) Incidence of restenosis after successful coronary angioplasty: a time-related phenomenon. A quantitative angiographic study in 342 consecutive patients at 1, 2, 3, and 4 months. Circulation 77:361–371
Zeymer U, Waliszewski M, Spiecker M et al (2014) Prospective ‘real world’ registry for the use of the ‘PCB only’ strategy in small vessel de novo lesions. Heart 100(4):311–316
Currier JW, Faxon DP (1995) Restenosis after percutaneous transluminal coronary angioplasty: have we been aiming at the wrong target? J Am Coll Cardiol 25:516–520
Leimgruber PP, Roubin GS, Anderson HV et al (1985) Influence of intimal dissection on restenosis after successful coronary angioplasty. Circulation 72:530–535
Poerner TC, Otto S, Gassdorf J et al (2011) A prospective randomised study using optical coherence tomography to assess endothelial coverage and neointimal proliferation at 6-months after implantation of a coronary everolimus-eluting stent compared with a bare metal stent postdilated with a paclitaxel-eluting balloon (OCTOPUS Trial): rationale, design and methods. EuroIntervention 7(Suppl K):K93–K99
Conflict of interest
The authors declare the following conflicts of interest: Franz Kleber is a consultant to B. Braun and has received institutional grant support by Medtronic and B. Braun. Yvonne Clever and Telse Hausschild declared no potential conflict of interest. Antonia Schulz received travel expenses from B. Braun. Matthias Waliszweski is a full-time employee at the Medical Scientific Affairs department of B. Braun Vascular Systems. Michael Böhm and Ulrich Dietz declared no conflict of interest. Bruno Scheller is a consultant to B. Braun and received institutional grants and lecture fees from B. Braun as well as travel expenses from Medtronic and B. Braun. Bodo Cremers received lecture fees from Medtronic and B. Braun as well as travel expenses from Medtronic and B. Braun. This is an investigator-driven study. Relative to this clinical assessment there was no funding provided from any public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kleber, F.X., Schulz, A., Waliszewski, M. et al. Local paclitaxel induces late lumen enlargement in coronary arteries after balloon angioplasty. Clin Res Cardiol 104, 217–225 (2015). https://doi.org/10.1007/s00392-014-0775-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-014-0775-2