Abstract
Objective
Conflicting data exists regarding the frequency and significance of acute kidney injury (AKI) in ST segment elevation MI (STEMI) patients. The acute kidney injury network (AKIN) classification has been shown to predict mortality in various critically ill patients; however, limited information is available regarding its use and its clinical relevance among STEMI patients.
Study design and methods
We retrospectively studied 1,033 STEMI patients undergoing primary percutaneous intervention (PCI). AKI was identified on the basis of the changes in serum creatinine during hospitalization according to the AKIN criteria. Patients were assessed for in-hospital adverse outcomes as well as all-cause mortality up to 5 years.
Results
Overall, 100 patients (9.6 %) developed AKI: 79 patients (79 %) had stage 1, 14 patients (14 %) developed stage 2, and 7 patients (7 %) developed stage 3 AKI. Patients with AKI had more complications during hospitalization, with higher 30 days (11 vs 1 %; p < 0.001) and 5-year all-cause mortality (29 vs 6 %; p < 0.001) compared to those without AKI. The adjusted risk of death increased proportionally to AKI severity. Compared to patients with no AKI, the adjusted hazard ratio for all-cause mortality was 6.68 (95 % confidence interval: 2.1–21.6, p = 0.002) in patients with AKI. Age, hypertension, chronic kidney injury and low left ventricular ejection fraction were independent predictors of developing AKI.
Conclusion
In STEMI patients undergoing primary PCI, AKI assessed by AKIN criteria is a frequent complication, associated with an increased risk of both short- and long-term mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Previous reports have shown that among ST elevation acute myocardial infarction (STEMI) patients, the development of acute kidney injury (AKI) occurs during hospitalization in 10–27 % of acute MI patients and predicts both short- and long-term mortality [1–5]. Since no standardized definition of AKI has been used previously for patients with MI, information on the true incidence as well as the clinical and prognostic are still lacking. The recently proposed AKI network (AKIN) [6] provides a standardized definition of AKI, and includes three stages based on the changes in serum creatinine. Although the use of this classification was shown to predict mortality in a variety of critically ill patients including septic, post cardiac surgery and following angiography [7–10], limited information is available regarding the use of the AKIN classification to evaluate the incidence and clinical relevance of AKI among STEMI patients, especially in those undergoing primary percutaneous intervention (PCI), as well as its relation to long-term survival. In the present study, we evaluated the incidence, risk factors, in-hospital complications as well as the short- and long-term mortality associated with AKI as classified by AKIN definition in a large single-center cohort of consecutive STEMI patients.
Methods
Study population
A retrospective, single-center observational study was conducted in the Tel-Aviv Sourasky Medical Center, a tertiary referral hospital with a 24/7 primary PCI service. Included were all 1,105 consecutive patients admitted between January 2008 and November 2012 to the cardiac intensive care unit (CICU) with the diagnosis of acute STEMI. Excluded were 18 patients who were treated either conservatively or with thrombolysis, and 45 patients whose final diagnosis on discharge was other than anterior wall STEMI (e.g. myocarditis or Takotusubo cardiomyopathy). Also excluded were patients who died within 24 h of admission (n = 6) because they would not have had sufficient time to develop AKI and patients requiring chronic peritoneal or hemodialysis (n = 3) treatment. The final study population included 1,033 patients (Fig. 1) whose baseline demographic, cardiovascular history, clinical risk factors, treatment characteristics and laboratory results were retrieved from their medical files.
Protocol
The diagnosis of STEMI was established by a typical history of chest pain, diagnostic electrocardiographic changes, and serial elevation of serum cardiac biomarkers [11].
Primary PCI was performed in patients with symptoms ≤12 h in duration as well as in patients with symptoms lasting 12–24 h in duration if the symptoms continued to persist at the time of admission. Following primary PCI, left ventricular ejection fraction was measured in all patients, by bedside echocardiography, within the first 48 h of admission. Patient records were evaluated for in-hospital mortality and complications occurring during the hospitalization. These included cardiogenic shock or the need for intra aortic balloon counterpulsation (IABC) treatment, need for emergent coronary artery bypass graft (CABG) surgery, mechanical ventilation or heart failure episodes treated conservatively, clinically significant tachyarrhythmias (ventricular fibrillation, sustained ventricular tachycardia, and atrial fibrillation) and bradyarrhythmias requiring pacemaker as well as major bleeding (requiring blood transfusion). Mortality was assessed over a median period of 1,526 ± 298 days (range 2–2,130) up to August 1, 2013. Assessment of survival following hospital discharge was determined from computerized records of the population registry bureau. The study protocol was approved by the local institutional ethics committee.
Laboratory
The serum creatinine (sCr) was determined upon hospital admission and at least once a day during the CICU stay and was available for all analyzed patients. The estimated glomerular filtration rate was estimated using the abbreviated modification of diet in renal disease equation (MDRD) [12]. Baseline renal insufficiency was categorized as an estimated glomerular filtration rate (eGFR) of ≤60 ml/min/1.73 m2 [13]. AKI was defined, applying the AKIN classification [6], according to the maximum increase in sCr from baseline (hospital admission): stage 1—an increase of ≥0.3 mg/dl in sCr; stage 2—more than two- to threefold sCr increase; stage 3—more than threefold sCr increase from baseline or baseline sCr >4.0 mg/dl with an acute increase of >0.5 mg/dl; or the need for renal replacement therapy, irrespective of the AKIN stage at renal replacement therapy initiation. Renal recovery was defined as a reduction in sCr to the admission range without the need for renal replacement therapy.
Statistical analysis
All data were summarized and displayed as mean (±standard deviation) or median (25–75 %) for continuous variables and as number (percentage) of patients in each group for categorical variables. The p values for the Chi-square test were calculated with the Fisher’s exact test. Continuous variables were compared using the independent sample t test or Mann–Whitney test. The identification of the independent predictors of AKI was assessed using logistic regression. Binary logistic regression models were performed using the Enter mode. The models were adjusted for age, male gender, left ventricular ejection fraction, hypertension, diabetes mellitus, eGFR and symptom duration. The influence of AKIN on the occurrence of all-cause mortality was evaluated using multivariate Cox regression. We adjusted for age, gender, hypertension, diabetes mellitus, smoking status, left ventricular ejection fraction, eGFR, peak creatine phosphkinase (CPK),baseline hemoglobin, white blood cell count, high sensitive C reactive protein (CRP) levels, and AKIN status. A two-tailed p value <0.05 was considered significant for all analyses. All analyses were performed with the SPSS 20.0 software (SPSS Inc., Chicago, IL).
Results
A total of 1,033 STEMI patients treated by primary PCI were enrolled in the study, 100 (9.6 %) of whom developed AKI in accordance with the AKIN criteria. Stage 1 AKI occurred in 79 patients (79 %, mean sCr increase 0.46 ± 0.21 mg/dl), AKI stage 2 occurred in 14 patients (14 %, mean sCr increase 1.3 ± 0.29 mg/dl) and AKI stage 3 developed in 7 patients (7 %, mean sCr increase 2.26 ± 1.45 mg/dl). Only 2 patients among those developing AKI required renal replacement therapy throughout hospitalization, whereas 57 (57 %) of the AKI patients had renal recovery at CICU discharge. A total of 257 patients (25 %) had baseline renal insufficiency upon hospital admission.
The baseline clinical characteristics of patients with and without AKIN are listed in Table 1. Patients with AKI were more likely to be older, of female gender, to have more co-morbidities, longer symptom duration prior to emergency room admission, lower baseline eGFR, lower left ventricular ejection fraction and longer time until hospital discharge.
The occurrence of AKI following STEMI treated with primary PCI resulted in more complications and adverse events during hospitalization, as well as higher 30-day mortality (Table 2).
Long-term outcome
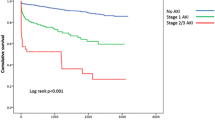
Over a mean period of 2.7 + 1.6 years, 72 (6.9 %) patients of the entire cohort died. Mortality was significantly higher among those with AKI (29/100, 29 %) following STEMI than those without AKI (43/933, 4.6 %); p < 0.001). Among the 29 patients with AKI who died, 20 (69 %) had AKIN stage 1 and 9 patients (31 %) had AKIN stages 2 and 3. Figure 2 shows the Kaplan–Meier survival curve for long-term survival according to the AKIN stages. A significant increase in long-term mortality was observed between patients without AKI and those with stage 1 and 2/3 AKIN (p < 0.001). AKI was an independent predictor of mortality reaching a hazard ratio of 6.68 (95 % CI 2.1–21.6, p = 0.002) compared to patients without AKI. Within the AKIN groups the hazard ratio for all-cause mortality was 7.42 (95 % CI 1.9–27.8, p = 0.003) for stage 1 AKIN, and 5.55 (95 % CI 1.1–28.8, p = 0.04) for combined AKIN stages 2 and 3.
Predictors of AKI
We created a multivariate regression model in order to elucidate the risk factors predicting the development of AKI. The major risk factors found for AKI occurrence were hypertension (OR 2.6, 95 % CI 1.5–4.3, p < 0.001), gradual 1 % reductions in left ventricular ejection fraction (OR 0.95, 95 % CI 0.92–0.97, p < 0.001) and eGFR (OR 0.972, 95 % CI 0.95–0.99, p = 0.005) and a trend for every 1 year of age increment (OR 1.025, 95 % CI 0.96–1.05, p = 0.09) (Table 3).
Discussion
The main finding in our study is that early AKI is a frequent complication, occurring among 9.6 % of STEMI patients undergoing primary PCI, and that even mild elevation of sCr (≥0.3 mg/dl, AKIN stage 1) is associated with a marked increase in both in-hospital and all-cause mortality, up to 5 years following STEMI. To our knowledge, this is the first study assessing both short- and long-term mortality in a large non-selected population of patients presenting with STEMI and treated by primary PCI, in whom the AKIN classification was assessed following daily measurement of sCr.
The worsening of renal function throughout hospitalization in STEMI patients is multifactorial and is affected by hemodynamic state, contrast material use during cardiac catheterization, drugs admitted (especially blockers of the renin angiotensin axis) as well as the occurrence of sepsis, bleeding, atheroembolic disease and acute hyperglycemia [14–16].
The lack of consensus criteria to define AKI occurrence and severity had resulted in marked variability of reported AKI among AMI patients ranging from 10 to 27 %, depending on the study population considered, the period during which the study was conducted and, in particular, the criteria used to define AKI [1–5]. Several definitions of AKI have been used in AMI studies. Some studies defined AKI as an absolute (≥0.3 or ≥0.5 mg/dl) or relative (>25 %) increases in sCr above baseline at any point during hospital stay, without stratification of AKI severity. Other studies proposed a staged classification of AKI based on the both absolute and relative sCr changes [17, 18]. Moreover, sCr was evaluated at different time frames, ranging from 24 h following AMI to 1 week [1, 3, 10, 14, 15]. The different definitions of AKI and heterogeneous data reported have lead to difficulties in comparing the various study results. In order to amend the lack of a standardized definition, the Acute Dialysis Quality Initiative Group (ADQI) proposed in 2002 the classification Risk, Injury, Failure, Loss and End-stage Renal Failure (RIFLE) classification [19, 20]. The AKIN proposed in 2005 improvements to the RIFLE criteria in order to make the detection of AKI swift and clear, by adopting a lower cutoff point for variation in serum creatinine [6]. Although the importance and prognostic implications of the AKIN classification were validated in various critical care conditions [7–9, 21–23], limited data exists regarding the utilization of AKIN in ischemic patients.
Hwang et al. [24] reported a 30 % prevalence of AKI, defined by AKIN among AMI patients which independently predicted 1-year mortality, with stage 3 AKIN STEMI patients having the worst outcomes. No information was reported on the distribution of AKIN between STEMI and non-STEMI patients, and regarding the use of PCI. Marenzi et al. [25] evaluated the incidence and outcomes associated with AKI, defined by AKIN, in a large group of acute coronary syndrome patients. In that report AKI prevalence was 13 % (14 % among STEMI patients) and associated with a more complicated in-hospital course and higher in-hospital mortality. AKI was more prevalent among STEMI patients, and those undergoing primary PCI; however the latter was performed in only 82 % of STEMI patients. Our study is novel in several aspects, since it is the first to evaluate AKI and long-term all-cause mortality in a large homogeneous cohort of STEMI patients, all undergoing primary PCI. The lower incidence of AKI in our cohort (9.6 % compared to 14 % in the STEMI group described by Marenzi [25]), although a higher rate of primary PCI in our cohort, may theoretically point out that early PCI in STEMI patients may protect against AKI development, as it allows early normalization of cardiovascular hemodynamics. Although our findings demonstrated a lower hazard ratio for long-term mortality among AKIN stages 2 and 3 patients as compared to those with AKIN stage 1, we believe that these results reflect the lower number of patients having AKIN 2/3 (21/1,033, 2 %), and that eventually a higher AKIN stage will be associated with a higher risk for mortality.
Our findings bare some important clinical implications. The close association between even a small elevation (≥0.3 mg/dl) in sCr and increased morbidity and mortality observed in our study highlights the importance of obtaining a baseline sCr value early after admission for STEMI, and the need for frequent monitoring of renal function during the entire hospitalization period. The identification of AKI predictors, such as hypertension, age, baseline eGFR, and left ventricular ejection fraction may help in pointing those at higher risk, warranting even more frequent monitoring and prompt intervention. In those patients the early implementation of prophylactic strategies aimed at preventing AKI or at reducing its severity might also provide significant clinical benefit. Recent trials demonstrated that among patients with chronic renal disease a single high loading dose of atorvastatin administered within 24 h before contrast material exposure is effective in reducing the rate of contrast-induced AKI [26, 27]. In addition, rapid alkalization by bolus injection of sodium bicarbonate was effective for the prevention of contrast-induced nephropathy (CIN) in patients with chronic kidney disease undergoing emergent procedures [28].
Another novel treatment strategy recently shown to decrease contrast-induced AKI is remote ischemic preconditioning (rIPC), defined as transient brief episodes of ischemia at a remote site, and represents an adaptive response that protects against ischemic and reperfusion insult in various organs [29, 30]. Studies demonstrated that rIPC has protective effects on renal function among patients undergoing elective PCI [31, 32] and was shown to increase myocardial salvage among STEMI patients undergoing primary PCI [33]. In this regard, rIPC may offer a novel noninvasive and virtually cost-free treatment strategy for improving cardiovascular hemodynamics and decreasing AKI incidence in this population.
Finally, as AKI was associated with higher long-term mortality, it should be regularly reported as part of the in-hospital course, even if mild and transient.
The major limitation of our study was lack of information regarding the volume of contrast material used during primary PCI, which was available only for a minority of patients. Thus, the effect of contrast volume on renal impairment was not included in the analysis. Contrast-induced acute kidney injury (CI-AKI) is a prevalent and deleterious complication of coronary angiography and reported to be the third most common cause of hospital-acquired renal failure [34]. The risk of CI-AKI is directly associated with increasing contrast media volume [35], with incidence ranging from 2 % among patients with normal baseline renal function to as high as 20–30 % in patients with a baseline creatinine >2.0 mg/dl [36]. Even after adjusting for baseline renal function and co-morbidities, in-hospital mortality is about fivefold higher in CI-AKI patients, and 1- and 5-year mortality rates are about fourfold higher [37]. We believe, however, that additional factors aside from CI-AKI contribute to AKI development in this setting [14–16]. Our above-mentioned results show that patients developing AKI had longer symptom duration and worse LV function, which can alter hemodynamics and renal perfusion. Symptom duration in AMI is a powerful prognostic marker in AMI patients undergoing reperfusion [38, 39] and major consideration is given to minimizing ischemic duration in order to improve survival following an AMI [40]. Time to reperfusion is known to determine infarct size [41, 42] and systolic function [42, 43], which was also true in our cohort. In addition, we recently demonstrated that longer symptom duration is associated with higher admission C reactive protein and lower hemoglobin level in STEMI patients [44]. It appears thus that longer symptom duration may alter left ventricular function and hemodynamics as a consequence of inflammation, thus contributing to AKI development.
Our study bares some other notable limitations. First, this was a single-center retrospective, non-randomized observational study, and as such may have been subject to bias, even though we included consecutive patients and attempted to adjust for confounding factors using the multivariate Cox regression model. Second, although AKI definition refers to a sCr increase compared to the baseline value, the sCr at hospital admission may not represent a true baseline value in STEMI patients as an increase could have already occurred prior to hospital arrival owing to the hemodynamic impairment. Third, data regarding concomitant therapy with statins, Renin/angiotensin blockers and diuretics throughout hospitalization were not present for many patients, and their effect on AKI development could not be assessed. Finally, the definition of AKIN refers to sCr change within a time frame of 48 h. As the change in sCr can lag beyond this time period due to delayed effects of contrast material and drugs, worsening of renal function might have occurred following hospital discharge in some patients, thus the true incidence of AKI described in our study may have been an underestimation.
We conclude that AKI defined by AKIN is a frequent and hazardous complication in STEMI patients in the primary PCI era, and its occurrence is associated with adverse short- and long-term outcomes.
References
Goldberg A, Hammerman H, Petcherski S, Zdorovyak A, Yalonetsky S, Kapeliovich M, Agmon Y, Markiewicz W, Aronson D (2005) Inhospital and 1-year mortality of patients who develop worsening renal function following acute ST-elevation myocardial infarction. Am Heart J 150(2):330–337. doi:10.1016/j.ahj.2004.09.055
Parikh CR, Coca SG, Wang Y, Masoudi FA, Krumholz HM (2008) Long-term prognosis of acute kidney injury after acute myocardial infarction. Arch Intern Med 168(9):987–995. doi:10.1001/archinte.168.9.987
Marenzi G, Assanelli E, Campodonico J, De Metrio M, Lauri G, Marana I, Moltrasio M, Rubino M, Veglia F, Montorsi P, Bartorelli AL (2010) Acute kidney injury in ST-segment elevation acute myocardial infarction complicated by cardiogenic shock at admission. Crit Care Med 38(2):438–444. doi:10.1097/CCM.0b013e3181b9eb3b
Amin AP, Spertus JA, Reid KJ, Lan X, Buchanan DM, Decker C, Masoudi FA (2010) The prognostic importance of worsening renal function during an acute myocardial infarction on long-term mortality. Am Heart J 160(6):1065–1071. doi:10.1016/j.ahj.2010.08.007
Latchamsetty R, Fang J, Kline-Rogers E, Mukherjee D, Otten RF, LaBounty TM, Emery MS, Eagle KA, Froehlich JB (2007) Prognostic value of transient and sustained increase in in-hospital creatinine on outcomes of patients admitted with acute coronary syndrome. Am J Cardiol 99(7):939–942. doi:10.1016/j.amjcard.2006.10.058
Levin A, Warnock DG, Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C (2007) Improving outcomes from acute kidney injury: report of an initiative. Am J Kidney Dis 50(1):1–4. doi:10.1053/j.ajkd.2007.05.008
Bagshaw SM, George C, Dinu I, Bellomo R (2008) A multi-centre evaluation of the RIFLE criteria for early acute kidney injury in critically ill patients. Nephrol Dial Transplant 23(4):1203–1210. doi:10.1093/ndt/gfm744
Bagshaw SM, George C, Bellomo R (2008) Early acute kidney injury and sepsis: a multicentre evaluation. Crit Care 12(2):R47. doi:10.1186/cc6863
Hobson CE, Yavas S, Segal MS, Schold JD, Tribble CG, Layon AJ, Bihorac A (2009) Acute kidney injury is associated with increased long-term mortality after cardiothoracic surgery. Circulation 119(18):2444–2453. doi:10.1161/CIRCULATIONAHA.108.800011
James MT, Ghali WA, Knudtson ML, Ravani P, Tonelli M, Faris P, Pannu N, Manns BJ, Klarenbach SW, Hemmelgarn BR (2011) Associations between acute kidney injury and cardiovascular and renal outcomes after coronary angiography. Circulation 123(4):409–416. doi:10.1161/CIRCULATIONAHA.110.970160
O’Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX, Anderson JL, Jacobs AK, Halperin JL, Albert NM, Brindis RG, Creager MA, DeMets D, Guyton RA, Hochman JS, Kovacs RJ, Ohman EM, Stevenson WG, Yancy CW (2012) 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 61(4):e78–e140. doi:10.1016/j.jacc.2012.11.019
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 130(6):461–470
Board. NKFNKDOQIKDA (2002) K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 39(2 Suppl 1):S1–S266
Koreny M, Karth GD, Geppert A, Neunteufl T, Priglinger U, Heinz G, Siostrzonek P (2002) Prognosis of patients who develop acute renal failure during the first 24 hours of cardiogenic shock after myocardial infarction. Am J Med 112(2):115–119
Marenzi G, Assanelli E, Campodonico J, Lauri G, Marana I, De Metrio M, Moltrasio M, Grazi M, Rubino M, Veglia F, Fabbiocchi F, Bartorelli AL (2009) Contrast volume during primary percutaneous coronary intervention and subsequent contrast-induced nephropathy and mortality. Ann Intern Med 150(3):170–177
Marenzi G, De Metrio M, Rubino M, Lauri G, Cavallero A, Assanelli E, Grazi M, Moltrasio M, Marana I, Campodonico J, Discacciati A, Veglia F, Bartorelli AL (2010) Acute hyperglycemia and contrast-induced nephropathy in primary percutaneous coronary intervention. Am Heart J 160(6):1170–1177. doi:10.1016/j.ahj.2010.09.022
Weisbord SD, Chen H, Stone RA, Kip KE, Fine MJ, Saul MI, Palevsky PM (2006) Associations of increases in serum creatinine with mortality and length of hospital stay after coronary angiography. J Am Soc Nephrol 17(10):2871–2877. doi:10.1681/ASN.2006030301
Fox CS, Muntner P, Chen AY, Alexander KP, Roe MT, Wiviott SD (2012) Short-term outcomes of acute myocardial infarction in patients with acute kidney injury: a report from the national cardiovascular data registry. Circulation 125(3):497–504. doi:10.1161/CIRCULATIONAHA.111.039909
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P (2004) Acute renal failure—definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care 8(4):R204–R212. doi:10.1186/cc2872
Srisawat N, Hoste EE, Kellum JA (2010) Modern classification of acute kidney injury. Blood Purif 29(3):300–307. doi:10.1159/000280099
Palmieri T, Lavrentieva A, Greenhalgh DG (2010) Acute kidney injury in critically ill burn patients. Risk factors, progression and impact on mortality. Burns 36(2):205–211. doi:10.1016/j.burns.2009.08.012
Moore EM, Bellomo R, Nichol A, Harley N, Macisaac C, Cooper DJ (2010) The incidence of acute kidney injury in patients with traumatic brain injury. Ren Fail 32(9):1060–1065. doi:10.3109/0886022X.2010.510234
Kundakci A, Pirat A, Komurcu O, Torgay A, Karakayali H, Arslan G, Haberal M (2010) Rifle criteria for acute kidney dysfunction following liver transplantation: incidence and risk factors. Transplant Proc 42(10):4171–4174. doi:10.1016/j.transproceed.2010.09.137
Hwang SH, Jeong MH, Ahmed K, Kim MC, Cho KH, Lee MG, Ko JS, Park KH, Sim DS, Yoon NS, Yoon HJ, Kim KH, Hong YJ, Park HW, Kim JH, Ahn YK, Cho JG, Park JC, Kang JC (2011) Different clinical outcomes of acute kidney injury according to acute kidney injury network criteria in patients between ST elevation and non-ST elevation myocardial infarction. Int J Cardiol 150(1):99–101. doi:10.1016/j.ijcard.2011.03.039
Marenzi G, Cabiati A, Bertoli SV, Assanelli E, Marana I, De Metrio M, Rubino M, Moltrasio M, Grazi M, Campodonico J, Milazzo V, Veglia F, Lauri G, Bartorelli AL (2013) Incidence and relevance of acute kidney injury in patients hospitalized with acute coronary syndromes. Am J Cardiol 111(6):816–822. doi:10.1016/j.amjcard.2012.11.046
Quintavalle C, Fiore D, De Micco F, Visconti G, Focaccio A, Golia B, Ricciardelli B, Donnarumma E, Bianco A, Zabatta MA, Troncone G, Colombo A, Briguori C, Condorelli G (2012) Impact of a high loading dose of atorvastatin on contrast-induced acute kidney injury. Circulation 126(25):3008–3016. doi:10.1161/CIRCULATIONAHA.112.103317
Zhao JL, Yang YJ, Zhang YH, You SJ, Wu YJ, Gao RL (2008) Effect of statins on contrast-induced nephropathy in patients with acute myocardial infarction treated with primary angioplasty. Int J Cardiol 126(3):435–436. doi:10.1016/j.ijcard.2007.01.123
Ueda H, Yamada T, Masuda M, Okuyama Y, Morita T, Furukawa Y, Koji T, Iwasaki Y, Okada T, Kawasaki M, Kuramoto Y, Naito T, Fujimoto T, Komuro I, Fukunami M (2011) Prevention of contrast-induced nephropathy by bolus injection of sodium bicarbonate in patients with chronic kidney disease undergoing emergent coronary procedures. Am J Cardiol 107(8):1163–1167. doi:10.1016/j.amjcard.2010.12.012
Gassanov N, Nia AM, Caglayan E, Er F (2013) Remote ischemic preconditioning and renoprotection: from myth to a novel therapeutic option? J Am Soc Nephrol. doi:10.1681/ASN.2013070708
Hausenloy DJ, Candilio L, Laing C, Kunst G, Pepper J, Kolvekar S, Evans R, Robertson S, Knight R, Ariti C, Clayton T, Yellon DM, Investigators ET (2012) Effect of remote ischemic preconditioning on clinical outcomes in patients undergoing coronary artery bypass graft surgery (ERICCA): rationale and study design of a multi-centre randomized double-blinded controlled clinical trial. Clin Res Cardiol 101(5):339–348. doi:10.1007/s00392-011-0397-x
Bell RM, Rear R, Cunningham J, Dawnay A, Yellon DM (2013) Effect of remote ischaemic conditioning on contrast-induced nephropathy in patients undergoing elective coronary angiography (ERICCIN): rationale and study design of a randomised single-centre, double-blind placebo-controlled trial. Clin Res Cardiol. doi:10.1007/s00392-013-0637-3
Er F, Nia AM, Dopp H, Hellmich M, Dahlem KM, Caglayan E, Kubacki T, Benzing T, Erdmann E, Burst V, Gassanov N (2012) Ischemic preconditioning for prevention of contrast medium-induced nephropathy: randomized pilot RenPro Trial (Renal Protection Trial). Circulation 126(3):296–303. doi:10.1161/CIRCULATIONAHA.112.096370
Botker HE, Kharbanda R, Schmidt MR, Bottcher M, Kaltoft AK, Terkelsen CJ, Munk K, Andersen NH, Hansen TM, Trautner S, Lassen JF, Christiansen EH, Krusell LR, Kristensen SD, Thuesen L, Nielsen SS, Rehling M, Sorensen HT, Redington AN, Nielsen TT (2010) Remote ischaemic conditioning before hospital admission, as a complement to angioplasty, and effect on myocardial salvage in patients with acute myocardial infarction: a randomised trial. Lancet 375(9716):727–734. doi:10.1016/S0140-6736(09)62001-8
James MT, Samuel SM, Manning MA, Tonelli M, Ghali WA, Faris P, Knudtson ML, Pannu N, Hemmelgarn BR (2013) Contrast-induced acute kidney injury and risk of adverse clinical outcomes after coronary angiography: a systematic review and meta-analysis. Circ Cardiovasc Interv 6(1):37–43. doi:10.1161/CIRCINTERVENTIONS.112.974493
Gurm HS, Dixon SR, Smith DE, Share D, Lalonde T, Greenbaum A, Moscucci M, Registry BMC (2011) Renal function-based contrast dosing to define safe limits of radiographic contrast media in patients undergoing percutaneous coronary interventions. J Am Coll Cardiol 58(9):907–914. doi:10.1016/j.jacc.2011.05.023
Tehrani S, Laing C, Yellon DM, Hausenloy DJ (2013) Contrast-induced acute kidney injury following PCI. Eur J Clin Invest 43(5):483–490. doi:10.1111/eci.12061
Seeliger E, Sendeski M, Rihal CS, Persson PB (2012) Contrast-induced kidney injury: mechanisms, risk factors, and prevention. Eur Heart J 33(16):2007–2015. doi:10.1093/eurheartj/ehr494
Newby LK, Rutsch WR, Califf RM, Simoons ML, Aylward PE, Armstrong PW, Woodlief LH, Lee KL, Topol EJ, Van de Werf F (1996) Time from symptom onset to treatment and outcomes after thrombolytic therapy. GUSTO-1 Investigators. J Am Coll Cardiol 27(7):1646–1655
Cannon CP, Gibson CM, Lambrew CT, Shoultz DA, Levy D, French WJ, Gore JM, Weaver WD, Rogers WJ, Tiefenbrunn AJ (2000) Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA, J Am Med Assoc 283(22):2941–2947
Bradley EH, Nallamothu BK, Herrin J, Ting HH, Stern AF, Nembhard IM, Yuan CT, Green JC, Kline-Rogers E, Wang Y, Curtis JP, Webster TR, Masoudi FA, Fonarow GC, Brush JE Jr, Krumholz HM (2009) National efforts to improve door-to-balloon time results from the door-to-balloon alliance. J Am Coll Cardiol 54(25):2423–2429. doi:10.1016/j.jacc.2009.11.003
Reimer KA, Lowe JE, Rasmussen MM, Jennings RB (1977) The wavefront phenomenon of ischemic cell death. 1. Myocardial infarct size vs duration of coronary occlusion in dogs. Circulation 56(5):786–794
Hasche ET, Fernandes C, Freedman SB, Jeremy RW (1995) Relation between ischemia time, infarct size, and left ventricular function in humans. Circulation 92(4):710–719
de Waha S, Eitel I, Desch S, Fuernau G, Lurz P, Haznedar D, Grothoff M, Gutberlet M, Schuler G, Thiele H (2012) Time-dependency, predictors and clinical impact of infarct transmurality assessed by magnetic resonance imaging in patients with ST-elevation myocardial infarction reperfused by primary coronary percutaneous intervention. Clin Res Cardiol 101(3):191–200. doi:10.1007/s00392-011-0380-6
Shacham Y, Leshem-Rubinow E, Ben-Assa E, Roth A, Steinvil A (2013) Lower admission hemoglobin levels are associated with longer symptom duration in acute ST-elevation myocardial infarction. Clin Cardiol. doi:10.1002/clc.22215
Financial disclosure
None.
Conflict of interest
None on the part of any author.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shacham, Y., Leshem-Rubinow, E., Steinvil, A. et al. Renal impairment according to acute kidney injury network criteria among ST elevation myocardial infarction patients undergoing primary percutaneous intervention: a retrospective observational study. Clin Res Cardiol 103, 525–532 (2014). https://doi.org/10.1007/s00392-014-0680-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-014-0680-8