Abstract
Acute kidney injury is a frequent complication among ST segment elevation myocardial infarction (STEMI) patients undergoing primary percutaneous coronary intervention (PCI), and is associated with adverse outcomes. While contrast nephropathy is considered the most important reason for worsening of renal function, recent data have suggested the role of other important factors among this specific patient population. In the present review, we examine the various factors leading to renal impairment in STEMI patients and place the findings in the context of this specific patient population in the era of primary PCI. These factors include contrast nephropathy, time to coronary reperfusion, cardiac pump function and hemodynamics as well as various inflammatory and metabolic markers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
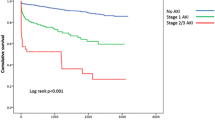
Among ST segment elevation myocardial infarction (STEMI) patients undergoing primary percutaneous coronary intervention (PCI) worsening of renal function resulting in acute kidney injury (AKI) is a frequent complication, known to be associated with adverse outcomes [1–4]. The worsening of renal function throughout the hospitalization period in STEMI patients is multifactorial, though the most important reason is considered contrast-induced AKI, related mainly to the amount and type of contrast material and to preprocedural renal function [5–7]. A growing amount of data now suggests that AKI, in this clinical scenario, has a complex and multifactorial pathogenesis which goes beyond the administration of contrast volume during catheterization. These factors include an adverse hemodynamic state resulting in reduced renal perfusion, other metabolic factors such as drugs administered (especially blockers of the renin-angiotensin axis) as well as the occurrence in parallel of sepsis, bleeding, atheroembolic disease and acute hyperglycemia [8–10] (Fig. 1). In the present review we describe the various factors associated with AKI in this specific patient population, including new novel theories. We hope that this will aid physicians in a better awareness of those at risk for this complication, enabling the implementation of both primary and secondary preventive measures.
Contrast-induced nephropathy
Contrast-induced acute kidney injury (CI-AKI) is a prevalent and deleterious complication of coronary angiography. CI-AKI has been reported to be the third most common cause of hospital-acquired renal failure [11]. The risk of CI-AKI is directly associated with increasing contrast media volume [6]. The incidence of CI-AKI ranges from 2 % in patients with normal baseline renal function to as high as 20–30 % in patients with a baseline creatinine >2.0 mg/dl [12]. Even after adjusting for baseline renal function and comorbidities, in-hospital mortality is about fivefold higher in patients with CI-AKI, and 1-year and 5-year mortality rates are about fourfold higher [13]. The average amount of contrast volume used in primary PCI has been reported to be higher than in elective PCI [14]. In addition, the contrast volume/estimated glomerular filtration rate (eGFR) ratio was recently shown to predict AKI among patients undergoing primary PCI [15, 16].
Time to reperfusion
Recent data suggest an association between longer time to reperfusion and CI-AKI in patients undergoing primary PCI [17]. Time to coronary reperfusion is a powerful prognostic marker in STEMI patients [18, 19] and major efforts are devoted to minimizing the total ischemic duration in order to improve survival following STEMI [20]. The sudden myocardial insult in STEMI often results in an acute reduction of cardiac output. This early hemodynamic deterioration may theoretically lead to reduced renal perfusion and consequently to kidney injury. Bradycardia or tachycardia in the acute STEMI setting can have similar hemodynamic effects. Short renal hypoperfusion is often associated with a prerenal failure, defined as a reversible loss of renal function without structural damage [21]. A more profound and prolonged hypoperfusion primarily affects the function and structure of tubular epithelial cells and, in severe cases, this is characterized by epithelial cell ischemia and necrosis. Nevertheless, ischemia-related injury does not exclusively lead to alterations of epithelial cell function and structure but also causes interstitial inflammation and interstitial microvasculopathy [22–24]. In contrast to prerenal injury, these alterations can result in irreversible loss or delayed restoration of renal function, and may increase susceptibility to CI-AKI. In addition, longer symptom duration prior to hospital admission is associated with higher admission C-reactive protein and lower hemoglobin levels in STEMI patients [25], both demonstrated to be associated with increased risk for AKI in STEMI patients. It appears that, in addition to the well-known fact that “time is myocardium” among STEMI patients, one might also say that “time is kidney”.
Cardiac pump function and hemodynamics
Among the eight different risk factors included in the current most widely applied score to estimate the risk of CI-AKI [26], three (hypotension, congestive heart failure, and intra-aortic balloon pump) are directly related to cardiac pump function and to acute hemodynamic deterioration. This score was also validated recently among STEMI patients undergoing primary PCI [27]. A report by Marenzi et al. demonstrated that among STEMI patients undergoing PCI, age, anterior infarct location, contrast agent volume, time to reperfusion >6 h, and use of intraaortic balloon were independent predictors of CI-AKI. These factors were used to build a specific score which demonstrated a graded increase in CI-AKI incidence as well as in-hospital mortality as the risk score increased [28]. Both scores (Mehran’s and Marenzi’s) have been recently assessed in a HORIZONS-AMI sub-study of STEMI patients undergoing primary PCI, where CI-AKI was shown to be associated with adverse short- and long-term outcomes [14]. Similarly, in a recent study published by our group, STEMI patients developing AKI were more likely to be at a critical state and to sustain significant arrhythmias and congestive heart failure episodes in addition to lower left ventricular ejection fraction [29]. We also demonstrated that every 1 % reduction in left ventricular ejection fraction was associated with a 10 % increase in the risk AKI [30]. Following the resumption of coronary flow and the improvement of left ventricular function as well as the resolution of arrhythmias, hemodynamic impairment often resolves although renal function may still remain impaired or lag behind in recovery.
Inflammatory and metabolic markers
Several metabolic markers have been postulated to play a role in the development of AKI in STEMI patients.
C-reactive protein
The ischemic injury and myocardial necrosis following a STEMI incite an acute inflammatory response. Among the various pro-inflammatory cytokines, high sensitive C-reactive protein (hs-CRP) has emerged as a powerful and independent predictor of heart failure and long-term mortality [31]. Elevated periprocedural hs-CRP was shown to be associated with an increased risk for AKI in non-MI patients undergoing PCI [32]. A recent study demonstrated that among STEMI patients, admission hs-CRP level is an independent risk factor for AKI [33]. There is convincing evidence that the elevation of the serum hs-CRP level in STEMI patients may not be just an epiphenomenon, but rather may directly contribute to the inflammatory state. hs-CRP can directly activate the clotting system [34], and mediate enhanced expression of adhesion molecules, reduced nitric oxide production and impairment of antioxidant defenses [35] resulting in endothelial dysfunction. Endothelial dysfunction and decreased activity of renal vasodilators has been regarded as an important contributor to AKI development [36]. Thus, it is possible that elevated peri-PCI hs-CRP levels are not only a marker for AKI, but may also make kidneys more vulnerable to contrast-induced damage.
Admission glucose
Hyperglycemia is common in patients with STEMI, even in the absence of a history of diabetes mellitus (DM), and has been identified as a major independent predictor of both in-hospital congestive heart failure and mortality in STEMI [37, 38]. Recent evidence demonstrated that acute hyperglycemia was also associated with increased risk for contrast-induced nephropathy following primary PCI [10, 39, 40]. Hyperglycemia may represent an epiphenomenon of the stress response, mediated by cortisol and catecholamines whose release is elicited by the hemodynamic compromise or myocardial damage. Hyperglycemia may, however, exert a direct negative impact on renal function. The outer medullary region is particularly susceptible to ischemic injury because of its high metabolic activity and low prevailing oxygen tension [41]. The partial oxygen pressure of the outer medulla in the kidney is very low during normal function. Contrast media aggravates hypoxic injury to this region by increasing renal vascular resistance [42]. Hyperglycemia may lead to increased production of oxygen free radicals with increased oxidative stress and suppressed flow-mediated vasodilatation, inducing medullary hypoxia and ischemia, thus exacerbating the deleterious effect of contrast material [43, 44]. Furthermore, acute hyperglycemia may induce osmotic diuresis, resulting in volume depletion and increasing the risk for pre-renal azotemia and contrast toxicity. Patients with hyperglycemia also exhibit more metabolic abnormalities in the background that can lead to higher inflammatory biomarkers [44].
Admission anemia
Previous studies have shown that anemia increases the risk of CI-AKI in various patient populations [45–47]. Contrast media could increase oxygen affinity of hemoglobin, so oxygen delivery to the peripheral tissues might be impaired [42]. Local renal hypoxia can therefore be aggravated among patients with low hemoglobin levels after exposure to contrast media; hence, the combination of contrast-induced vasoconstriction and anemia may decrease oxygen delivery, sufficiently to cause renal medullary hypoxia. The presence of anemia in the acute STEMI setting can thus further aggravate the ischemic insult to the kidney, resulting in greater susceptibility to AKI [48].
Hyperuricemia
Previous studies have shown that elevated uric acid levels increase the risk of AKI in patients undergoing cardiac surgery [49, 50] and non-emergent PCI [51]. Elevated serum uric acid levels were also associated with increased short- and long-term mortality among myocardial infarction patients [52–55]. A report by Park et al. demonstrated that, among patients undergoing PCI, patients with AKI had higher uric acid levels, and that uric acid was independently associated with the risk for AKI [51]. Hyperuricemia inhibits the nitric oxide system in the kidneys and increases endothelin-1 concentrations, resulting in loss of renal blood flow autoregulation, renal vasoconstriction and reduced medullary blood flow [56]. Hyperuricemia has also been shown to stimulate the expression of C-reactive protein and induces the infiltration of inflammatory cells into the renal parenchyma with resultant tissue injury [57]. Elevated uric acid levels may thus reduce renal perfusion, exacerbating ischemia/reperfusion injury, further aggravating the ischemic insult to the kidney, with the result of greater susceptibility to AKI.
Bleeding complications
Anemia is known to be an independent predictor of CI-AKI [45, 46] being one of the main variables of the Mehran contrast-induced nephropathy risk score [26]. However, few previous studies or risk score models have accounted for periprocedural bleeding as a risk factor for the development of CI-AKI. A recent report demonstrated that, among patients undergoing PCI, those who experienced periprocedural bleeding had a higher likelihood of developing CI-AKI, and CI-AKI incidence correlated closely with bleeding severity [58]. It also appears that the transradial approach is also associated with a lower rate of occurrence of both acute and chronic renal dysfunction following PCI, when compared to the transfemoral approach, a fact which could be attributed at least in part, to the lower bleeding risk associated with the radial puncture [58, 59].
Conclusion
Among STEMI patients undergoing primary PCI, AKI is complex and should not be assumed to be solely due to contrast media. Hemodynamic abnormalities representing a special type of acute cardio-renal syndrome and various metabolic factors should be considered when evaluating the risk for this complication.
References
Shacham Y, Leshem-Rubinow E, Steinvil A, Assa EB, Keren G, Roth A, Arbel Y (2014) Renal impairment according to acute kidney injury network criteria among ST elevation myocardial infarction patients undergoing primary percutaneous intervention: a retrospective observational study. Clin Res Cardiol 103:525–532
Watabe H, Sato A, Hoshi T, Takeyasu N, Abe D, Akiyama D, Kakefuda Y, Nishina H, Noguchi Y, Aonuma K (2014) Association of contrast-induced acute kidney injury with long-term cardiovascular events in acute coronary syndrome patients with chronic kidney disease undergoing emergent percutaneous coronary intervention. Int J Cardiol 174:57–63
Parikh CR, Coca SG, Wang Y, Masoudi FA, Krumholz HM (2008) Long-term prognosis of acute kidney injury after acute myocardial infarction. Arch Intern Med 168:987–995
Marenzi G, Cosentino N, Guastoni C (2015) How to balance risks and benefits in the management of CKD patients with coronary artery disease. J Nephrol 28:403–413
Giacoppo D, Madhavan MV, Baber U, Warren J, Bansilal S, Witzenbichler B, Dangas GD, Kirtane AJ, Xu K, Kornowski R, Brener SJ, Généreux P, Stone GW, Mehran R (2015) Impact of contrast-induced acute kidney injury after percutaneous coronary intervention on short- and long-term outcomes: pooled analysis from the HORIZONS-AMI and ACUITY trials. Circ Cardiovasc Interv. doi:10.1161/114.002475
Cruz DN (2013) Cardiorenal syndrome in critical care: The acute cardiorenal and renocardiac syndromes. Adv Chron Kidney Dis 20:56–66
Arbel Y, Halkin A, Finkelstein A, Revivo M, Berliner S, Herz I, Keren G, Banai S (2013) Impact of estimated glomerular filtration rate on vascular disease extent and adverse cardiovascular events in patients without chronic kidney disease. Can J Card 29:1374–1381
Marenzi G, Cosentino N, Bartorelli AL (2015) Acute kidney injury in patients with acute coronary syndromes. Heart. doi:10.1136/307773
Marenzi G, Assanelli E, Campodonico J, Lauri G, Marana I, De Metrio M, Moltrasio M, Grazi M, Rubino M, Veglia F, Fabbiocchi F, Bartorelli AL (2009) Contrast volume during primary percutaneous coronary intervention and subsequent contrast-induced nephropathy and mortality. Ann Intern Med 150:170–177
Marenzi G, De Metrio M, Rubino M, Lauri G, Cavallero A, Assanelli E, Grazi M, Moltrasio M, Marana I, Campodonico J, Discacciati A, Veglia F, Bartorelli AL (2010) Acute hyperglycemia and contrast-induced nephropathy in primary percutaneous coronary intervention. Am Heart J 160:1170–1177
James MT, Samuel SM, Manning MA, Tonelli M, Ghali WA, Faris P, Knudtson ML, Pannu N, Hammelgarn BR (2013) Contrast-induced acute kidney injury and risk of adverse clinical outcomes after coronary angiography: a systematic review and meta-analysis. Circ Cardiovasc Interv 6:37–43
Tehrani S, Laing C, Yellon DM, Hausenloy DJ (2013) Contrast-induced acute kidney injury following PCI. Eur J Clin Invest 43:483–490
Seeliger E, Sendeski M, Rihal CS, Persson PB (2012) Contrast-induced kidney injury: mechanisms, risk factors, and prevention. Eur Heart J 33:2007–2015
Narula A, Mehran R, Weisz G, Dangas GD, Yu J, Généreux P, Nikolsky E, Brener SJ, Witzenbichler B, Guagliumi G, Clark AE, Fahy M, Xu K, Brodie BR, Stone GW (2014) Contrast-induced acute kidney injury after primary percutaneous coronary intervention: results from the HORIZONS-AMI substudy. Eur Heart J 35:1533–1540
Gurm HS, Dixon SR, Smith DE, Share D, Lalonde T, Greenbaum A, Moscucci M (2011) Renal function-based contrast dosing to define safe limits of radiographic contrast media in patients undergoing percutaneous coronary interventions. J Am Coll Cardiol 58:907–914
Mager A, Vaknin Assa H, Lev EI, Bental T, Assali A, Kornowski R (2011) The ratio of contrast volume to glomerular filtration rate predicts outcomes after percutaneous coronary intervention for ST-segment elevation acute myocardial infarction. Catheter Cardiovasc Interv 78:198–201
Shacham Y, Leshem-Rubinow E, Gal-Oz A, Arbel Y, Keren G, Roth A, Steinvil A (2014) Relation of time to coronary reperfusion and the development of acute kidney injury after ST-segment elevation myocardial infarction. Am J Cardiol 114:131–135
Newby LK, Rutsch WR, Califf RM, Simoons ML, Aylward PE, Armstrong PW, Woodlief LH, Lee KL, Topol EJ, Van de Werf F (1996) Time from symptom onset to treatment and outcomes after thrombolytic therapy. GUSTO-1 Investigators. J Am Coll Cardiol 27:1646–1655
Cannon CP, Gibson CM, Lambrew CT, Shoultz DA, Levy D, French WJ, Gore JM, Weaver WD, Rogers WJ, Tiefenbrunn AJ (2000) Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA 283:2941–2947
Bradley EH, Nallamothu BK, Herrin J, Ting HH, Stern AF, Nembhard IM, Yuan CT, Green JC, Kline-Rogers E, Wang Y, Curtis JP, Webster TR, Masoudi FA, Fonarow GC, Brush JE Jr, Krumholz HM (2009) National efforts to improve door-to-balloon time results from the door-to-balloon alliance. J Am Coll Cardiol 54:2423–2429
Devarajan P (2006) Update on mechanisms of ischemic acute kidney injury. J Am Soc Nephrol 17:1503–1520
Chertow GM, Burdick E, Honour M, Bonventre JV, Bates DW (2005) Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol 16:3365–3370
Lameire N, Van Biesen W, Vanholder R (2005) Acute renal failure. Lancet 365:417–430
Schrier RW, Wang W, Poole B, Mitra A (2004) Acute renal failure: definitions, diagnosis, pathogenesis, and therapy. J Clin Invest 114:5–14
Shacham Y, Leshem-Rubinow E, Ben-Assa E, Roth A, Steinvil A (2014) Lower admission hemoglobin levels are associated with longer symptom duration in acute ST-elevation myocardial infarction. Clin Cardiol 37:73–77
Mehran R, Aymong ED, Nikolsky E, Lasic Z, Iakovou I, Fahy M, Mintz GS, Lansky AJ, Moses JW, Stone GW, Leon MB, Dangas G (2004) A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: development and initial validation. J Am Coll Cardiol 44:1393–1399
Wi J, Ko YG, Kim JS, Kim BK, Choi D, Ha JW, Hong MK, Jang Y (2011) Impact of contrast-induced acute kidney injury with transient or persistent renal dysfunction on long-term outcomes of patients with acute myocardial infarction undergoing percutaneous coronary intervention. Heart 97:1753–1757
Marenzi G, Lauri G, Assanelli E, Campodonico J, De Metrio M, Marana I, Grazi M, Veglia F, Bartorelli AL (2004) Contrast-induced nephropathy in patients undergoing primary angioplasty for acute myocardial infarction. J Am Coll Cardiol 44:1780–1785
Shacham Y, Leshem-Rubinow E, Gal-Oz A, Arbel Y, Keren G, Roth A, Steinvil A (2015) Acute cardio-renal syndrome as a cause for renal deterioration among myocardial infarction patients treated by primary percutaneous intervention. Can J Cardiol 31:1240–1244
Shacham Y, Leshem-Rubinow E, Gal-Oz A, Topilsky Y, Steinvil A, Keren G, Roth A, Arbel Y (2014) Association of left ventricular function and acute kidney injury among ST-elevation myocardial infarction patients treated by primary percutaneous intervention. Am J Cardiol 115:293–297
Suleiman M, Khatib R, Agmon Y, Mahamid R, Boulos M, Kapeliovich M, Levy Y, Beyar R, Markiewicz W, Hammerman H, Aronson D (2006) Early inflammation and risk of long-term development of heart failure and mortality in survivors of acute myocardial infarction predictive role of C-reactive protein. J Am Coll Cardiol 47:962–968
Gao F, Zhou YJ, Zhu X, Wang ZJ, Yang SW, Shen H (2011) C-reactive protein and the risk of contrast-induced acute kidney injury in patients undergoing percutaneous coronary intervention. Am J Nephrol 34:203–210
Shacham Y, Leshem-Rubinow E, Steinvil A, Keren G, Roth A, Arbel Y (2015) High sensitive C-reactive protein and the risk of acute kidney injury among ST elevation myocardial infarction patients undergoing primary percutaneous intervention. Clin Exp Nephrol 19:838–843
Cermak J, Key NS, Bach RR, Balla J, Jacob HS, Vercellotti GM (1993) C-reactive protein induces human peripheral blood monocytes to synthesize tissue factor. Blood 82:513–520
Fujii H, Li SH, Szmitko PE, Fedak PW, Verma S (2006) C-reactive protein alters antioxidant defenses and promotes apoptosis in endothelial progenitor cells. Arterioscler Thromb Vasc Biol 26:2476–2482
Russo D, Minutolo R, Cianciaruso B, Memoli B, Conte G, De Nicola L (1995) Early effects of contrast media on renal hemodynamics and tubular function in chronic renal failure. J Am Soc Nephrol 6:1451–1458
Timmer JR, Hoekstra M, Nijsten MW, van der Horst IC, Ottervanger JP, Slingerland RJ, Dambrink JH, Bilo HJ, Zijlstra F, van’t Hof AW (2011) Prognostic value of admission glycosylated hemoglobin and glucose in nondiabetic patients with ST-segment-elevation myocardial infarction treated with percutaneous coronary intervention. Circulation 124:704–711
Goyal A, Mehta SR, Gerstein HC, Diaz R, Afzal R, Xavier D, Zhu J, Pais P, Lisheng L, Kazmi KA, Zubaid M, Piegas LS, Widimsky P, Budaj A, Avezum A, Yusuf S (2009) Glucose levels compared with diabetes history in the risk assessment of patients with acute myocardial infarction. Am Heart J 157:763–770
Moriyama N, Ishihara M, Noguchi T, Nakanishi M, Arakawa T, Asaumi Y, Kumasaka L, Kanaya T, Miyagi T, Nagai T, Yamane T, Fujino M, Honda S, Fujiwara R, Anzai T, Kusano K, Goto Y, Yasuda S, Ogawa H (2014) Admission hyperglycemia is an independent predictor of acute kidney injury in patients with acute myocardial infarction. Circ J 78:1475–1480
Shacham Y, Gal-Oz A, Leshem-Rubinow E, Arbel Y, Keren G, Roth A, Steinvil A (2015) Admission glucose levels and the risk of acute kidney injury in nondiabetic ST segment elevation myocardial infarction patients undergoing primary percutaneous coronary intervention. Cardiorenal Med 5:191–198
Persson PB, Patzak A (2005) Renal haemodynamic alterations in contrast medium-induced nephropathy and the benefit of hydration. Nephrol Dial Transpl 20(Suppl 1):i2–i5
Kim SJ, Salem MR, Joseph NJ, Madayag MA, Cavallino RP, Crystal GJ (1990) Contrast media adversely affect oxyhemoglobin dissociation. Anesth Analg 71:73–76
Kawano H, Motoyama T, Hirashima O, Hirai N, Miyao Y, Sakamoto T, Kugiyama K, Ogawa H, Yasue H (1999) Hyperglycemia rapidly suppresses flow-mediated endothelium-dependent vasodilation of brachial artery. J Am Coll Cardiol 34:146–154
Arbel Y, Shmueli H, Halkin A, Berliner S, Shapira I, Herz I, Havakuk O, Shacham Y, Rabinovich I, Keren G, Finkelstein A, Banai S (2014) Hyperglycemia in patients referred for cardiac catheterization is associated with preexisting diabetes rather than a stress-related phenomenon: a prospective cross-sectional study. Clin Cardiol 37:479–484
Nikolsky E, Mehran R, Lasic Z, Mintz GS, Lansky AJ, Na Y, Pocock S, Negoita M, Moussa I, Stone GW, Moses JW, Leon MB, Dangas G (2005) Low hematocrit predicts contrast-induced nephropathy after percutaneous coronary interventions. Kidney Int 67:706–713
Dangas G, Iakovou I, Nikolsky E, Aymong ED, Mintz GS, Kipshidze NN, Lansky AJ, Moussa I, Stone GW, Moses JW, Leon MB, Mehran R (2005) Contrast-induced nephropathy after percutaneous coronary interventions in relation to chronic kidney disease and hemodynamic variables. Am J Cardiol 95:13–19
Murakami R, Kumita S, Hayashi H, Sugizaki K, Okazaki E, Kiriyama T, Hakozaki K, Tani H, Miki I, Takeda M (2013) Anemia and the risk of contrast-induced nephropathy in patients with renal insufficiency undergoing contrast-enhanced mdct. Eur J Radiol 82:e521–e524
Shacham Y, Gal-Oz A, Leshem-Rubinow E, Arbel Y, Keren G, Roth A, Steinvil A (2015) Association of admission hemoglobin levels and acute kidney injury among myocardial infarction patients treated with primary percutaneous intervention. Can J Cardiol 31:50–55
Ejaz AA, Beaver TM, Shimada M, Sood P, Lingegowda V, Schold JD, Kim T, Johnson RJ (2009) Uric acid: a novel risk factor for acute kidney injury in high-risk cardiac surgery patients? Am J Nephrol 30:425–429
Lapsia V, Johnson RJ, Dass B, Shimada M, Kambhampati G, Ejaz NI, Arif AA, Ejaz AA (2012) Elevated uric acid increases the risk for acute kidney injury. Am J Med 125:302e9–17
Park SH, Shin WY, Lee EY, Gil HW, Lee SW, Lee SJ, Jin DK, Hong SY (2011) The impact of hyperuricemia on in-hospital mortality and incidence of acute kidney injury in patients undergoing percutaneous coronary intervention. Circ J 75:692–697
Kojima S, Sakamoto T, Ishihara M, Kimura K, Miyazaki S, Yamagishi M, Tei C, Hiraoka H, Sonoda M, Tsuchihashi K, Shimoyama N, Honda T, Ogata Y, Matsui K, Ogawa H (2005) Prognostic usefulness of serum uric acid after acute myocardial infarction (the Japanese acute coronary syndrome study). Am J Cardiol 96:489–495
Lazzeri C, Valente S, Chiostri M, Sori A, Bernardo P, Gensini GF (2010) Uric acid in the acute phase of ST elevation myocardial infarction submitted to primary PCI: its prognostic role and relation with inflammatory markers: a single center experience. Int J Cardiol 138:206–209
Lazzeri C, Valente S, Chiostri M, Picariello C, Gensini GF (2012) Uric acid in the early risk stratification of ST-elevation myocardial infarction. Intern Emerg Med 7:33–39
Kowalczyk J, Francuz P, Swoboda R, Lenarczyk R, Sredniawa B, Golda A, Kurek T, Mazurek M, Podolecki T, Polonski L, Kalarus Z (2010) Prognostic significance of hyperuricemia in patients with different types of renal dysfunction and acute myocardial infarction treated with percutaneous coronary intervention. Nephron Clin Pract 116:c114–c122
Ejaz AA, Mu W, Kang DH, Roncal C, Sautin YY, Henderson G, Tabah-Fisch I, Keller B, Beaver TM, Nakagawa T, Johnson RJ (2007) Could uric acid have a role in acute renal failure? Clin J Am Soc Nephrol 2:16–21
Kang DH, Park SK, Lee IK, Johnson RJ (2005) Uric acid-induced C-reactive protein expression: implication on cell proliferation and nitric oxide production of human vascular cells. J Am Soc Nephrol 16:3553–3562
Ohno Y, Maekawa Y, Miyata H, Inoue S, Ishikawa S, Sueyoshi K, Noma S, Kawamura A, Kohsaka S, Fukuda K (2013) Impact of Periprocedural bleeding on incidence of contrast-induced acute kidney injury in patients treated with percutaneous coronary intervention. J Am Coll Cardiol 62:1260–1266
Vuurmans T, Byrne J, Fretz E, Janssen C, Hilton JD, Klinke WP, Djurdjev O, Levin A (2010) Chronic kidney injury in patients after cardiac catheterisation or percutaneous coronary intervention: a comparison of radial and femoral approaches (from the British Columbia cardiac and renal registries). Heart 96:1538–1542
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None on the part of any author.
Ethical standard
The research did not involve human participants and/or animals.
Rights and permissions
About this article
Cite this article
Shacham, Y., Steinvil, A. & Arbel, Y. Acute kidney injury among ST elevation myocardial infarction patients treated by primary percutaneous coronary intervention: a multifactorial entity. J Nephrol 29, 169–174 (2016). https://doi.org/10.1007/s40620-015-0255-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-015-0255-4